Prevalence, Severity, and Co-occurrence of Chronic Physical Health Problems of Persons With Serious Mental Illness
Abstract
OBJECTIVES: This study examined Medicaid claims forms to determine the prevalence, severity, and co-occurrence of physical illness within a representative sample of persons with serious mental illness (N=147). METHODS: Representativeness of health problems in the study sample was established through comparison with a larger sample of persons with serious mental illness enrolled in Medicaid within the same state. Standardized annual costs were then assigned to Medicaid claims diagnoses, and individual health problem severity was measured as the sum of estimated treatment costs for diagnosed conditions. RESULTS: Seventy-four percent of the study sample (N=109) had been given a diagnosis of at least one chronic health problem, and 50 percent (N=73) had been given a diagnosis of two or more chronic health problems. Of the 14 chronic health conditions surveyed, chronic pulmonary illness was the most prevalent (31 percent incidence) and the most comorbid. Persons with chronic pulmonary illness were second only to those with infectious diseases in average annual cost of treatment ($8,277). Also, 50 percent or more of participants in eight other diagnostic categories had chronic pulmonary illness. A regression analysis identified age, obesity, and substance use disorders as significant predictors of individual health problem severity. CONCLUSIONS: Risk adjustment for physical health is essential when setting performance standards or cost expectations for mental health treatment. Excluding persons with chronic health problems from mental health service evaluations restricts generalizability of research findings and may promote interventions that are inappropriate for many persons with serious mental illness.
Persons with serious mental illness tend to be in poorer physical health than persons without mental illness, especially in regard to obesity (1,2,3), cardiovascular (4,5,6,7,8) and gastrointestinal (8) disorders, diabetes (3,8,9), HIV (10,11), and both chronic (7,8) and acute (8) pulmonary disease. The high incidence of substance use disorders contributes to this overall poorer health (8,12,13,14).
However, little agreement exists as to which health conditions are the most prevalent within this population. Gastrointestinal, cardiovascular, metabolic, neurologic, and pulmonary diseases have each been ranked as being among the top five health problems by at least two research studies (8,12,15,16), but these studies did not agree as to the relative prevalence of these conditions. Variations in the diagnostic conditions chosen for study, and whether health conditions are acute or chronic, could account for differences in condition rank between prevalence studies. Variations in data source could also account for differences in reported prevalence ranks. Although Medicaid databases provide less information on individuals than research interviews, interview self-reports of substance use and psychiatric illness severity are less reliable than claims data (2,17). Our study measured the relative prevalence of chronic health conditions in a sample of adults with serious mental illness by adopting a standardized system of diagnostic classification that allowed a comparison of health condition ranks that were based on prevalence of ranks based on severity (estimated cost of treatment) and ranks that were based on co-occurrence of other chronic health conditions. We also estimated the extent of underreporting in our Medicaid claims data through a comparison with chronic health conditions documented in research interviews.
Methods
Overview
We first compared the characteristics of our sample of adults with serious mental illness (N=147) with those of a larger sample of adults with serious mental illness drawn from an epidemiologic study by Dickey and colleagues (8) (N=11,185) to estimate the extent to which our study findings would be generalizable. Both studies used data from Medicaid claims and drew their sample from Massachusetts. We then compared the health condition prevalence ranks of these two samples with those of a national sample of the general population that included approximately 250 million persons (18) to determine whether the Massachusetts population of adults with serious mental illness is unique in its ranking of health conditions. Finally, we conducted a descriptive analysis of chronic health conditions within our own sample to estimate the prevalence, co-occurrence of conditions, and severity (estimated cost of treatment) of chronic health conditions.
Study sample
Our study used data that were originally collected for a randomized controlled comparison of two psychiatric rehabilitation programs. The data were collected under the approval of the institutional review board of Fountain House, Inc., in New York City as part of the Employment Intervention Demonstration Project (19). Persons were eligible for the study (N=176) if they were aged 18 or older, did not have severe retardation (IQ greater than 60), were currently unemployed, and were given a primary DSM-IV diagnosis of a schizophrenia spectrum disorder, major depression, or bipolar disorder. We examined a subsample of this group consisting of those for whom Medicaid data from 1996 to 2000 were available and who resided in Massachusetts for at least two of these years or until the date of death (N=147). This Medicaid subsample did not differ significantly from the rest of the total sample on any background variable and was similar to the sample drawn from the large epidemiologic study by Dickey and colleagues (8). The mean±SD age of 38±10 years for our sample was comparable to the mean of 40±11 years for the sample from the larger study. In our study 79 participants, or 54 percent, were male, compared with 4,591 participants, or 41 percent, in the larger study. In our study 29 participants, or 20 percent, were from a racial or ethnic minority group, compared with 15 percent in the larger study. In our study 40 participants, or 27 percent, had Medicaid-documented substance use disorder, compared with 2,563 participants, or 23 percent, in the larger study. The only notable difference was in the prevalence of psychotic symptoms: the sample in the large epidemiologic study included only persons with psychotic disorders, whereas 84 percent (N=123) of our sample had documented psychotic symptoms.
Research measures
Background characteristics. Study variables included gender, age at project enrollment, race and ethnicity (Caucasian or from a racial or ethnic minority group), homelessness at any time between 1996 and 2000 (yes or no), and socioeconomic status (high or low), with high socioeconomic status defined as having a postsecondary education or having held a white collar or managerial job that lasted more than five years. Participants were coded as being obese if they had a Medicaid diagnosis of morbid obesity. They were coded as having a current, severe substance use disorder if they had any Medicaid claims for substance abuse treatment that lasted more than five days.
Psychiatric variables. Diagnostic eligibility was confirmed through recent clinical records or through the Structured Clinical Interview for DSM-IV (20), which was conducted by medical faculty of the department of psychiatry at the University of Massachusetts at Worcester. Psychiatric diagnosis was coded either as schizophrenia spectrum disorder or as bipolar disorder or major depression. Illness chronicity was measured as age at first psychiatric hospitalization.
Physical health measures
Medicaid data. Medicaid billing records from 1996 to 2000 were obtained from the Massachusetts Division of Medical Assistance after informed consent was acquired. The study and the informed consent forms were approved by the institutional review board. To restrict the data to confirmed diagnoses, we ignored diagnostic testing that was not followed by consultation or treatment and counted only diagnoses that involved two or more claims that extended for at least two weeks during any fiscal year. To avoid underreporting caused by the omission of annual checkups or infrequent treatment (21), we included single claims if they were repeated over any two or more of the four fiscal years of the current study.
The method that we used to rate the severity of physical health problems was based on the Chronic Illness and Disability Payment System (CDPS), which was developed by the University of California, San Diego (22). Average annual treatment costs that were derived from the CDPS multistate sample of Medicaid recipients (N=960,760) were assigned to diagnostic codes; groups of diagnoses were then ranked by cost, from extremely low to high, within 14 broad diagnostic categories that included cardiovascular, skeletal and connective tissue, nervous system, pulmonary, gastrointestinal, skin, renal, cancer, genital, metabolic, eye, and infectious diseases as well as diabetes and hematologic conditions. We omitted pregnancy, developmental disabilities, and cerebrovascular conditions from our analyses because each had an incidence of less than five cases. Physical health severity scores for each individual in our sample were calculated by summing the separate annual costs for each person's most costly diagnosis within each of the 14 categories.
Interview data. For the comparison of Medicaid data with interview data, we relied on clinician and consumer reports of a severe, current substance use disorder, morbid obesity, and chronic health conditions. Most self-reported health conditions were identified through a content analysis of interviewee responses to open-ended probes for the Positive and Negative Syndrome Scale (PANSS) (23). Because we did not use a checklist to document the absence of a condition, the reliability of interview reports cannot be ascertained. However, we assessed the completeness of Medicaid data by tracking whether the health conditions that were reported in interviews also appeared in the same participant's Medicaid claims.
Results
Sample representativeness
Table 1 shows the prevalence of health problems for three samples: a very large sample of the general population (approximately 250 million persons) from a study by the Centers for Disease Control and Prevention (CDC) (18), a sample of Medicaid enrollees with severe mental illness (N=11,185) from a large epidemiologic study by Dickey and colleagues (8), and our sample of Medicaid enrollees with severe mental illness (N=147). For the health problem categories we used seven chronic conditions that were targeted by the large epidemiologic study for which prevalence figures were also available from the CDC study and from our study. Because the three studies had varying time frames and because the percentages in the large epidemiologic study were adjusted for comparison with a control sample of Aid to Families With Dependent Children recipients, prevalence ranks rather than percentages should be compared.
As can be seen in Table 1, for the two samples of persons with severe mental illness, prevalence rankings are identical, and both samples differ from the national sample in the ranking of only one category, gastrointestinal disorders. Gastrointestinal disorders had the highest prevalence rank in both samples of persons with severe mental illness, whereas this health category ranked fourth in the national sample.
Chronic physical health problems
Prevalence and cost of treatment. Seventy-four percent (N=109) of our study sample was treated for one or more of the chronic health conditions listed in Table 2. Chronic pulmonary disease was the most prevalent health condition, and it was second in cost only to infectious diseases. Overall, there was wide variation in average annual costs (range, $175 to $4,200), which were measured as the average of estimated annual costs per person receiving a diagnosis. Average cost and prevalence of health conditions were uncorrelated, substantiating the independence of these two health measures.
Comorbid physical conditions. Fifty percent (N=73) of our sample was treated for two or more of the 14 conditions listed in Table 2. More than a third (N=46) were treated for three or more conditions, and a fifth (N=29) were treated for four or more conditions. Pulmonary disease was the most comorbid condition in our sample: 50 percent or more of participants with eight other health conditions were also treated for respiratory problems. Except for the pervasive co-occurrence of pulmonary disease and another disease, dual diagnoses of health conditions were diverse. Less than 50 percent of participants with gastrointestinal diseases, metabolic diseases, or diabetes had a co-occurring physical condition.
Health condition severity. A high correlation was found between each individual's estimated annual total cost of treatment (overall health problem severity) and total number of health conditions (r=.85, p<.001). Estimated average annual cost of treatment for individuals with chronic pulmonary disease (45 persons, or 31 percent) was four times that of a person without chronic pulmonary illness (102 persons, or 69 percent; mean of $8,277±$5,632 compared with a mean of $2,270±$2,713; t= 6.75, df=144, p<.001), even with an outlier of $40,000 omitted. Otherwise, estimated total cost per person across the 14 health categories was highly variable (mean of $4,315± $5,491).
Mortality. Eleven participants (6 percent) from the Massachusetts Employment Intervention Demonstration Project sample (N=176) died during the study period, seven of whom were in our Medicaid subsample (N=147). Dual diagnoses were very evident: five of the 11 deaths were due to pulmonary illness (lung cancer, chronic obstructive pulmonary disease, or pneumonia), and all five of these deaths were associated with a severe substance use disorder. Except for a single death that was caused by diabetes, the other six deaths were directly related to a substance use disorder (overdoses and drug-related murder), often with a co-occurring severe illness, such as AIDS. Ten of the 11 participants who died during the study were Caucasian and older than 35 years, and there was an even split in gender (five females and six males). Seven of the deceased had psychiatric diagnoses of bipolar disorder or major depression.
Correlations with background characteristics. By using estimated annual costs per condition as a measure of severity, we compared participants on eight background characteristics across the 14 CDPS diagnostic categories, with a moderately stringent threshold for statistical significance (p=.02). As Table 3 shows, participants who were treated for pulmonary disease were more likely to have been given a diagnosis of major depression or bipolar disorder than a diagnosis of schizophrenia, and they were more likely to have an active substance use problem. Infectious disease was also associated with a substance use disorder and with homelessness. Because 84 percent of persons who were homeless at any time during the project (16 of 19 participants) were treated for a substance use disorder, but only 40 percent of those with an active substance use disorder (16 of 40 participants) were homeless at any time during the project, substance use disorder may account for the greater incidence of infectious disease among participants who were homeless, but homelessness cannot account for the greater incidence of infectious disease among participants who had a substance use disorder.
Gender, obesity, and age were also predictive of health problems. Women had more metabolic (thyroid), skeletal and connective (arthritis), eye, and genital disorders than men. Also, obesity was associated with a higher incidence of both metabolic and gastrointestinal disorders. Age differences were also evident: only one participant younger than 33 years had a serious pulmonary disease, and no one older than 45 years had an infectious disease. One medical condition, cardiovascular disorders, showed a clear progressive increase across age groups for both hypertension and heart problems. Participants aged 45 through 75 years at baseline had higher rates of hypertension (11 participants, or 30 percent) than those aged 34 through 44 years (seven participants, or 11 percent) or those aged 18 through 33 years (three participants, or 6 percent) (p=.006). Likewise, participants aged 45 through 75 years at baseline also had more heart problems (ten participants, or 27 percent) than those aged 34 through 44 (six participants, or 10 percent) or those aged 18 through 33 (three participants, or 6 percent) (p=.011). No racial or ethnic differences were found in the prevalence of any health condition.
Predictors of health problem severity. As shown in Table 4, a regression analysis was conducted to identify personal characteristics that were predictive of health problem severity (standardized estimated annual treatment costs per person). The overall model was statistically significant, with age, substance use disorders, and obesity as significant predictors; the .05 level of significance (two-tailed test) was used. To test the robustness of these findings, the analysis was repeated with the inclusion of participants in the Massachusetts Employment Intervention Demonstration Project who were not Medicaid recipients (N=30). We used interview data to identify health problems, obesity, and substance use disorders for these additional participants. The new model was statistically significant (F=3.73, df=8, 164, p=.001; R2=.181; adjusted R2=.139), with the same significant covariates: age (B=.239; p=.002), obesity (B=.174, p=.024), and substance use disorder (B=.246, p=.006). Although substance use disorder, age, and obesity were not collinear, 30 percent of persons aged 45 or older at baseline in the Medicaid subsample (11 of 37 participants) and the total Massachusetts Employment Intervention Demonstration Project sample (12 of 42 participants) were both obese and had a substance use disorder.
Comparison of Medicaid claims data and interview data
Medicaid claims data either partially or fully confirmed 76 percent of interview reports of participants' health problems (84 of 110 participants) and 62 percent of interview reports of good health—that is, no claims for physical treatment (23 of 37 participants). There was an overall 73 percent (N=107) confirmation rate. The 76 percent confirmation of interview-reported health problems was paralleled by similar matches in the 70 percent range for a substance use disorder (40 of 55 participants, or 73 percent), morbid obesity (15 of 23 participants, or 65 percent), and pregnancy (five of six participants, or 83 percent), suggesting that Medicaid claims data routinely underestimate the prevalence of health conditions by an average of 25 to 30 percent. This underreporting by Medicaid claims data balances previous reports of underreporting in health surveys (17), suggesting that prevalence reports that rely on a single data source tend to underestimate the incidence of health problems in a population with severe mental illness.
Discussion and conclusions
Reliability and generalizability of the study findings
Confidence in the reliability of our study's prevalence ranks for 14 chronic health conditions is strengthened by the match in ranks between our study and the large epidemiologic study by Dickey and colleagues (8) for seven chronic health conditions, as well as a close match with condition ranks reported for a national sample (18) (Table 1). Likewise, our sample's 6 percent mortality rate for 1996 through 2001 is similar to the 4.4 percent mortality rate for 1989 to 1994 that was reported for a large Massachusetts sample (N=43,274) of adults with serious mental illness (24). The 27 percent rate of a current substance use disorder that we found is also comparable to the 24 to 29 percent rates that have been reported for research samples with similar psychiatric diagnoses (25,26,27). These findings, together with the close correspondence in sample characteristics between our sample and the large epidemiologic study, suggest that our sample is representative of the population of adults with serious mental illness in the state of Massachusetts.
Importance of level of specificity
Broadening the categories of asthma and gastrointestinal disorders (Table 1) to include all chronic respiratory and gastrointestinal conditions (Table 2) resulted in pulmonary disorders' outranking gastrointestinal disorders in prevalence (31 percent compared with 25 percent) within our study sample. This strong impact of method of classification on prevalence figures argues for consistency in level of specificity in comparisons of different conditions and for the adoption of standardized definitions.
Importance of study time frames
As the last two columns of Table 1 show, our study's cumulative prevalence rates for a four-year period were substantially higher than annual rates across the same four years, suggesting that underreporting in Medicaid claims data may be worse when the data are annualized. The differences in cumulative versus annualized rates also suggest that observation periods should be taken into account in cross-study comparisons.
Implications for research and service planning
The fact that 75 percent of our representative outpatient sample had a Medicaid-documented chronic health condition and that 50 percent had two or more chronic conditions suggests that the results of studies that screen for serious physical health problems (for example, many supported employment studies) are not generalizable to most persons with serious mental illness. The wide variability in the severity of physical health conditions in our sample also argues for the adoption of risk adjustment when mental health service outcomes or program performance indicators are compared across samples or treatment populations. The observed lack of correlation between prevalence of health problems and estimated annual treatment cost (Table 2) suggests that severity as well as prevalence of physical health conditions should be statistically controlled for when making cross-study or treatment group comparisons on mental health outcome measures. Counting the number of health conditions per person should provide a reliable measure of physical health severity, because condition counts correlate strongly with total cost of illness. Counts of physical health conditions have been found in other studies to predict both functioning and psychiatric symptoms (12,28).
The study findings also suggest that projected costs for the physical health treatment of adults with serious mental illness (29) should be adjusted for risk in the same way as costs for mental illness treatment (30). Underuse of medical health services by persons with serious mental illness is a growing concern (31,32,33), and if projected costs for adequate health care are underestimated because severity and prevalence of health conditions were not both taken into account, medical services may not be available to everyone who needs them.
Our findings that pulmonary illness is the most prevalent physical health problem among persons with serious mental illness and that it is second only to infectious diseases like AIDS in being the most severe and mortality-related condition replicate findings from other studies (7,34,35). Our study findings also underscore the fact that smoking is unusually high among persons with mental illness (36,37). Unfortunately, no ready-made interventions exist to address this problem, because tobacco addiction has an illness-related etiology and smoking cessation may elevate psychiatric symptoms (38,39). Likewise, although prevention and wellness interventions are increasing, few services exist that are tailored to the needs of the many persons with mental illness who already have serious physical problems. As the baby boomers within the population of adults with serious mental illness grow older, mental health programs may soon be serving a formidable number of individuals who are elderly, obese, actively abusing substances, and medically ill for whom existing psychiatric rehabilitation services are inappropriate. If we continue to focus on rehabilitation goals, like competitive employment, that are tailored to relatively healthy individuals, we may soon find a large cohort of older, physically ill individuals who spend their days in nursing homes and psychiatric hospitals (34). There is an immediate need for population-specific, interdisciplinary research to guide the design of integrated mental and physical health care for persons with serious mental illness (40,41), especially interventions that might ameliorate the long-term impact of combined physical and mental illness (28,42).
Acknowledgments
This study was supported by grant R01-MH-62628 from the National Institute of Mental Health, by collaborative agreement SM-51831 from the Substance Abuse and Mental Health Services Administration, by the van Ameringen Foundation, by the Rhodebeck Charitable Trust, and by Llewellyn and Nicholas Nicholas.
Dr. Jones, Dr. Macias, and Dr. Barreira are affiliated with the department of community intervention research at McLean Hospital, 115 Mill Street, Belmont, Massachusetts 02478-9106 (e-mail, [email protected]). Dr. Fisher is with the Center for Mental Health Services Research at the University of Massachusetts Medical School in Worcester. Dr. Hargreaves is with the department of psychiatry at the University of California, San Francisco. Dr. Harding is with the Sargent College of Health and Rehabilitation Sciences at Boston University.
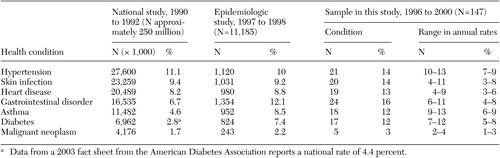 |
Table 1. Prevalence rates of health conditions in a national general-population study, an epidemiologic study of Medicaid enrollees with severe mental illness, and the sample of Medicaid enrollees with severe mental illness in this study
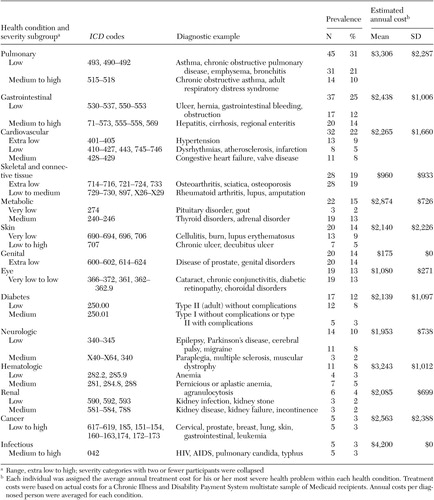 |
Table 2. Rank in prevalence of physical health conditions in a sample of 147 Medicaid enrollees with severe mental illness and the estimatedtotal annual costs per condition
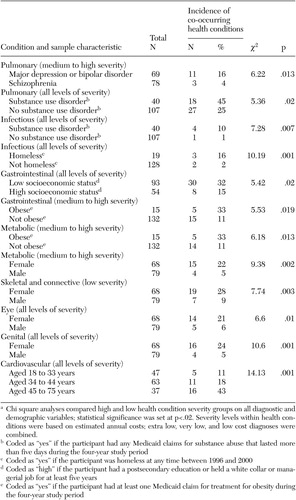 |
Table 3. Statistically significant differences in the prevalence rates of health conditions betweensubgroups of a sample of 147 Medicaid enrollees with severe mental illnessa
a Chi square analyses compared high and low health condition severity groups on all diagnostic anddemographic variables; statistical significance was set at p<.02. Severity levels within health conditions were based on estimated annual costs; extra low, very low, and low cost diagnoses were combined.
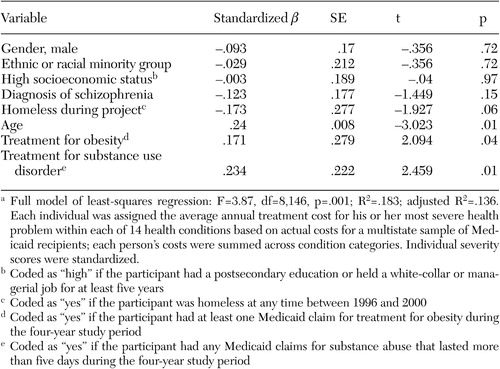 |
Table 4. Least-squares regression of sample characteristics on individual health problemseverity of 147 Medicaid enrollees with severe mental illnessa
a Full model of least-squares regression: F=3.87, df=8,146, p=.001; R2=.183; adjusted R2=.136. Each individual was assigned the average annual treatment cost for his or her most severe health problem within each of 14 health conditions based on actual costs for a multistate sample of Medicaid recipients; each person's costs were summed across condition categories. Individual severity scores were standardized.
1. Wallace B, Tennant C: Nutrition and obesity in the chronic mentally ill. Australian and New Zealand Journal of Psychiatry 32:82–85, 1998Crossref, Medline, Google Scholar
2. Holmberg SK, Kane C: Health and self-care practices of persons with schizophrenia. Psychiatric Services 50:827–829, 1999Link, Google Scholar
3. Daumit GL, Pratt LA, Crum RM, et al: Characteristics of primary care visits for individuals with severe mental illness. General Hospital Psychiatry 24:391–395, 2002Crossref, Medline, Google Scholar
4. Davidson S, Judd F, Jolley D, et al: Cardiovascular risk factors for people with mental illness. Australian and New Zealand Journal of Psychiatry 35:196–202, 2001Crossref, Medline, Google Scholar
5. Hansen V, Arnesen E, Jacobsen BK: Total mortality in people admitted to a psychiatric hospital. British Journal of Psychiatry 170:186–190, 1997Crossref, Medline, Google Scholar
6. Appleby L, Thomas S, Ferrier N, et al: Sudden unexplained death in psychiatric in-patients. British Journal of Psychiatry 174:405–406, 2000Crossref, Google Scholar
7. Prior P, Hassall C, Cross K: Causes of death associated with psychiatric illness. Journal of Public Health Medicine 18:381–389, 1996Crossref, Medline, Google Scholar
8. Dickey B, Normand S-L, Weiss R, et al: Medical morbidity, mental illness, and substance use disorders. Psychiatric Services 53:861–867, 2002Link, Google Scholar
9. Dixon L, Weiden P, Delahanty J, et al: Prevalence and correlates of diabetes in national schizophrenia samples. Schizophrenia Bulletin 26:903–912, 2000Crossref, Medline, Google Scholar
10. Gearon JS, Bellack AS: Women with schizophrenia and co-occurring substance use disorders: an increased risk for violent victimization and HIV. Community Mental Health Journal 35:401–419, 1999Crossref, Medline, Google Scholar
11. Stoskopf CH, Kim YK, Glover SH: Dual diagnosis: HIV and mental illness, a population-based study. Community Mental Health Journal 37:469–479, 2001Crossref, Medline, Google Scholar
12. Dixon L, Postrado L, Delahanty J, et al: The association of medical comorbidity in schizophrenia with poor physical and mental health. Journal of Nervous and Mental Disease 187:496–502, 1999Crossref, Medline, Google Scholar
13. Felker B, Yazel JJ, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356–1363, 1996Link, Google Scholar
14. Dixon L: Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophrenia Research 35(suppl):S93-S100, 1999Google Scholar
15. Koran LM, Sheline Y, Imai K, et al: Medical disorders among patients admitted to a public-sector psychiatric inpatient unit. Psychiatric Services 53:1623–1625, 2002Link, Google Scholar
16. Sox H, Koran L, Sox C, et al: A medical algorithm for detecting physical disease in psychiatric patients. Hospital and Community Psychiatry 40:1270–1276, 1989Abstract, Google Scholar
17. Mark TL, Buck JA, Dilonardo JD, et al: Medicaid expenditures on behavioral health care. Psychiatric Services 54:188–194, 2003Link, Google Scholar
18. Collins JG: Prevalence of Selected Chronic Conditions: United States, 1990–1992. Vital and Health Statistics: Series 10, Data From the National Health Survey:1–89, 1997Google Scholar
19. Cook JA, Carey MA, Razzano L, et al: The Pioneer: The Employment Intervention Demonstration Program in Conducting Multiple Site Evaluations in Real-World Settings: Vol 94. Edited by Herrell JM, Straw RB. San Francisco, Calif, Jossey-Bass, American Evaluation Association, 2002Google Scholar
20. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for Axes I and II DSM-IV Disorders (SCID-1/P). New York, Biometrics Research Department, New York State Psychiatric Institute, 1996Google Scholar
21. Report to the Congress on Medicare Payment Policy. Washington, DC, Medicaid Payment Advisory Commission, March 1998Google Scholar
22. Kronick R, Gilmer T, Dreyfus T, et al: Improving health-based payment for Medicaid beneficiaries: CDPS. Health Care Financing Review 21:29–64, 2000Medline, Google Scholar
23. Kay SR, Fiszbein A, Opler LA: The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin 13:261–276, 1987Crossref, Medline, Google Scholar
24. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036–1042, 1999Link, Google Scholar
25. Graham HL, Maslin J, Copello A, et al: Drug and alcohol problems amongst individuals with severe mental health problems in an inner city area of UK. Social Psychiatry and Psychiatric Epidemiology 36:448–455, 2001Crossref, Medline, Google Scholar
26. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and drug abuse: results from the Epidemiological Catchment Area (ECA) Study. JAMA 264:2511–2518, 1990Crossref, Medline, Google Scholar
27. Weaver T, Hickman M, Rutter D, et al: The prevalence and management of co-morbid substance misuse and mental illness: results of a screening survey in substance misuse and mental health treatment populations. Drug and Alcohol Review 20:407–416, 2001Crossref, Google Scholar
28. Druss BG, Marcus SC, Rosenheck RA, et al: Understanding disability in mental and general medical conditions. American Journal of Psychiatry 157:1485–1491, 2000Link, Google Scholar
29. Druss BG, Rosenheck RA: Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatric Services 50:214–218, 1999Link, Google Scholar
30. Dickey B, Hermann RC, Eisen SV: Assessing the quality of psychiatric care: research methods and application of clinical practice. Harvard Review of Psychiatry 6:88–96, 1998Crossref, Medline, Google Scholar
31. Druss BG, Rosenheck RA: Mental disorders and access to medical care in the United States. American Journal of Psychiatry 155:1775–1777, 1998Link, Google Scholar
32. Berren M, Santiago JM, Zent MR, et al: Health care utilization by persons with severe and persistent mental illness. Psychiatric Services 50:559–561, 1999Link, Google Scholar
33. Morrissey JP, Stroup TS, Ellis AR, et al: Service use and health status of persons with severe mental illness in full-risk and no-risk Medicaid programs. Psychiatric Services 53:293–298, 2002Link, Google Scholar
34. Kamara SG, Peterson PD, Dennis JL: Prevalence of physical illness among psychiatric inpatients who die of natural causes. Psychiatric Services 49:788–793, 1998Link, Google Scholar
35. Amaddeo F, Bisoffi G, Bonizzato P, et al: Mortality among patients with psychiatric illness: a ten-year case register study in an area with a community-based system of care. British Journal of Psychiatry 166:783–788, 1995Crossref, Medline, Google Scholar
36. Kager A, Berghofer G, Lang A, et al: Smoking: an addiction of mentally ill patients? European Journal of Psychiatry 14:69–77, 2000Google Scholar
37. Lasser K, Boyd JW, Woolhandler S, et al: Smoking and mental illness: a population-based prevalence study. JAMA 284:2606–2610, 2000Crossref, Medline, Google Scholar
38. Leonard S, Adler LE, Benhammou K, et al: Smoking and mental illness. Pharmacology, Biochemistry, and Behavior 70:561–570, 2001Crossref, Medline, Google Scholar
39. Lucksted A, Dixon L, Sembly JB: A focus group pilot study of tobacco smoking among psychosocial rehabilitation clients. Psychiatric Services 51:1544–1548, 2000Link, Google Scholar
40. Barreira P: Reduced life expectancy and serious mental illness. Psychiatric Services 50:995–996, 1999Link, Google Scholar
41. Druss BG, Rohrbaugh RM, Levinson CM, et al: Integrated medical care for patients with serious psychiatric illness: a randomized trial. Archives of General Psychiatry 58:861–868, 2001Crossref, Medline, Google Scholar
42. Pledger C: Discourse on disability and rehabilitation issues: opportunities for psychology. American Psychologist 58:279–284, 2003Crossref, Medline, Google Scholar



