The Quality of Asthma Care Among Adults With Substance-Related Disorders and Adults With Mental Illness
Asthma remains a significant source of morbidity and mortality in the United States. Recent reports from the Centers for Disease Control and Prevention estimate that 7.7% of Americans currently have asthma, while 11.2% will experience asthma at some point during their lifetimes. In 2004 a total of 1.8 million emergency room visits, 14.7 million outpatient visits, and 497,000 hospitalizations were attributed to asthma. Over 4,000 people in the United States die from asthma each year ( 1 ).
Government health agencies have devoted a great deal of attention to improving the quality of asthma care over the past two decades ( 2 , 3 , 4 ). The Healthcare Effectiveness Data and Information Set (HEDIS), published by the National Committee for Quality Assurance, provides quality measures for a number of medical conditions, including asthma ( 5 ). These measures allow managed care organizations and other health plans to track and compare the rates at which medical services delivered meet these standardized quality benchmarks.
Current treatment guidelines emphasize the importance of identifying patients with more severe asthma and of decreasing symptoms and the frequency of complications through the use of long-term controller medications ( 6 ). Use of controller medications, especially inhaled corticosteroids, has been associated with decreased incidence of asthma exacerbations ( 7 ), hospitalizations ( 8 , 9 ), emergency department utilization ( 10 ), and death ( 9 , 11 ).
The 2007 HEDIS quality measure for asthma treatment focuses on patients' meeting HEDIS criteria for persistent asthma; these patients are expected to show at least one dispensing event for a long-term controller medication each year ( 5 ). Recent studies have suggested, however, that the ratio of long-term controller medications to the total number of asthma medications dispensed may be a more effective measure of the quality of asthma treatment than the one-time prescription of a controller medication ( 12 ).
Asthma and other medical conditions are found at higher rates among patients with mental illness and those with substance-related disorders ( 13 , 14 , 15 , 16 , 17 ). There is a growing body of evidence that patients with mental illness and those with substance-related disorders may receive lower-quality care for some medical conditions ( 18 , 19 , 20 , 21 , 22 , 23 ), but no studies have evaluated the quality of asthma care in these populations.
The purpose of this study was to investigate whether the presence of substance-related disorders or mental illness may affect the quality of medication management in asthma care. We estimated the odds of patients with these conditions achieving established quality benchmarks for asthma care, while controlling for demographic factors. We hypothesized that patients with these conditions would be significantly less likely than patients without these conditions to achieve asthma medication quality standards.
Methods
We analyzed Medicaid claims for the year 1999 from five states representing different regions of the United States: Colorado, Georgia, Indiana, New Jersey, and Washington. For our study population we selected adults ages 18–56 and restricted our sample to patients whose files contained specific coding for asthma ( ICD-9 code 493.x) to minimize the inclusion of patients with other, nonasthma pulmonary conditions. Beneficiaries who had Medicare or private health insurance in addition to Medicaid were excluded, because claims from payers other than Medicaid were not available. We included patients with a minimum Medicaid enrollment of 30 days and controlled statistically for enrollment duration. Claims from each state were analyzed separately, because Medicaid benefits, demographic characteristics, and medical provider resources vary widely from state to state.
From this sample, we selected patients who met HEDIS persistent asthma criteria for our analysis. HEDIS technical specifications categorize a patient as having persistent asthma if he or she meets one of the following criteria in both the study year and in the year prior: one or more emergency department visits with a primary diagnosis of asthma; one or more hospital admissions with a primary diagnosis of asthma; four or more outpatient visits with asthma listed as any of the diagnoses, along with at least two asthma medication dispensing events; or four or more separate asthma medication dispensing events. Because our data set included claims only for calendar year 1999, it did not allow identification of persistent asthma criteria in two consecutive years, as described in the HEDIS specifications.
Rates of achieving the HEDIS quality standard (at least one long-term controller medication during the study year) and the quality measure described by Schatz and colleagues ( 12 ) (a ratio of long-term controller medications to total number of asthma medications of ≥.5) were measured by using National Drug Codes from pharmaceutical claims. Patients who met our inclusion criteria but who had no documented dispensing events for any asthma medications were included in the analysis.
Patients in the sample with substance-related disorders were identified through ICD-9 coding (291.x, 292.x, 303.x, 304.x, 305.2–305.9, and 648.3). Coding for tobacco use disorders (305.1) was found only rarely and therefore was not included in the analysis. Patients with mental illness were identified through ICD-9 coding for major depression and other depressive disorders (296.2, 296.3, 300.4, and 311), anxiety disorders (300.xx, excluding 300.4), bipolar disorder (296.0–296.9, excluding 296.2 and 296.3), schizophrenia disorders (295.x), and other psychiatric disorders (297.x–315.x, excluding all diagnostic codes listed in other study categories).
We first compared the unadjusted proportions of patients with persistent asthma and substance-related disorders or mental illness who met either the HEDIS or the ratio quality measure. Statistically significant differences were identified with Fisher's exact tests, with significance defined as p≤.05.
By using logistic regression adjusting for age, gender, race or ethnicity, and length of Medicaid enrollment, we then estimated the odds of achieving these asthma quality measures at the individual level for patients with substance-related disorders and those with mental illness. Adjusted odds ratios for achieving each of the two quality measures are reported separately for patients with substance-related disorders, depressive disorders, anxiety disorders, bipolar disorder, schizophrenia disorders, and other mental illness.
Results
Initial samples of patients identified as having an asthma diagnosis ranged from 2,205 to 9,056, with over half of these patients meeting criteria for persistent asthma in each state (range 51.6%–64.2%). Table 1 describes the composition for each state of the sample with persistent asthma, which was predominantly female (range 77.3%–86.7%) and relatively evenly distributed by age. Over two-thirds of the samples had Medicaid coverage for the entire study year (range 67.0%–77.2%). The racial composition of the samples varied widely by state.
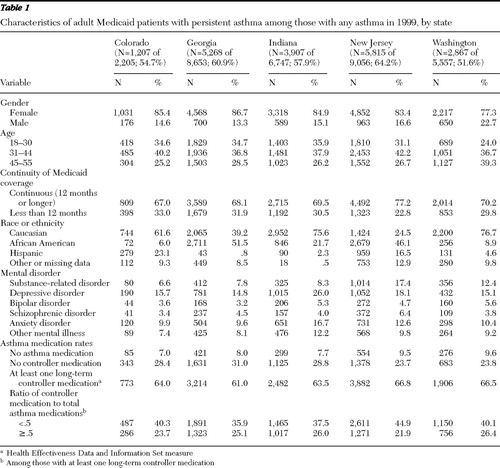 |
Coding for substance-related disorders was found at rates ranging from 6.6% to 17.4%. Coding for mental illness was found at the highest rates for depressive disorders (range 14.8%–26.0%) and anxiety disorders (range 9.6%–16.7%). Coding for bipolar disorder ranged from 3.2% to 5.6%, while coding for schizophrenia disorders ranged from 3.4% to 6.4%. Other psychiatric diagnostic codes were combined into a single "other mental illness" category (range 7.4%–12.2%).
Approximately two-thirds (range 61.0%–66.8%) of the study sample met the HEDIS quality criterion of having at least one dispensing event for a long-term controller medication. Only about one-quarter (range 21.9%–26.4%) of patients meeting persistent asthma criteria achieved a ratio of controller medications to total asthma medications ≥.5.
Analysis of the unadjusted data showed that patients with substance-related disorders achieved asthma care quality measures at lower rates than patients without substance-related diagnoses ( Table 2 ). For the HEDIS measure, these differences did not reach statistical significance. The rates of achieving the medication ratio of ≥.5 were significantly lower in the population with substance-related disorders in four of the five states studied.
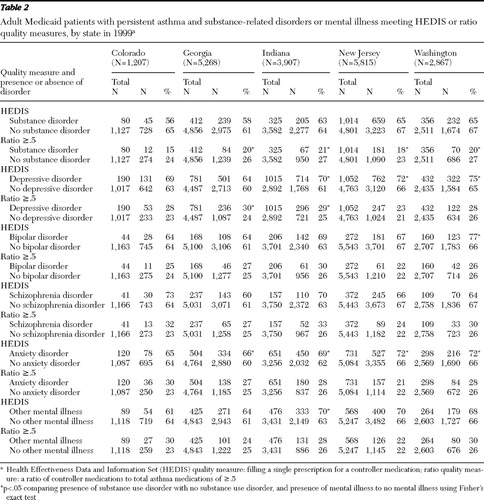 |
Analysis of data for patients with mental illness showed dramatically different results: rates of achieving asthma quality measures trended higher for these patients ( Table 2 ). Patients with depressive disorders and anxiety disorders, respectively, were significantly more likely to meet the HEDIS quality criterion in four and three of the five states studied. Rates for patients with bipolar disorder and patients with other mental illness were significantly increased in only one of the five states. Evaluation of the ratio measure showed fewer significant differences. Patients with depressive disorders achieved the ratio measure at significantly increased rates in two of the five states studied, but differences were not significant in any state for any of the other mental illness categories studied. In the unadjusted data, patients with schizophrenia disorders showed no significant differences for either measure.
Many differences emerged when the data were adjusted for demographic characteristics, continuity of Medicaid coverage, and the presence of co-occurring substance-related or mental disorders. Table 3 shows the adjusted odds of achieving the HEDIS quality measure. Patients with substance-related disorders showed lower odds of achieving the measure; the difference reached statistical significance in two states: Georgia (odds ratio [OR]=.79) and New Jersey (OR=.81). Patients in these two states were also less likely to achieve the HEDIS measure if they had a schizophrenia disorder: Georgia (OR=.69) and New Jersey (OR=.69). Odds of achieving the HEDIS measure were significantly increased for patients with depressive disorders in two states (Indiana, OR=1.34, and Washington, OR=1.37) and in one state each for bipolar disorder (Washington, OR=1.69) and other mental illness (Indiana, OR=1.47). Unlike in the unadjusted data, no significant differences were found for patients with anxiety disorders.
 |
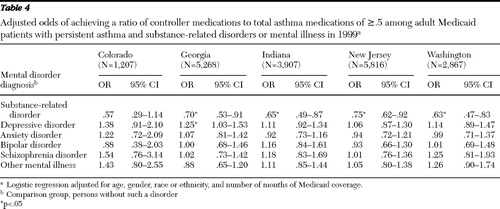
Table 4 shows the adjusted odds of achieving a ratio of long-term controller medication to total asthma medications of ≥.5. Odds of achieving this quality measure were significantly lower for patients with substance-related disorders in four of the five states studied, with odds ratios ranging from .63 to .75. For mental disorders, odds of achieving this measure differed significantly only for patients with depressive disorders and only in Georgia (OR=1.3).
 |
Discussion
Our findings suggest that substance-related disorders and mental illness may influence rates at which patients achieve standardized asthma care quality measures, but this occurred in different ways than we originally hypothesized.
Past studies have shown that patients who abuse drugs may be at increased risk of severe asthma exacerbations or asthma death ( 24 , 25 , 26 , 27 , 28 , 29 , 30 ), but there has been little information to explain this association beyond the understanding that inhaled drugs may trigger severe asthma exacerbations. Our findings demonstrate that patients with substance-related disorders and persistent asthma fill prescriptions for controller medications at lower rates than patients without substance-related disorders. Although we cannot say whether these differences are due to differential access to care, decreased compliance with treatment recommendations, or the receipt of substandard care, these findings still may partially explain the disparities in asthma outcomes observed for these patients.
Decreased utilization of outpatient asthma care may also be a factor contributing to the decreased quality of asthma care for patients with substance-related disorders, because efforts to improve asthma care have largely focused on improving monitoring and prescribing practices in outpatient settings ( 2 , 3 , 6 ). We have shown in a recent analysis ( 31 ) that patients with substance-related disorders were half as likely as patients without these disorders to receive asthma care in outpatient settings, and therefore they may be less likely to benefit from outpatient-based quality improvement efforts.
Patients with mental illness showed more variable results. In general, with the exception of patients with schizophrenia disorders, patients with mental illness were equally or more likely to achieve the HEDIS asthma care quality measure, compared with patients without mental illness. These differences suggest that patients with some forms of mental illness may be receiving an enhanced level of care in some states, which may, in turn, be leading to improved compliance with quality guidelines. Patients with mental illness and asthma may have closer monitoring, more frequent contact with the medical system, or greater access to specialists, all of which may lead to a greater likelihood that their asthma will be recognized and treated with the initiation of controller medications.
In contrast, patients with schizophrenia disorders showed lower odds of achieving the HEDIS measure. As with patients with substance-related disorders, these differences could be due to barriers to accessing medical care, decreased compliance with treatment recommendations, or lower-quality medical care for asthma ( 32 ). It appears then that even if in some states enhanced care for patients with asthma and mental illness is provided, this benefit may not extend to patients with schizophrenia disorders.
Our findings show some variability by diagnosis for patients with mental illness among the states, which may result from differences in sample sizes, rates of mental illness, diagnostic accuracy, the precision of coding, and differences in characteristics of the mental illnesses studied. Differences in care delivery systems and benefit structures among the states may also contribute.
Our results also show significant variability between the two quality measures. Only about one-quarter (21.9%–26.4%) of the patients in our samples met the ratio measure, and approximately two-thirds (61.0%–66.8%) of the samples met the HEDIS measure, even though both the HEDIS measure ( 10 , 33 ) and the ratio measure ( 12 , 34 ) have been shown to be predictive of some outcomes in selected samples. Patients with substance-related disorders showed lower odds of achieving both the HEDIS and the ratio measures, but the odds of achieving the ratio were more consistently decreased across the states. For patients with mental illness, differences found in the odds of achieving the HEDIS measure did not persist for the ratio measure. The HEDIS measure, which looks only at a single prescription filling event for a controller medication, may be more sensitive than the ratio measure to the influences of mental illness and mental health treatment on asthma care. On the other hand, the ratio measure may be capturing increased utilization of rescue medications among patients with substance-related disorders, which would increase the denominator in this measure and drive the ratios lower.
The variability between these measurements may also reflect some limitations in the current approach to assessing asthma care quality. Questions have been raised about the validity of the criteria for persistent asthma ( 35 , 36 ) that form the foundation for both of the quality measures used in this study. Many patients do not meet these criteria from year to year. The quantity of controller medications prescribed and adherence to those medications may be better predictors of utilization outcomes than the HEDIS benchmark, which measures the dispensing of only a single controller prescription ( 10 ).
No studies have evaluated the association between existing administrative quality measures and clinical outcomes in high-risk subpopulations, such as patients with mental disorders, despite studies showing that patients with substance-related disorders ( 27 , 28 , 29 , 30 ) and some forms of mental illness ( 37 , 38 , 39 , 40 , 41 ) may have poorer asthma outcomes. In addition, factors that are likely to affect the quality of asthma care and clinical outcomes in these populations are often not addressed by current quality assessment methods. For example, these measures do not incorporate any direct measurement of disease severity, which may be higher among patients with mental disorders. Smoking rates among patients with mental disorders are at least twice as high as those found in the general population ( 42 ), but adjusting for tobacco use can be difficult when using administrative data. Patients using tobacco are also less responsive to inhaled steroids, suggesting that smoking may lead to poorer asthma outcomes, even when quality measures based on the use of inhaled steroids are met ( 43 , 44 ). Specific studies are warranted to examine the determinants of asthma care quality among patients with substance-related disorders and those with mental disorders and to examine the ability of administrative quality measures to predict improved clinical outcomes in these high-risk subpopulations.
This study draws from a large database of Medicaid claims and shows some consistency of results across multiple states despite differences in demographic characteristics and the structure of Medicaid-funded treatment services. Our findings, therefore, may be somewhat generalizable to other Medicaid populations, especially for patients with substance use disorders. We utilized existing, accepted measures of asthma care quality; the HEDIS measure is the current standard for comparing performance among managed care organizations ( 36 ), and the ratio of controller medication to total asthma medications has recently been validated as being associated with improved quality-of-life scores and decreased future emergency and inpatient hospital utilization ( 12 ). The assessment of asthma care quality in our study was facilitated by access to Medicaid pharmaceutical claims, which provided a comprehensive record of prescriptions filled by the Medicaid recipients included in the analysis.
This study is limited by having only one year of data available, making it necessary to identify patients with persistent asthma and measure their medication utilization within the same year. Our samples may include more patients with less severe asthma who would not meet persistent asthma criteria in consecutive years. Restricting our samples to Medicaid patients between the ages of 18 and 56 limits the ability to generalize our findings to other populations, and socioeconomic factors that may affect the quality of care, such as income, education level, and population density, were not evaluated. Also, our findings were derived from 1999 coding data and will not reflect any changes in asthma care guidelines, or improvements in adherence to those guidelines, that have taken place in the intervening years.
The persistent asthma designation is only a proxy for asthma severity; our data do not permit any direct measure of asthma severity, such as symptom ratings, quality-of-life scores, peak flow measurements, or pulmonary function testing. In addition, the quality measures studied evaluate rates of dispensing controller medications and do not include any direct measure of medication adherence. Finally, our study relied on administrative data to identify patients with substance-related disorders and those with mental illness. As such, a number of patients with these disorders may have been excluded from the analysis as a result of low rates of screening, lack of precision in making diagnoses, and incomplete or inaccurate diagnostic coding.
Conclusions
Our data show that patients with substance-related disorders and those with schizophrenia disorders were less likely to achieve asthma care quality benchmarks in some states, while patients with other forms of mental illness may be more likely to achieve the benchmark. Further studies are needed to determine the components of asthma care most representative of quality in these populations, as well as the ability of administrative quality measures to predict clinical outcomes in high-risk subpopulations, such as patients with mental illness and patients with substance-related disorders.
Acknowledgments and disclosures
Preparation of this article was assisted by a grant from the Robert Wood Johnson Foundation Substance Abuse Policy Research Program.
The authors report no competing interests.
1. Akinbami L: Asthma Prevalence, Health Care Use and Mortality: United States, 2003–2005. Hyattsville, Md, Centers for Disease Control, National Center for Health Statistics 2006. Available at www.cdc.gov/nchs Google Scholar
2. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md, National Heart, Lung, and Blood Institute, 1997. Available at www.nhlbi.nih.gov/guidelines/archives/epr-2/asthgdlnarchive.pdf Google Scholar
3. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma—Update of Selected Topics 2002 (EPR-update 2002). Bethesda, Md, National Heart, Lung, and Blood Institute, 2003. Available at www.nhlbi.nih.gov/guidelines/archives/epr-2upd Google Scholar
4. Healthy People 2010, Vol II, 2nd ed. Objectives for Improving Health (Part B: Focus Areas 15–28). Washington, DC, US Department of Health and Human Services, 2000. Available at www.healthypeople.gov/publications Google Scholar
5. HEDIS 2007: Technical Specifications, Vol 2. Washington, DC, National Committee for Quality Assurance, 2007Google Scholar
6. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md, National Heart, Lung, and Blood Institute, 2007. Available at www.nhlbi.nih.gov/guidelines Google Scholar
7. Sin DD, Man J, Sharpe H, et al: Pharmacological management to reduce exacerbations in adults with asthma: a systematic review and meta-analysis. JAMA 292:367–376, 2004Google Scholar
8. Suissa S, Ernst P, Kezouh A: Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax 57:880–884, 2002Google Scholar
9. Suissa S, Ernst P: Inhaled corticosteroids: impact on asthma morbidity and mortality. Journal of Allergy and Clinical Immunology 107:937–944, 2001Google Scholar
10. Berger WE, Legorreta AP, Blaiss MS, et al: The utility of the Health Plan Employer Data and Information Set (HEDIS) asthma measure to predict asthma-related outcomes. Annals of Allergy, Asthma, and Immunology 93:538–545, 2004Google Scholar
11. Suissa S, Ernst P, Benayoun S, et al: Low-dose inhaled corticosteroids and the prevention of death from asthma. New England Journal of Medicine 343:332–336, 2000Google Scholar
12. Schatz M, Zeiger RS, Vollmer WM, et al: The controller-to-total asthma medication ratio is associated with patient-centered as well as utilization outcomes. Chest 130:43–50, 2006Google Scholar
13. Mertens JR, Lu YW, Parthasarathy S, et al: Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Archives of Internal Medicine 163:2511–2517, 2003Google Scholar
14. Dickey B, Normand SL, Weiss RD, et al: Medical morbidity, mental illness, and substance use disorders. Psychiatric Services 53:861–867, 2002Google Scholar
15. Sokal J, Messias E, Dickerson FB, et al: Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Disease 192:421–427, 2004Google Scholar
16. Jones DR, Macias C, Barreira PJ, et al: Prevalence, severity, and co-occurrence of chronic physical health problems of persons with serious mental illness. Psychiatric Services 55:1250–1257, 2004Google Scholar
17. Kilbourne AM, Cornelius JR, Han X, et al: Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disorders 6:368–373, 2004Google Scholar
18. Druss BG, Bradford WD, Rosenheck RA, et al: Quality of medical care and excess mortality in older patients with mental disorders. Archives of General Psychiatry 58: 565–572, 2001Google Scholar
19. Druss BG, Rosenheck RA, Desai MM, et al: Quality of preventive medical care for patients with mental disorders. Medical Care 40:129–136, 2002Google Scholar
20. Frayne SM, Halanych JH, Miller DR, et al: Disparities in diabetes care: impact of mental illness. Archives of Internal Medicine 165:2631–2638, 2005Google Scholar
21. Cradock-O'Leary J, Young AS, Yano EM, et al: Use of general medical services by VA patients with psychiatric disorders. Psychiatric Services 53:874–878, 2002Google Scholar
22. Desai MM, Rosenheck RA, Druss BG, et al: Mental disorders and quality of diabetes care in the Veterans Health Administration. American Journal of Psychiatry 159:1584–1590, 2002Google Scholar
23. Goldberg RW, Kreyenbuhl JA, Medoff DR, et al: Quality of diabetes care among adults with serious mental illness. Psychiatric Services 58:536–543, 2007Google Scholar
24. Krantz AJ, Hershow RC, Prachand N, et al: Heroin insufflation as a trigger for patients with life-threatening asthma. Chest 123: 510–517, 2003Google Scholar
25. Osborn HH, Tang M, Bradley K, et al: New-onset bronchospasm or recrudescence of asthma associated with cocaine abuse. Academic Emergency Medicine 4: 689–692, 1997Google Scholar
26. Rome LA, Lippmann ML, Dalsey WC, et al: Prevalence of cocaine use and its impact on asthma exacerbation in an urban population. Chest 117:132–139, 2000Google Scholar
27. Levine M, Iliescu ME, Margellos-Anast H, et al: The effects of cocaine and heroin use on intubation rates and hospital utilization in patients with acute asthma exacerbations. Chest 128:1951–1957, 2005Google Scholar
28. Weitzman JB, Kanarek NF, Smialek JE: Medical examiner asthma death autopsies: a distinct subgroup of asthma deaths with implications for public health preventive strategies. Archives of Pathology and Laboratory Medicine 122:691–699, 1998Google Scholar
29. Tatum AM, Greenberger PA, Mileusnic D, et al: Clinical, pathologic, and toxicologic findings in asthma deaths in Cook County, Illinois. Allergy and Asthma Proceedings 22:285–291, 2001Google Scholar
30. Levenson T, Greenberger PA, Donoghue ER, et al: Asthma deaths confounded by substance abuse: an assessment of fatal asthma. Chest 110:604–610, 1996Google Scholar
31. Baxter JD, Samnaliev M, Clark RE: Patterns of health care utilization for asthma in adults with substance use disorders. Journal of Addiction Medicine 2:79–84, 2008Google Scholar
32. Druss BG, von Esenwein SA: Improving general medical care for persons with mental and addictive disorders: systematic review. General Hospital Psychiatry 28:145–153, 2006Google Scholar
33. Fuhlbrigge A, Carey VJ, Adams RJ, et al: Evaluation of asthma prescription measures and health system performance based on emergency department utilization. Medical Care 42:465–471, 2004Google Scholar
34. Schatz M, Nakahiro R, Crawford W, et al: Asthma quality-of-care markers using administrative data. Chest 128:1968–1973, 2005Google Scholar
35. Mosen DM, Macy E, Schatz M, et al: How well do the HEDIS asthma inclusion criteria identify persistent asthma? American Journal of Managed Care 11:650–654, 2005Google Scholar
36. Gelfand EW, Colice GL, Fromer L, et al: Use of the Health Plan Employer Data and Information Set for measuring and improving the quality of asthma care. Annals of Allergy, Asthma, and Immunology 97:298–305, 2006Google Scholar
37. Lavoie KL, Cartier A, Labrecque M, et al: Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respiratory Medicine 99:1249–1257, 2005Google Scholar
38. Lavoie KL, Bacon SL, Barone S, et al: What is worse for asthma control and quality of life: depressive disorders, anxiety disorders, or both? Chest 130:1039–1047, 2006Google Scholar
39. Ten Brinke A, Ouwerkerk ME, Zwinderman AH, et al: Psychopathology in patients with severe asthma is associated with increased health care utilization. American Journal of Respiratory and Critical Care Medicine 163:1093–1096, 2001Google Scholar
40. Eisner MD, Katz PP, Lactao G, et al: Impact of depressive symptoms on adult asthma outcomes. Annals of Allergy, Asthma, and Immunology 94:566–574, 2005Google Scholar
41. Wainwright NW, Surtees PG, Wareham NJ, et al: Psychosocial factors and incident asthma hospital admissions in the EPIC-Norfolk cohort study. Allergy 62:554–560, 2007Google Scholar
42. Lasser K, Boyd JW, Woolhandler S, et al: Smoking and mental illness: a population-based prevalence study. JAMA 284:2606–2610, 2000Google Scholar
43. Tomlinson JE, McMahon AD, Chaudhuri R, et al: Efficacy of low and high dose inhaled corticosteroid in smokers versus non-smokers with mild asthma. Thorax 60:282–287, 2005Google Scholar
44. Chalmers GW, Macleod KJ, Little SA, et al: Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax 57:226–230, 2002Google Scholar



