Medical Morbidity, Mental Illness, and Substance Use Disorders
Abstract
OBJECTIVE: Previous research on the prevalence of medical disorders among adults with mental illness has been inconclusive. In general, studies have found higher rates among persons with mental illness, but these studies did not account for comorbid substance use disorders. The authors examined whether certain medical disorders are more prevalent among adults with severe mental illness and whether a comorbid substance use disorder increases prevalence beyond the effect of severe mental illness alone. METHODS: Administrative data from the Massachusetts Division of Medical Assistance were used in a cross-sectional observational study design. The sample consisted of 26,332 Medicaid beneficiaries 18 to 64 years of age. Of these, 11,185 had been treated for severe mental illness. Twelve-month prevalence rates were computed, and logistic regression was used to estimate the effect of a substance use disorder or another mental illness on the risk of having a medical disorder. RESULTS: Compared with Medicaid beneficiaries who were not treated for severe mental illness, those with severe mental illness had a significantly higher age- and gender-adjusted risk of the medical disorders considered in the study. Those with a comorbid substance use disorder had the highest risk for five of the disorders. CONCLUSIONS: The higher treated prevalence of certain medical disorders among adults with severe mental illness has three implications: substance use disorder is an important risk factor and requires early detection; integration of the treatment of medical disorders and severe mental illness should receive higher priority; and efforts should be made to develop specialized disease self-management techniques.
Although it is commonly believed that persons with mental illness have an unusually high prevalence of medical disease, research to date has yielded inconsistent findings. Moreover, published estimates have not been adjusted for differences in sociodemographic characteristics or the contribution of comorbid substance use disorders. The prevalence of medical disorders among persons with severe mental illness has important policy implications because of the growth of carve-out behavioral health plans that separate the treatment of mental and medical illness. The purpose of this study was to test whether and to what extent certain common medical disorders are more prevalent among adults with severe mental illness and to examine whether comorbid substance use disorders contribute to the rates of medical illness.
Several epidemiological studies of medical comorbidity among patients with psychiatric illness have been conducted. Koran and associates (1) reviewed the medical status of 500 psychiatric inpatients and found that 291 (about 60 percent) had significant active medical disorders, of which hypertension, epilepsy, organic brain syndrome, diabetes, and hepatitis were the most common. More recently, in a survey of 719 persons with schizophrenia by Dixon and associates (2), the majority reported at least one medical problem; poor eyesight, dental problems, and high blood pressure were the most common complaints.
Reports about co-occurring medical and mental illness are inconsistent, however. A review by Jeste and colleagues (3) suggested that people with schizophrenia may not have more coexisting medical illnesses than the general population, although their illnesses may be more severe, which suggests inadequate medical treatment. Furthermore, these authors speculated that schizophrenia may act as a buffer for certain disorders. In support of these findings, Eaton and associates (4) published a review of epidemiological studies that consistently found a negative relationship between rheumatoid arthritis and schizophrenia. They also reported that rates of cancer were no different for adults with schizophrenia than for the general public, but they found some evidence that the risk of lung cancer was lower among adults with schizophrenia (5,6,7), despite high rates of nicotine dependence. Several other authors have investigated the association of schizophrenia with other specific disorders (8,9,10,11,12), but the findings have been mixed.
It has long been known that habitual alcohol use increases the likelihood of developing many disorders, such as liver, heart, and gastrointestinal disease, and exacerbates others, such as diabetes and hypertension (13). However, the degree to which mental illness adds extra risk of developing these disorders is unclear. In two cross-sectional studies of patients with psychotic disorders, chronic medical problems rated by case managers were not correlated with substance use disorders (14,15). These studies did not control for age, however. Because the frequency of chronic medical disorders increases with age and substance users are more often younger, the studies may have underestimated the association between chronic medical disorders, substance use, and mental illness.
Few health services research studies have examined the association of substance use disorders, mental disorders, and medical disorders. Compared with clinical studies, health services research studies have much larger samples, broader sampling frames, and more inclusive diagnostic categories. However, administrative data lack clinical detail, and the observational design of these studies prohibits causal interpretations. One study of health care utilization examined the public health implications of co-occurring chronic medical problems, depression, and drinking among 2,546 adults (16); when all three conditions were present, the likelihood of seeking mental health treatment was lower. In an observational study of 6,884 adult Medicaid recipients with schizophrenia, Dickey and associates (17) compared those with and those without co-occurring substance use disorders and found no differences in the age- and gender-adjusted frequency of diabetes, hypertension, heart disease, asthma, infections of the skin and subcutaneous tissue, malignant neoplasms, acute respiratory disorders, and diseases of the esophagus, stomach, and duodenum. The National Comorbidity Study (18), the most widely known psychiatric comorbidity study, did not include information about comorbid medical disorders.
To contribute to this body of research, we investigated whether certain medical disorders were more prevalent among adults with severe mental illness and whether comorbid substance use disorders increased the prevalence of certain medical disorders beyond the effect of severe mental illness alone.
Methods
Data source
Claims paid by Medicaid in Massachusetts from July 1, 1997, to June 30, 1998, were used to develop the database for the study. The sample was drawn from a pool of adult Medicaid beneficiaries comprising all claimants with a psychotic disorder in the disabled benefit category and a random sample of 30 percent of claimants with no mental illness in the Aid to Families With Dependent Children (AFDC) benefit category. We included all of the disabled enrollees with a psychiatric disorder and 30 percent of the AFDC enrollees without a mental disorder to create two groups of sufficient size for the statistical analysis of the presence of certain medical disorders within these groups. The study was exempt from institutional review board approval, because only de-identified administrative data were used.
Sampling
We selected all disabled beneficiaries who had at least one claim for the treatment of schizophrenia, bipolar disorder, or another psychotic disorder. We used the following hierarchical algorithm to assign diagnoses to enrollees. If, over the course of one year, the person had a diagnosis of schizophrenia, we assigned that person a diagnosis of schizophrenia. If the person did not have a diagnosis of schizophrenia but had a diagnosis of bipolar disorder, we recorded a diagnosis of bipolar disorder. If the person did not have a diagnosis of schizophrenia or bipolar disorder but did have one other diagnosis of a psychotic disorder, we coded the diagnosis as "other psychoses." This set of three diagnoses was categorized as psychotic disorders (N=11,185).
For comparison, we identified AFDC beneficiaries who did not have any claims for mental illness (N=15,147). Thus the total sample consisted of 26,332 Medicaid beneficiaries 18 to 64 years of age. We used the beneficiaries' unique Medicaid identification numbers to extract data on their paid claims during the study period, including claims for all treatment of psychiatric and substance use disorders and claims for the treatment of medical disorders.
We categorized an individual as having a substance use disorder if the person had any claim with a primary or secondary diagnosis of substance use disorder. To identify persons with a substance use disorder, we used all ICD-9 codes for alcohol and drug use or abuse.
We chose eight medical disorders or groups of disorders to test for differences in frequencies across groups: diabetes; hypertension; heart disease (ischemic heart disease, heart rhythm disorders, and other heart disorders); asthma; gastrointestinal disorders (diseases of the esophagus, stomach, and duodenum); infections of the skin and subcutaneous tissue; malignant neoplasms; and acute respiratory disorders (pneumonia and influenza). We selected these disorders because they represent major health problems in the general population, because they were likely to produce enough cases for the analyses, and because many of them are known to be related to substance use.
Statistical analyses
We examined the proportion of individuals treated for each of the eight medical disorders in each of the four study groups: patients with psychotic disorders without comorbid substance use disorder, those with psychotic disorders and comorbid substance use disorder, those with substance use disorder alone, and those with no mental illness or substance use disorder. Chi square tests of association between treatment for the medical disorder and presence of mental illness were conducted separately for each disorder. To avoid false-positive results when multiple tests were conducted, we used a Bonferroni adjustment to set statistical significance at a p value of less than .006; this cutoff was chosen so that the p value for significance in all tests simultaneously would be .05 (that is, .05/8=.006 ).
To examine whether the presence of a substance use disorder differentially affected the odds of treatment for a medical disorder depending on the presence of mental illness, we estimated logistic regression models separately for each disorder, including an interaction term. The interaction term was coded 1 if the individual had a mental illness and a co-occurring substance use disorder and 0 otherwise. A significant positive value for this coefficient would indicate that co-occurring diseases have a multiplicative effect on the log odds of treatment, increasing the risk beyond that of an additive effect of both diseases. We included binary variables in the models to indicate the presence of mental illness and of substance use disorder, as well as demographic variables. For each of the three groups defined by substance use disorder and mental illness status, we constructed odds estimates for treatment of each medical disorder—adjusted for age, gender, and race or ethnicity—and calculated the corresponding 95% confidence intervals. The reference group consisted of individuals without mental illness and without substance use disorders. SAS was used for all statistical modeling. Accuracy was assessed by examining the area under the receiver operating characteristic curve.
Papers on Medical Conditions of Persons With Severe Mental Illness
Lisa B. Dixon, M.D., M.P.H.
Over the past five years, a number of forces have converged to focus attention on the unmet medical needs of persons with severe mental illness. The expansion of managed care has required that we answer the question of whether psychiatric care should be carved in or carved out of insurance packages. We have seen that while carve-outs may in some ways ensure better psychiatric care, the medical needs of people with psychiatric disabilities may not be met.
In addition, the newer, atypical antipsychotic drugs have reduced extrapyramidal side effects and in many instances have improved symptoms, allowing patients and their families to tend to other aspects of their lives. At the same time, some of these new agents have been implicated in weight gain and conditions such as type 2 diabetes.
Research is needed to help identify comorbid medical conditions among persons with severe mental illness and to suggest effective interventions. In this issue of Psychiatric Services, a group of six research papers—three articles and three brief reports—focus attention on the comorbid medical conditions of persons with severe mental illness. Another group of such papers will be featured in an upcoming issue.
Using Medicaid data sets, Dickey and her colleagues (see page 861) and Blank and his associates (page 868) demonstrate the increased vulnerability of persons with severe mental illness to HIV infection and other medical conditions. In the former study, substance use disorders greatly enhanced this vulnerability. Cradock-O'Leary and her coauthors (page 874) and Dickerson and her colleagues (page 882) explored differences in receipt of medical care among persons with severe mental illness and found that younger patients and women may receive less intensive care for a given medical condition and may also receive fewer preventive services. The Dickerson study also shows that older women with schizophrenia have poorer health behaviors in terms of smoking and seeking preventive care.
A study by Daumit and her colleagues (page 884) explored the nature of preventive medical care provided in the psychiatric specialty sector and found that relatively few patients received even basic preventive interventions. Finally, Goldberg and his associates (page 879) determined that persons with severe mental illness can reliably report their recent use of medical services.
The results of these studies suggest that there are many challenges to providing high-quality medical care to people with psychiatric disabilities. It is important to find ways to promote healthier lifestyles in this population in order to prevent the onset of somatic illness. We need to optimize both acute and preventive services in the primary care and specialty sectors. Our patients can tell us about their medical needs—we must ask and listen.
Dr. Dixon is associate professor of psychiatry in the Department of Psychiatry, University of Maryland School of Medicine, 701 West Pratt Street, Room 476, Baltimore, Maryland 21201. She is also associate director of the Veterans Affairs Capitol Health Care Network Mental Illness Research, Education, and Clinical Center in Baltimore.
Results
Sociodemographic differences
The sample distribution of gender, age, and race or ethnicity varied considerably by the presence or absence of a psychotic disorder, although the proportion of persons with a substance use disorder in each group was similar. Table 1 summarizes the sociodemographic characteristics of the groups. Persons who were treated for a psychotic disorder were more likely to be male, white, and older than those without a psychotic disorder. The group without any psychotic disorders was drawn entirely from AFDC beneficiaries; their sociodemographic characteristics reflected the AFDC Medicaid population of enrollees—that is, they were more likely to be younger women of a racial or ethnic minority group.
Twelve-month treated prevalence rates
The findings summarized in Table 2 supported our hypothesis that certain treated medical disorders were more prevalent among individuals treated for a psychotic illness than among those who did not have a psychotic illness. In analyses that controlled for age and gender, we found significantly higher frequencies of all eight selected medical disorders among adults with psychoses than among those who did not have a psychotic illness. Furthermore, those with a psychotic disorder were twice as likely to be treated for two or more of the medical disorders we considered.
Given reports that schizophrenia may reduce the risk of lung cancer, we compared the prevalence of this disorder among persons with schizophrenia with that among those with no psychotic disorder or substance use disorder. The small number of individuals with lung cancer in our sample prevented statistical analysis of the findings. Thus we can report only that there were 13 cases (.24 percent) among the 5,467 persons with schizophrenia and three cases (.03 percent) among those with no psychotic disorder or substance use disorder. Even though the group without mental illness was younger, it appears that the risk of lung cancer in the sample was unlikely to be lower for adults with schizophrenia.
Substance use disorders and risk of medical illness
In analyses that were adjusted for age, gender, and race or ethnicity, psychosis alone and psychosis with a comorbid substance use disorder were each independently associated with a greater risk of the eight medical disorders. The results are summarized in Table 3. Of the three groups, the group of patients with a psychotic disorder and a comorbid substance use disorder had the highest adjusted odds for five of the eight disorders: heart disease, asthma, gastrointestinal disorders, skin infections, and acute respiratory disorders. Those without a psychotic disorder who were treated for a substance use disorder had a higher risk of all the disorders except hypertension.
Discussion
The results are consistent with other reports that adults with mental illness have a higher risk of medical disorders than those without mental illness. We found not only that they have a higher likelihood than those with no mental illness of having one of the eight disorders we studied but also that they are more likely to have more than one disorder. The presence of a substance use disorder contributed to the prevalence of five of the medical disorders. These findings also extend the information obtained in earlier studies by providing estimates of the size of the greater risk, reported separately for those with and those without comorbid substance use disorders.
Several factors that increase the risk of medical disorders are known to be directly associated with mental illness. Among them are use of medications that contribute to weight gain, which is associated with diabetes and hypertension; poor attention to personal hygiene, which is associated with skin infections; high rates of smoking, which contributes to asthma, acute respiratory disease, heart disease, and lung cancer; reduced physical activity and fitness, which contributes to hypertension and heart disease; and use of medications with adverse gastrointestinal effects. It is unclear, however, how much these factors alone account for the higher risk of the eight medical disorders. Some unexplained variance associated with mental illness may remain.
This study improved on earlier studies in several ways. The sample was large enough to provide stable frequency distributions for specific diseases, and the analyses controlled for other factors, such as poverty, that increase the risk of medical disorders. Although the study's strength lies in its use of data from a large Medicaid population, some problems with generalizability remain. Having AFDC beneficiaries as the comparison group was not ideal, because these individuals differed in age and gender from the study patients with psychotic disorders. However, statistical controls helped to reduce the case-mix differences and to make the comparisons equivalent. In addition, we had no way of estimating whether individuals with psychotic illness who are not within this Medicaid population would have the same estimated odds ratios for the diseases we studied. Mitigating this problem is the knowledge that the majority of adults with disabling psychotic illnesses are enrolled in Medicaid.
The high rates of these medical disorders, and perhaps others, have implications for how services for persons with severe mental illness are designed. The relative merits of separating mental health services from medical care provided through health plans have been questioned, because it is widely believed that this practice will leave many mentally ill individuals at risk of receiving inadequate medical care (1). People with mental illness are sometimes unwilling to seek medical help, or when they do seek help they frequently have difficulty describing their problems to a physician (19). Several clinically related reasons may explain why this might occur. For example, people with schizophrenia tend to have a high tolerance for pain (20) and thus may be less likely to report pain as a symptom. Psychotic symptoms may interfere with the patient's ability to communicate with the physician, or the physician may focus on the mental illness and miss symptoms related to a medical disorder. Integrating medical and mental health treatment may encourage greater continuity of care and coordination of different treatments but may not improve communication between the physician and the person with mental illness.
The long-standing separation of treatment for medical and mental illness may need to be reconsidered in light of these findings. Unfortunately, most mental health professionals are not trained to identify medical problems or to conduct physical evaluations. Because of this lack of training, some specialized mechanism is needed to bridge the gap between medicine and mental health services to improve the medical treatment of persons with mental illness. At the very least, psychiatrists must be alert to medical problems and take care to ensure that referral to appropriate medical treatment is provided.
A policy question related to access to medical care is whether adequate treatment of mental illness will lead to reductions in medical expenditures. Many studies, assuming a strong relationship between mental illness and medical comorbidity, have attempted to estimate the probability of reducing treatment costs for medical disorders when mental illness is properly identified and treated. These studies, usually referred to as medical offset studies, have hypothesized that increasing expenditures for treatment of mental disorders will result in lower expenditures for medical care (21).
This hypothesis stems from the belief that some medical disorders are better managed by physicians if the patient is less troubled by mental illness. Medical offset might also occur if appropriate psychiatric treatment reduces the number of medical visits for psychosomatic problems or vague physical complaints arising from emotional problems. Many researchers have tried to establish empirical support for this hypothesis, but few have succeeded. In fact, studies are more likely to find higher, not lower, medical care costs for adults treated for mental illness (22).
The dream of offsetting medical expenditures may be difficult to realize because serious medical problems are widespread. To reduce medical expenditures by increasing the intensity of mental health treatment, a focused strategy is needed. The effort could include, for example, specialized interventions tailored for persons with mental illness that might improve self-management of asthma, hypertension, and diabetes and thus might lower treatment costs. Other mechanisms that might reduce medical treatment costs lie in some promising new approaches that combine treatment for psychiatric and substance use disorders for some types of patients (23,24,25). These interventions, however, are likely to result in closer attention to both mental illness and substance use disorders, which in turn will lead to the early identification of medical illnesses among some patients and increase their overall treatment costs. The result may not be lower medical expenditures but better medical treatment.
This study provided an incomplete but compelling picture of the association between common medical disorders, mental illness, and substance use disorders. The next step along this avenue of research might require clinical studies that gather richer information about the patients, their medical histories, and their treatments. However, such research is expensive and difficult to carry out and requires large samples. A better—but also expensive and difficult—strategy would be to enhance the clinical information available in administrative data and to encourage the use of electronic medical records that can be shared among providers. In addition, developing a better understanding of how mental illness results from or leads to specific medical disorders is important for both clinical care and health care policy. Perhaps the most important message of this report is that the development of closer working relationships between medical and mental health professionals must be emphasized.
Acknowledgments
This study was supported by a grant from the Massachusetts Division of Medical Assistance and by grant MH-58288 from the National Institute of Mental Health (NIMH) to Dr. Dickey; grant DA-00326 from the National Institute on Drug Abuse and a grant from the Dr. Ralph and Marian C. Falk Medical Research Trust to Dr. Weiss; and an NIMH Research Infrastructure Support Program award to Dr. Drake. The authors thank Arthur Seigel, M.D., for comments on the manuscript.
Dr. Dickey is affiliated with Harvard Medical School and the department of psychiatry at Cambridge Hospital. Dr. Normand is affiliated with the department of health care policy at Harvard Medical School and the department of biostatistics at the Harvard School of Public Health in Boston. Dr. Weiss is with Harvard Medical School and McLean Hospital in Belmont, Massachusetts. Dr. Drake is affiliated with Dartmouth Medical School and the New Hampshire-Dartmouth Psychiatric Research Center in Lebanon, New Hampshire. Mr. Azeni is with the department of psychiatry at Harvard Medical School. Address correspondence to Dr. Dickey, Cambridge Hospital, 1493 Cambridge Street, Cambridge, Massachusetts 02139 (e-mail, [email protected]). Preliminary findings from this study were presented at a workshop on costs and assessment in psychiatry sponsored by the Section on Mental Health Economics of the World Psychiatric Association, held May 10-12, 2000, in Chicago. This paper is one of several in this issue focusing on the health and health care of persons with severe mental illness.
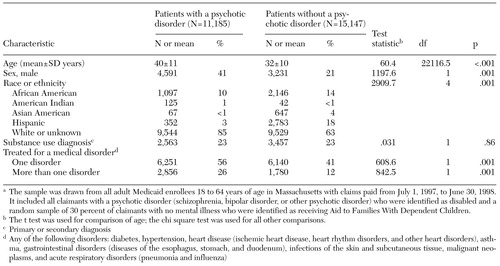 |
Table 1. Sociodemographic characteristics of Medicaid beneficiaries with and without a psychotic disorder in a study of medical morbidity and comorbid substance use disordersa
a The sample was drawn from all adult Medicaid enrollees 18 to 64 years of age in Massachusetts with claims paid from July 1, 1997, to June 30, 1998. It included all claimants with a psychotic disorder (schizophrenia, bipolar disorder, or other psychotic disorder) who were identified as disabled and a random sample of 30 percent of claimants with no mental illness who were identified as receiving Aid to Families With Dependent Children.
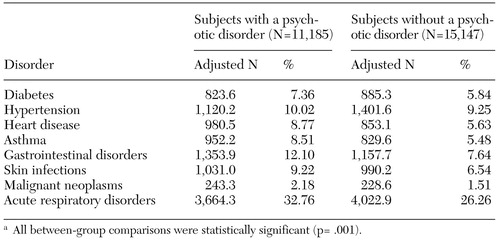 |
Table 2. Twelve-month treated prevalence of eight medical disorders, adjusted for age and gender, among Medicaid beneficiaries with and without a psychotic disordera
a All between-group comparisons were statistically significant (p= .001).
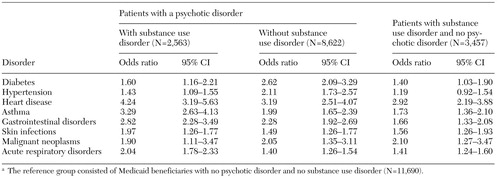 |
Table 3. Risk of eight medical disorders, adjusted for age, gender, and race, among Medicaid beneficiaries with and without a psychotic disorder and a substance use disordera
a The reference group consisted of Medicaid beneficiaries with no psychotic disorder and no substance use disorder (N=11,690).
1. Koran LM, Sox HC Jr, Marton KI, et al: Medical evaluation of psychiatric patients: I. results in a state mental health system. Archives of General Psychiatry 46:733-740, 1989Crossref, Medline, Google Scholar
2. Dixon L, Postrado L, Delahanty J, et al: The association of medical comorbidity in schizophrenia with poor physical and mental health. Journal of Nervous and Mental Disease 187:496-502, 1999Crossref, Medline, Google Scholar
3. Jeste DV, Gladsjo JA, Lindamer LA, et al: Medical comorbidity in schizophrenia. Schizophrenia Bulletin 22:413-430, 1996Crossref, Medline, Google Scholar
4. Eaton WW, Hayward C, Ram R: Schizophrenia and rheumatoid arthritis. Schizophrenia Research 6:181-192, 1992Crossref, Medline, Google Scholar
5. George TP, Sernyak MJ, Ziedonis DM, et al: Effects of clozapine on smoking in chronic schizophrenic outpatients. Journal of Clinical Psychiatry 56:344-346, 1995Medline, Google Scholar
6. Craig TJ, Lin SP: Cancer and mental illness. Comprehensive Psychiatry 22:404-410, 1981Crossref, Medline, Google Scholar
7. Mortensen PB: The incidence of cancer in schizophrenic patients. Journal of Epidemiology and Community Health 43:43-47, 1989Crossref, Medline, Google Scholar
8. Tsuang MT, Perkins K, Simpson JC: Physical diseases in schizophrenia and affective disorder. Journal of Clinical Psychiatry 44:42-46, 1983Medline, Google Scholar
9. Harris AE: Physical disease and schizophrenia. Schizophrenia Bulletin 14:85-96, 1988Crossref, Medline, Google Scholar
10. Gulbinat W, Dupont A, Jablensky A, et al: Cancer incidence of schizophrenia patients: results of record linkage studies in three countries. British Journal of Psychiatry 161(Oct suppl):75-83, 1992Google Scholar
11. Baldwin JA: Schizophrenia and physical disease: a preliminary analysis of the data from the Oxford Record Linkage Study, in The Biochemistry of Schizophrenia and Addiction: In Search of a Common Factor. Edited by Hemmings G. Lancaster, England, MTP, 1980Google Scholar
12. Lacro JP, Jeste DV: Physical comorbidity and polypharmacy in older psychiatric patients. Biological Psychiatry 36:146-152, 1994Crossref, Medline, Google Scholar
13. Zornberg G, Weiss R: Substance-related disorders, in Acute Care Psychiatry: Diagnosis and Treatment. Edited by Sederer LI, Rothschild AI. Baltimore, Williams & Wilkins, 1997Google Scholar
14. Drake RE, Osher FC, Wallach MA: Alcohol use and abuse in schizophrenia: a prospective community study. Journal of Nervous and Mental Disease 177:408-414, 1989Crossref, Medline, Google Scholar
15. Osher FC, Drake RE, Noordsy DL, et al: Correlates and outcomes of alcohol use disorder among rural outpatients with schizophrenia. Journal of Clinical Psychiatry 55:109-113, 1994Medline, Google Scholar
16. Jackson CA, Manning WG Jr, Wells KB: Impact of prior and current alcohol use on use of services by patients with depression and chronic medical illnesses. Health Services Research 30:687-702, 1995Medline, Google Scholar
17. Dickey B, Azeni H, Weiss R, et al: Schizophrenia, substance use disorders, and medical co-morbidity. Journal of Mental Health Policy and Economics 3:27-33, 2000Crossref, Medline, Google Scholar
18. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
19. Holmberg S: Physical health problems of the psychiatric client. Journal of Psychosocial Nursing and Mental Health Services 26:35-39, 1988Medline, Google Scholar
20. Dworkin RH: Pain insensitivity in schizophrenia: a neglected phenomenon and some implications. Schizophrenia Bulletin 20:235-248, 1994Crossref, Medline, Google Scholar
21. Olfson M, Sing M, Schlesinger HJ: Mental health/medical care cost offsets: opportunities for managed care. Health Affairs 18(2):79-90, 1999Google Scholar
22. Simon GE, VonKorff M, Barlow W: Health care costs of primary care patients with recognized depression. Archives of General Psychiatry 52:850-856, 1995Crossref, Medline, Google Scholar
23. Weiss RD, Najavits LM: Overview of treatment modalities for dual diagnosis patients: pharmacotherapy, psychotherapy, and twelve-step programs, in Dual Diagnosis: Substance Abuse and Comorbid Medical and Psychiatric Disorders. Edited by Kranzler HR, Rounsaville BJ. New York, Marcel Dekker, 1998Google Scholar
24. Drake RE, Noordsy DL, Ackerson T: Integrating mental health and substance abuse treatments for person with chronic mental disorders, in Double Jeopardy: Chronic Mental Illness and Substance Use Disorders. Edited by Lehman AF, Dixon LB. Newark, NJ, Gordon and Breach, 1995Google Scholar
25. Drake RE, McHugo GJ, Noordsy DL: Treatment of alcoholism among schizophrenic outpatients:4-year outcomes. American Journal of Psychiatry 150: 328-329, 1993Google Scholar



