Effects on Processes and Costs of Care Associated With the Addition of an Internist to an Inpatient Psychiatry Team
Abstract
OBJECTIVE: This study examined the effects of collaboration between an internist and psychiatrists on the processes and cost of care among psychiatric inpatients. METHODS: A randomized controlled study was performed on the psychiatric inpatient units of an academic medical center. All inpatients who were admitted to the units between March 2001 and January 2002 were asked to participate in the study. Patients in the intervention group met with an internist who participated in their care by communicating with the patients' primary care physicians, assessing needs, updating appropriate health maintenance services, managing chronic and acute medical problems, and attending hospital work rounds. Patients in the usual-care group received usual care. The processes of care were measured by examining 17 categories that involved assessment of needs, coordination of care, and completion of health maintenance services. Resource use was measured by examining hospital charges and length of stay. RESULTS: A total of 139 adults participated in the study: 55 were in the intervention group and 84 were in the usual-care group. Patients in the intervention group showed significant improvement in 12 of the 17 categories of the processes of care. Overall, no differences were found in hospital charges or length of stay. CONCLUSIONS: Adding an internist to an inpatient psychiatric team is an effective way of improving care for this traditionally underserved population without increasing cost.
Psychiatric patients are medically underserved in many ways (1). Compared with persons without psychiatric diagnoses, persons with mental illness have more difficulty gaining access to health care (2), have more chronic medical conditions (3), are less likely to follow guidelines for prevention (4), and are at increased risk of sickness (5). Even persons with mental illness who get care for their chronic medical problems are less likely to use preventive services (6,7,8). Because of these multiple barriers we must develop programs to better address the needs of our patients, their providers, and the systems that support them.
Although several interventions have been suggested to improve health care for persons with chronic mental illness—including case management (9) and training psychiatrists to provide primary care (10)—the only interventions that have been tested have been co-locating psychiatric and primary care services (11) and medical-psychiatric units (12,13). Although each of these interventions may be effective in its context, we believe that improvements in care can be achieved at many points in the cycle of care. Therefore, we offer another opportunity to provide preventive health services to this population: collaboration between an internist and psychiatrists during the inpatient stay. The opportunities offered by this approach include the availability of comprehensive services and staff and the use of the downtime that many patients experience while hospitalized.
What has been called an "interfaith marriage," a collaboration of two groups of physicians who do not often work together, offers advantages to both groups (14). This pilot study added a board-certified internist to the psychiatric teams of the inpatient units of the 562-bed hospital that is allied with the University of Vermont College of Medicine. We tested the hypothesis that this collaboration would improve the processes of care without increasing cost.
Methods
The study was a randomized controlled trial on the inpatient psychiatric units of Fletcher Allen Health Care in Burlington, Vermont. This work was approved by the institutional review board of the University of Vermont College of Medicine. Data were collected from March 2001 through January 2002.
Participants and site
All patients who were 18 years and older and were admitted to the two inpatient psychiatric units from March 2001 through January 2002 were eligible for this study. Both units hold 24 beds. One of these floors holds 12 beds and is a locked unit. Patients were excluded from our study if they required medical consultation before they could be randomly assigned into study groups. Patients on these units had the full range of diagnoses for which hospitalization is required. We defined patient discharge as transfer to home, a community care bed, the state hospital, or another unit within the hospital complex for a medical or surgical reason.
Study design
After the study coordinator obtained consent from participants, she determined whether their hospital records contained a list of physical and mental problems, current medications, review of symptoms, and the Global Assessment of Functioning (GAF) score (15); she also obtained information to complete the Charlson Comorbidity Index (16). She also administered the Short-Form-36 Health Survey (SF-36), a general functional status measure (17,18), and the Behavior and Symptom Identification Scale (BASIS-32), a functional status and symptom instrument specific to mental health (19). Patients were then randomly assigned to a usual-care group or an intervention group.
Participants in the usual-care group were cared for by the psychiatric house staff who had rotations in the inpatient unit that lasted for a month and who saw patients daily and followed their progress by one of the four psychiatric attending physicians who were permanently assigned to the units. Consultations from medical specialists were obtained by using the usual hospital services.
Participants in the intervention group were seen within 24 hours of admission by the internist who was involved with the study. The internist worked in conjunction with the usual-care team. He obtained a comprehensive medical history from the patient, performed a physical examination, and communicated with the primary care provider about health maintenance services, chronic medical problems, and current medications. On the basis of this information the list of medical problems and current medications was updated, and arrangements were made for completion of the health maintenance services specified by the U.S. Preventive Services Task Force (20), either as an inpatient or after discharge. In addition, the internist ordered specialty consultations as needed, made plans for alcohol and nicotine abatement, managed acute and chronic nonpsychiatric illnesses during the stay, and attended work rounds daily. At discharge, the internist again communicated with the primary care provider about new medications, medical problems, and plans for the completion of health maintenance services, for example, scheduling a mammogram.
After the patient was discharged, the research assistant reviewed the chart for evidence that appropriate health maintenance services had been initiated or completed.
Outcome variables
We chose outcome variables from two domains: processes of care and resource use. We looked at processes of care in terms of the functions of a general internist: developing a needs assessment that documented medical problems and current medications, updating appropriate health maintenance services, and coordinating care with outpatient primary care providers.
Developing a needs assessment involved updating the list of problems to include physical problems, psychosocial issues, family risk factors, allergies, and environmental problems; updating a current medication list; and looking for potential adverse drug reactions. Appropriate health maintenance services were chosen on the basis of recommendations of the U.S. Preventive Services Task Force (20). These services were either completed during the hospitalization or arranged for at discharge. Coordination of care involved calling primary care providers at admission and discharge. In all, 17 individual elements of the processes of care were recorded. Rates for the individual element were calculated as the number of patients who received the element divided by the number for whom it was appropriate, either by age, risk, or not having been recorded by the primary care provider, multiplied by 100. Summary scores for three subdomains—needs assessment, health maintenance, and coordination of care—were calculated as the percentage of appropriate elements that were completed for each patient.
We defined resource use as the total charges reported in the hospital's administrative database that is used for billing purposes, as well as length of stay. In addition, we looked at use of hospital inpatient days and emergency department visits for a year after discharge, although data were not available for all patients.
Statistical analyses
Because many of the variables we studied were not normally distributed, we used nonparametric statistics. Statistical significance for unadjusted comparisons between active and usual-care groups was calculated by using the Wilcoxon rank sum test for continuous outcomes and the chi square test or Fisher's exact test for dichotomous outcomes. To adjust for baseline differences between the two groups, we used robust linear regression with Huber iterations followed by biweight iterations (21). STATA 8.2 was used to analyze the data.
Results
Baseline characteristics
During the study period 272 patients were admitted to the psychiatric units. Twelve required medical consultation before they were to be randomly assigned into study groups, and 121 refused to participate in the study. The remaining 139 patients were randomly assigned into groups: 55 patients were assigned to the intervention group and 84 patients were assigned to the usual-care group. An administrative error resulted in unequal group sizes, but that did not violate randomness or introduce treatment assignment bias. The groups' baseline characteristics are shown in Table 1. No significant differences were found between the groups in age, sex, diagnosis, functioning, identification of a primary care provider, or admission to a psychiatric unit during the previous year. Although a majority of patients did not have any comorbid medical conditions, patients in the intervention group had slightly more of these conditions (p=.023).
Compared with participants, patients who were ineligible for the study or refused enrollment were older (mean±SD age of 37.2±12.3 years compared with a mean of 43.3±17.9 years; t=-3.3, df=270, p=.001) and had more comorbid medical conditions (mean Charlson score of .38±.77 among participants compared with a mean score of .19±.49 among nonparticipants; t=-2.32, df=270, p=.016). Participants and nonparticipants did not differ in terms of gender (35 percent men among participants compared with 41 percent men among nonparticipants), GAF score (mean score of 42±14 among participants compared with a mean score of 43±16 among nonparticipants), or whether they had a primary care provider (86 percent among participants compared with 81 percent among nonparticipants).
Outcomes
As shown in Table 2, the intervention group had better scores on every individual element of the processes of care than the usual-care group. Twelve of 17 individual comparisons were statistically significant. The summary scores for needs assessment, health maintenance, and coordination of care were all significantly better in the intervention group.
Although the length of stay was shorter in the intervention group, the difference was not statistically significant. Total hospital costs were similar in the two groups (Table 2). There were no significant differences in use of hospital services after discharge (mean of 4.2±11.3 inpatient-days compared with a mean of 4.4±19.6 inpatient-days) or emergency department visits (mean of 1.1±3.2 visits compared with a mean of .7±2.2 visits).
Discussion
This randomized, controlled trial of the effect of an internist's collaborating with an inpatient psychiatry team demonstrated significant improvements in the processes of care with no overall change in costs. The expenses generated by having the internist manage acute and chronic medical conditions and provide preventive services were offset by savings in other areas. Because length of stay was only minimally affected, we posit that having a general internist wisely overseeing the ordering of tests and consultations (for example, not ordering stress tests for noncardiac chest pain) produced efficiency and economy of care.
It could be argued that some of the needs assessment for preventive services done by the study internist could be performed by the psychiatric teams and that implementing health maintenance services (for example, smoking and alcohol plans) could be improved with systems changes. Indeed, a new database has been developed on these units to address some of these issues. However, we believe that the coordination of care offered in this type of collaboration is a unique contribution.
The study had several limitations. A large number of eligible patients refused to participate in the study, many because of fatigue or suspicion. It is not clear whether these patients would have refused medical attention by the internist if it was offered in a nonresearch, nonacute setting. We are also unsure of adherence to follow-up visits or tests.
Data were collected for patients at one academic medical center, and the results may not generalize to patients at other locations. However, the range of medical complexity and psychiatric diagnoses found in our center appears to be typical of that found in general hospitals in the United States.
Our estimates of the resources used are based on hospital charges. Although not perfectly representative of costs, they were recorded in identical fashion for both study groups and therefore provide an unbiased comparator. Some of the tests associated with prevention were arranged to take place after hospitalization, and we have no way of knowing whether these were done. Often these were the more expensive tests, for example, mammograms. The costs of these preventive measures were not factored into the study, because they were not borne by the hospital. However, these are appropriate costs of good care and are routinely covered by insurers as part of their obligations to care for these patients.
Several potentially important outcomes were not measured in this study. For example, transfers to other units for more intensive or specialized care may have been decreased by the presence of an internist, and patients with more medical problems may have been admitted to the psychiatry units because of his presence.
Conclusions
This randomized, controlled trial demonstrated that collaboration between an internist and psychiatrists resulted in improved patient care with no overall difference in the cost of care.
Acknowledgments
The authors thank Richard A. Bernstein, M.D., John Ives, M.D., Philip Wu, M.D., Suzanne Kennedy, M.D., and Christina Bodor, M.D. This project was supported by a Research Development Grant from Fletcher Allen Health Care and their office of patient oriented research.
Dr. Rubin and Dr. Littenberg are affiliated with the division of general internal medicine at the University of Vermont College of Medicine, 371 Pearl Street, Burlington, Vermont 05401 (e-mail, [email protected]). Dr. Ross is with the School of Nursing at the University of Vermont in Burlington. Dr. Wehry is with the department of psychiatry at the College of Medicine at the University of Vermont in Burlington. Ms. Jones is with Fletcher Allen Health Care in Burlington.
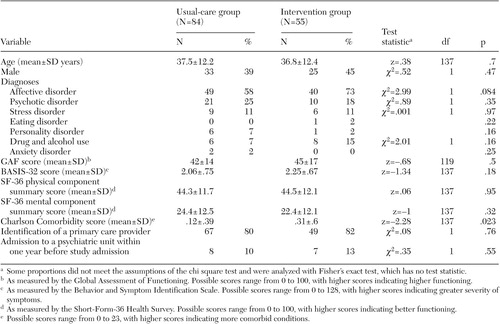 |
Table 1. Baseline characteristics of 139 adult inpatients, by whether they received usual care or treatment from an internist who coordinated care with the psychiatric team
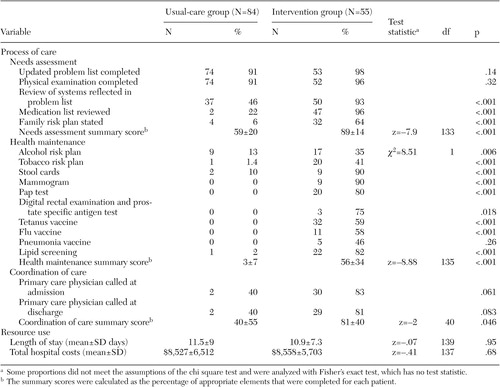 |
Table 2. Outcomes of 139 adult inpatients, by whether they received usual care or treatment from an internist who coordinated care with the psychiatric team
1. Roca R, Breakey W: Medical care of chronic psychiatric outpatients. Hospital and Community Psychiatry 38:741–749, 1987Abstract, Google Scholar
2. Druss BG, Rosenheck RA: Mental disorders and access to care in the US. American Journal of Psychiatry 155:1775–1777, 1998Link, Google Scholar
3. Blank MB, Mandell DS, Aiken L, et al: Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatric Services 53:868–873, 2002Link, Google Scholar
4. Druss BG, Rosenheck RA, Desai MM, et al: Quality of preventive medical care for patients with mental disorders. Medical Care 40:129–136, 2002Crossref, Medline, Google Scholar
5. Dickey B: Medical morbidity, mental illness, and substance use disorders. Psychiatric Services 53:861–867, 2002Link, Google Scholar
6. Carney CP, Allen J, Doebbeling BN: Receipt of clinical preventive medical services among psychiatric patients. Psychiatric Services 53:1028–1030, 2002Link, Google Scholar
7. Carney CP, Yates WR, Goerdt CJ, et al: Psychiatrists' and internists' knowledge and attitudes about delivery of clinical preventive medical services. Psychiatric Services 49:1594–1600, 1998Link, Google Scholar
8. Daumit GL, Crum RM, Guallar E, et al: Receipt of preventive medical services at psychiatric visits by patients with severe mental illness. Psychiatric Services 53:884–887, 2002Link, Google Scholar
9. Carter AM: Case management in psychiatric inpatient recapture. Military Medicine 162:44–50, 1997Crossref, Medline, Google Scholar
10. Golomb BA, Pyne JM, Wright B, et al: The role of psychiatrists in primary care of patients with severe mental illness. Psychiatric Services 51:766–773, 2002Link, Google Scholar
11. Druss BG, Rohrbaugh RM, Levinson CM, et al: Integrated medical care for patients with serious psychiatric illness: a randomized trial. Archives of General Psychiatry 58:861–868, 2001Crossref, Medline, Google Scholar
12. Kathol RG, Stoudemire A: Medical psychiatric units, in Textbook of Consult Liaison Psychiatry, 2d ed. Edited by Ramdell J. Washington, DC, American Psychiatric Press, 2000Google Scholar
13. Kishi Y, Kathol R: Integrating medical and psychiatric treatment in an inpatient medical setting. Psychosomatics 40:345–355, 1999Crossref, Medline, Google Scholar
14. Schuyler D, Davis K: Primary care and psychiatry: anticipating an interfaith marriage. Academic Medicine 74:27–32, 1999Crossref, Medline, Google Scholar
15. Endicott J, Spitzer RL, Fleiss Jl, et al: The Global Assessment Scale. Archives of General Psychiatry 33:766–771, 1976Crossref, Medline, Google Scholar
16. Charlson ME, Pompei P, Ales KL: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Disease 40:373–383, 1987Crossref, Medline, Google Scholar
17. Ware J: SF-36 Health Survey and Interpretation Guide. Boston, Health Institute, 1993Google Scholar
18. Ware J: SF-36 Physical and Mental Health Summary Scales: A User's Manual. Boston, MA, NEMC, 1994Google Scholar
19. Eisen S: Behavior and Symptom Identification Scale (BASIS-32), in Outcome Assessment in Clinical Practice. Edited by Sederer L, Dickey B. Baltimore Md, Williams and Wilkins, 1996Google Scholar
20. U.S. Preventive Services Task Force. Guide to Clinical Preventive Services, 2nd ed. Alexandria, Va, International Medical Publishing, 1996Google Scholar
21. Hamilton LC: Regression with Graphics. Pacific Grove, Calif, Brooks/Cole Publishing Company, 1992Google Scholar



