Psychiatrists' and Internists' Knowledge and Attitudes About Delivery of Clinical Preventive Medical Services
Abstract
OBJECTIVE: Changes in the health care environment have placed a greater responsibility on psychiatrists to deliver basic primary care services. The study assessed baseline knowledge and attitudes about clinical preventive medical services among psychiatric faculty and psychiatric residents at a tertiary care medical center. METHODS: Residents and faculty in psychiatry and general internal medicine completed a structured questionnaire, including 20 case scenarios, that assessed their baseline knowledge of clinical preventive medical services, their attitudes concerning delivery of those services, and their beliefs about the effectiveness of those services in changing patients' behavior. The case scenarios and knowledge questions were based on the clinical preventive medical services recommendations outlined by the U. S. Preventive Services Task Force. RESULTS: Psychiatrists reported more frequent assessment of and counseling about the use of illicit drugs and weapons, and internists were more likely to query about measures related to physical health such as cancer screening and immunizations. The two groups reported similar attitudes toward the need for and the efficacy of preventive medical services. Commonly cited barriers to the delivery of preventive care included lack of time and education. Psychiatrists scored reasonably well on baseline knowledge about guidelines for preventive medical services, particularly given their recent lack of specific education in these matters. CONCLUSIONS: Psychiatrists believe clinical preventive services are important and express interest in their delivery. Additional educational interventions are needed to train psychiatrists in clinical preventive services to avoid missed clinical opportunities for intervention in psychiatric populations that may have poor access to other medical care.
As the health care environment evolves to place increased emphasis on the primary care delivery of medical and psychiatric services, the traditional role of the psychiatrist may change to include more comprehensive care of the mentally ill patient. Education of primary care providers about psychiatric diagnoses and treatment has been widely advocated recently. However, rarely is the psychiatrist trained to provide basic primary care to patients. Pilot programs designed to train psychiatrists to serve as the principal or primary physician for selected populations of psychiatric patients are under way (1,2,3).
It is noteworthy that as many as one-third of homeless mentally ill patients have concomitant medical illness (4). In addition, standardized mortality rates for both natural and unnatural causes of death are higher among psychiatric patients than the general population (5,6,7,8). Many natural and unnatural causes of morbidity and mortality may be preventable with health care interventions.
The goal of primary prevention is to avoid the development of a disease or disorder by eliminating causative agents and decreasing reversible risk factors. Secondary prevention involves the early identification and prompt treatment of an illness or disorder. Typically, preventive care is delivered by primary caregivers such as general internists, family practitioners, pediatricians, and obstetrician-gynecologists. The psychiatrist has not traditionally been considered a primary care provider.
However, the psychiatrist may be in an unique position to deliver needed preventive services to populations of patients who may be unlikely to receive these services, including homeless mentally ill persons, institutionalized persons, and those whose psychiatric disease makes it financially or logistically difficult for them to receive regular medical care. Important potential sites for the delivery of clinical preventive medical services by mental health care personnel might include community mental health centers, homeless shelters, jails, and state psychiatric institutions.
The U. S. Preventive Services Task Force has recommended that clinicians take every opportunity to deliver preventive medical services, especially to persons with limited access to care, because those at greatest risk for many preventable causes of premature disease and disability, such as cervical cancer, tuberculosis, human immunodeficiency virus infection, and poor nutrition, are the same individuals least likely to receive adequate preventive services (9). Certainly, this guideline may apply to many persons with chronic psychiatric illness.
To determine whether psychiatrists in training and psychiatry faculty may be interested in learning about and delivering clinical preventive medical services, we did a baseline assessment of psychiatrists' attitudes about delivering preventive medical services and their knowledge of current preventive care guidelines. The survey was done in a department of psychiatry at a university teaching hospital. Responses from psychiatric faculty and residents were compared with those from their counterparts in the division of general internal medicine at the same institution.
Methods
Respondents
Residents and faculty in an academic psychiatry program at a tertiary medical center were asked to complete a validated questionnaire designed to assess attitudes toward the delivery of preventive medical care and baseline knowledge of preventive care recommendations (9,10,11). Preventive care guidelines were based on current recommendations by the U.S. Preventive Services Task Force (9).
Participation was entirely voluntary and was requested through a cover letter explaining the study and its procedures. The questionnaire, cover letter, and procedure for participation were approved by the institutional human subjects review committee. Completion of the questionnaire was considered written informed consent.
A total of 36 psychiatric residents and 25 psychiatric faculty were asked to complete the questionnaire during February 1996. A total of 151 internal medicine residents and 17 general internal medicine faculty who were asked to complete a nearly identical questionnaire at approximately the same time served as the comparison group.
Survey instrument
The survey instrument was divided into four major sections assessing subjects' demographic characteristics and training, practice patterns, professional outlook, and experience with barriers to and resources for providing preventive services.
Demographic and training factors requested by the instrument included age, gender, number of years of practice or training, and year of medical school graduation.
Data requested on practice patterns included time spent in ambulatory and inpatient care and the frequency of asking about and providing advice about preventive services. These survey items were selected by a panel of four academic generalists, based on the U.S. Preventive Services Task Force guidelines and their relative importance in preventing morbidity and mortality.
Subjects were asked how often, during the past three months, they had asked about or assessed several areas associated with preventive services as part of the examination of or history taking with new patients. These areas were alcohol use, diet, exercise, immunization history, history of screening for colon cancer, use of seat belts, number of recent sexual partners, tobacco use, illicit drugs, use of female contraceptives, use of male contraceptives, history of Pap tests for women age 18 and older, history of mammograms for women age 50 and older, and exposure to ultraviolet light and use of sunscreens.
Frequency for these areas was ranked on a 7-point Likert-type scale on which the anchor points were never, or 0 percent of the time (scored 1); rarely, or between 1 and 20 percent of the time (scored 2); sometimes, or between 21 and 40 percent of the time (scored 3); about half the time, or between 41 and 60 percent of the time (scored 4); often, or between 61 and 80 percent of the time (scored 5); usually, or between 81 and 99 percent of the time (scored 6); and always, or 100 percent of the time (scored 7).
Respondents were next questioned about the frequency of advice delivered to patients. They were asked how often over the past three months, when they saw an adult patient in the clinic, they advised the patient about several health-related preventive measures, including exercising regularly, increasing consumption of fruits and vegetables, decreasing dietary fat consumption, always using a seat belt when operating or riding in a motor vehicle, wearing a safety helmet when operating or riding a motorcycle or bicycle, avoiding alcohol when driving, and avoiding loaded or unlocked firearms in the home. Answers were given on the same 7-point Likert-type scale.
Preventive counseling related to use of tobacco was assessed with a question that asked respondents how often over the last three months, when they saw a patient who smoked cigarettes, did they advise the patient to quit smoking, advise setting a specific "quit date," see or call the patient near the quit date, refer the patient to a group clinic or intensive smoking cessation program, prepare the patient for withdrawal symptoms, and prescribe a nicotine patch or gum. Responses were given on the same 7-point Likert-type scale.
The third section of the survey assessed respondents' attitudes toward preventive medical counseling by asking them to rate their own effectiveness in changing their patients' behavior in the areas of alcohol reduction, smoking cessation, exercise, safe sex practices, and diet. For each area, physicians were asked to assess whether they were minimally effective (scored 1), somewhat effective (scored 2), quite effective (scored 3), or extremely effective (scored 4). They were also given the option to respond "I never do this." This response was not scored.
Twenty questions depicting different clinical scenarios were used to assess overall knowledge about clinical preventive services. The 20 scenarios included questions such as the recommended frequency for a Pap smear and mammogram for a normal-risk 50-year-old woman and a normal-risk woman under age 35 and the recommended frequency of testing blood pressure and cholesterol and administering the graded-exercise cardiac stress test. Appropriate delivery of the pneumococcal pneumonia vaccine was also questioned. Knowledge scores were tabulated by summing the correct answers for a maximum score of 20.
The fourth section of the survey assessed the extent to which barriers such as lack of time, lack of allied health personnel, lack of prompts, lack of patients' interest, uncertainty about which preventive medical services to provide, and lack of educational materials prevented the physician from providing effective health promotion. The amount of medical education in clinical preventive medical services received in the last six months was categorized in terms of informal and formal hours ranging from none to greater than 12 hours.
The reliability and validity of the instrument were recently reported (12). Copies of the survey instrument are available from the first author.
Statistical analysis
Statistical analysis was conducted using SPSS (13). Categorical variables were compared using the chi square test or Fisher's exact test. Continuously distributed factors, such as the overall knowledge score, were compared using Student's t test for normally distributed variables. Variables not normally distributed were compared using the Wilcoxon rank-sum test. Alpha was set at .05, and all p values were two-tailed.
Results
The response rates among the psychiatric residents and psychiatric faculty were similar. Twenty-eight of 36 residents, or 77 percent, and 16 of 25 faculty, or 64 percent, responded to the survey. Ninety-seven of 151 internal medicine residents, or 64 percent, and 15 of 17 internal medicine faculty, or 88 percent, responded, for an overall response rate of 67 percent for internal medicine residents and faculty.
Respondents from psychiatry had an average age of 35.9±10.9 years, compared with 31±7.3 years for respondents from internal medicine (z=-4.16, p<.001). The average number of years since receipt of their medical degree was 4±7.1 years for the psychiatrists and 9±10.1 for the internists (z=-3.99, p<.001). In both specialties, the male to female ratio was about two to one. Table 1 shows selected characteristics of the two groups.
Asking about preventive measures
As Table 2 shows, internists were more likely than psychiatrists to report that they had inquired about a new patient's diet, exercise habits, and history of immunization, colon cancer screening, Pap smears, and mammograms. Psychiatrists, however, reported that they inquired more frequently about patients' number of recent sexual partners and illicit drug use. Male patients were rarely asked, and female patients were only sometimes asked, about contraceptive use by both groups of providers. Both groups reported that they nearly always inquired about alcohol use. Both groups rarely asked patients about seat belt use.
Counseling
As Table 3 shows, psychiatrists were more likely to advise patients to avoid using alcohol when driving. Psychiatrists were also more likely to advise patients to avoid loaded or unlocked firearms in the home. Internists were more likely to report that they made dietary and exercise recommendations. Both groups rarely advised patients to use seat belts or safety helmets.
Tobacco use
Compared with psychiatrists, internists inquired more frequently about tobacco use (mean±SD frequency score=6.6±.7 for internists and 5.5±1.9 for psychiatrists; z= -3.56, p<.001) and were more likely to advise patients to quit smoking (6.3±1.1 for internists and 4.3±2 for psychiatrists; z=-6.2, p<.001). Internists were also more likely to use measures to help patients stop smoking (for example, advising the patient to stop smoking, setting a specific "quit date," seeing or calling the patient near the quit date, referring the patient to a smoking cessation program, preparing the patient for withdrawal symptoms, and prescribing nicotine replacement therapy.)
Internists believed that they were more effective in changing patients' smoking behaviors than psychiatrists did (1.9±.7 for internists and 1.7±1.1 for psychiatrists; t=1.67, df=151, p=.09), but there was no difference between groups in perceived ability to reduce patients' alcohol intake. Both groups reported that they were only minimally to somewhat effective in changing patients' health risk behaviors.
Knowledge
Psychiatric residents and faculty had a mean knowledge score of 9.5±6.6 correct answers, compared with 16.2±2.2 for the internal medicine residents and faculty (z=-7.3, p< .001). There were no differences in knowledge scores between internal medicine faculty and internal medicine residents and between psychiatric faculty and residents. For both groups the overall knowledge score was positively related to the amount of preventive health education received in the last six months (r=.271, p<.001). As Figure 1 shows, most psychiatrists, or 67 percent, reported receiving less than one hour of training during that period.
Barriers and attitudes
Both groups noted that lack of time was a major barrier to providing effective health promotion. Fifty-one percent of psychiatrists but only 15 percent of internists reported that uncertainty about what preventive services to provide was a major barrier (t=-2.3, df=151, p<.001). The overall knowledge scores were inversely related to the degree of uncertainty about what services to provide (r=-.394, p<.001). Both groups agreed that more professional education about preventive care would be helpful.
Psychiatrists and internists shared similar beliefs about the need for clinical preventive medical services and also had similar attitudes about barriers to effectively delivering those services. However, both groups believed that they were only minimally to somewhat effective in changing patients' behavior with respect to alcohol reduction, smoking cessation, exercise, safe sex, and diet. However, compared with psychiatrists, internists believed they were more effective in changing behaviors related to smoking (1.9±.7 for internists and 1.7±1.1 for psychiatrists; t=1.67, df=151, p=.09), exercise (2.11±.7 for internists and 2.02±1.5 for psychiatrists; z=-2.4, p=.017, and diet (2.2± .87 for internists and 2±1.5 for psychiatrists; z=-3.36, p<.001). The two groups did not differ in their perceived ability to affect patients' alcohol or safe sex practices.
Discussion and conclusions
This study provided a baseline assessment of psychiatrists' knowledge, attitudes, and self-reported delivery of clinical preventive medical services and contrasted the findings with those for a group of primary care (internal medicine) physicians. The results provide a controlled assessment of psychiatrists' attitudes and knowledge about preventive medical services, an integral part of primary care medicine.
The importance of screening and of delivering preventive services such as immunizations is profound. For instance, influenza is considered responsible for 20,000 or more excess deaths during each of ten epidemics occurring in the 20-year period before 1990 (10). The estimated direct savings derived from influenza immunization per individual ranges from $21 to $235, with cumulative savings of nearly $5 million (14).
It is well documented that clinicians often fail to provide recommended clinical preventive medical services. (15,16,17,18,19,20). Reported barriers to care include insufficient time, inadequate reimbursement, clinicians' lack of interest and knowledge, patients' lack of knowledge and involvement, and lack of availability of systems to promote delivery of preventive medical services (9,10).
Patients with a regular source of care are more likely to receive recommended preventive services (21). There is a strong and consistent association between having a physician as the most useful source of information and having received clinical preventive medical services (22). Fox and associates (23) found that the most important factor predicting whether a woman had ever had a mammogram was whether her physician had talked to her about mammography. Patients' refusal also plays an important role in the receipt of preventive medical services (24,25).
Although psychiatric and internal medicine residents and faculty shared similar beliefs about the delivery of clinical preventive medical services, they reported delivering such services at different rates and with different levels of confidence. Internists were more likely to gather historical information on aspects of physical health such as immunization status and cancer screening. Both groups reported that they nearly always assess alcohol use, but they differed in assessment of cigarette smoking and illicit drug use.
The psychiatrists reported that they rarely actually advised or counseled patients to quit smoking. Psychiatrists may believe that smoking may provide some benefit to specific groups of psychiatric patients such as patients with schizophrenia, or that smoking cessation may trigger a major depressive episode in those with a history of depression (26,27). Given that smoking among those with mental illness and mental retardation has been associated with higher rates of alcohol use, use of other substances, and sexual activity (28), assessment and counseling related to tobacco use should be considered. Addington and colleagues (29) have reported that even patients with schizophrenia may be motivated to engage in smoking cessation interventions.
Psychiatrists reported that they do inquire about and are interested in many clinical preventive medical services. Despite reported limited education in these matters, psychiatrists had a reasonably good level of knowledge. Psychiatrists reported little training in clinical preventive medical services and stated that lack of training was a major barrier to delivery. Lack of training may also contribute to the tendency of psychiatric house staff and faculty to order more tests and generate more costly work-ups of patients with medical problems, compared with internal medicine and family practice providers (30). Clearly defined educational guidelines for delivery of clinical preventive medical services in psychiatric settings may result in improved delivery and cost savings.
The majority of psychiatrists surveyed in this study spent little time in ambulatory care, and only one set of questions—about frequency of advising patients on preventive health measures—specifically addressed interactions with clinic patients. However, both inpatient and outpatient psychiatric settings provide excellent opportunities to address preventive services. For example, mentally ill persons with poor access to outpatient care should be assessed while inpatients. The inpatient hospitalization may be the ideal time to provide vaccinations. Inpatients can also benefit from counseling about use of tobacco and alcohol and about safety and dietary practices. Failure to deliver preventive care at psychiatric evaluations and follow-up should be considered missed opportunities for prevention and intervention (11).
Although the data do not address the issues of who should provide preventive services and when they should be provided, they are important concerns. The answers to these questions may vary in different practice settings. Patients enrolled in a psychiatric clinic should be asked at the initial visit whether they regularly see a primary care provider who delivers preventive services such as blood pressure checks and immunizations. If patients are able to identify such a caregiver, the mental health provider can offer counseling in areas related to mental health such as alcohol use, tobacco use, and sexual risk factors. A similar assessment can be performed for psychiatric inpatients. If the patient does not have a regular provider for primary medical care, the psychiatric team may need to assume responsibility for delivering clinical preventive medical services. Referral to medical clinics should be made if the patients' health status dictates.
Automated systems to provide clinical prompts or computer-generated reminders may be particularly useful for the mental health provider, as they have been shown to be for primary care providers. Including preventive care checklists with patients' medical records has been shown to increase rates of delivery in primary care (31). In addition, computer-generated reminders have been shown to affect the delivery of clinical preventive services to ambulatory patients (32,33,34).
Specific patient populations may benefit from psychiatric delivery of clinical preventive medical services. Persons identified as at high risk for human immunodeficiency virus infection should receive counseling about disease prevention from all health care providers. Persons at high risk for pneumococcal pneumonia and influenza, including those who are substance abusers and elderly persons, should receive appropriate vaccinations. Mentally ill homeless persons may benefit from a tetanus vaccine booster, although there are no data on the importance of this measure for this group. Injection drug users and those who are sexually promiscuous may benefit from hepatitis B vaccination. Alcohol and smoking cessation counseling should be provided to all persons who abuse these substances. Collaboration between agencies such as the U.S. Preventive Services Task Force and the American Psychiatric Association may be needed to design guidelines for specific populations of psychiatric patients, including persons with alcohol dependence, substance abuse, and chronic psychotic disorders.
This study is limited by the self-report nature of the questionnaire. In a survey of family practice physicians, Montano and Phillips (18) found that respondents tended to report higher rates of screening than were confirmed by a chart audit. Their results suggest either that physicians may report providing more services than they actually deliver or that they may not document all the counseling they truly provide. The study may also have been affected by nonresponse bias—those who did not respond to the survey may have been reluctant to be assessed about an area in which they had little knowledge. However, the relatively high response rates should have minimized this type of bias.
A possible additional limitation relates to the study population. Only psychiatrists and internists at an academic center were surveyed, raising questions about generalizability. The need to perform initial assessment of providers in an academic setting is underscored by the fact that residents, medical students, physicians' assistants, and nurse practitioners are educated primarily in academic facilities. If faculty in these settings are not interested in and willing to provide clinical preventive medical services, educational efforts in this area will likely fail.
The survey results suggest areas for potential change in professional education. Further assessment of actual delivery of preventive medical services to psychiatric inpatients and outpatients in a variety of care settings is needed and is currently under way.
Dr. Carney is affiliated with the departments of psychiatry, internal medicine, and preventive medicine and environmental health, Dr. Goerdt is with the department of internal medicine, and Dr. Doebbeling is with the departments of internal medicine and preventive medicine at the University of Iowa College of Medicine in Iowa City. Dr. Yates is with the department of psychiatry at the University of Oklahoma in Tulsa. Dr. Doebbeling is also affiliated with the Iowa City Veterans Affairs Medical Center. Address correspondence to Dr. Carney, Department of Psychiatry, 202 Medical Education Building, University of Iowa College of Medicine, Iowa City, Iowa 52242 (e-mail, [email protected]). An earlier version of this paper was presented at the annual meeting of the Academy of Psychosomatic Medicine held November 14-17, 1996, in San Antonio, Texas.
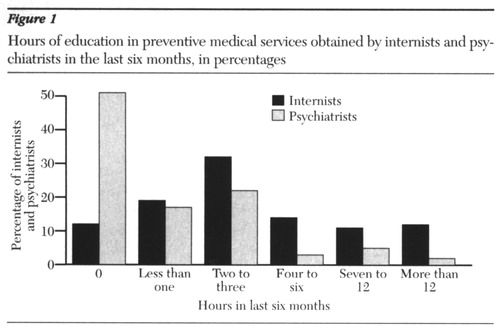
Figure 1. Hours of education in preventive medical services obtained by internists and psychiatrists in the last six months, in percentages
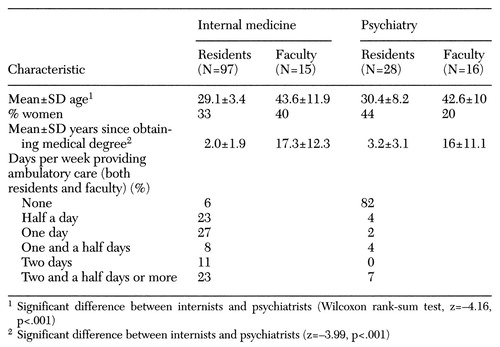 |
Table 1. Selected characteristics of internal medicine and psychiatric residents and faculty who participated in a survey of knowledge, attitudes, and beliefs about clinical preventive medical services
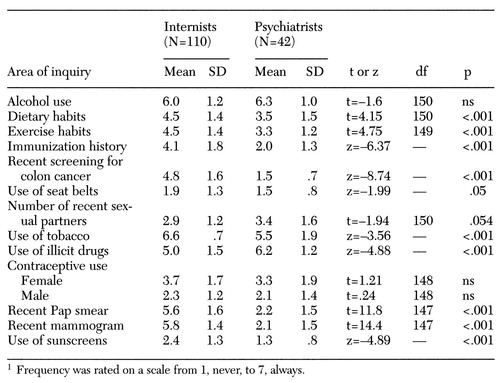 |
Table 2. Mean frequency of internists' and psychiatrists' asking new patients about their history in areas addressed in clinical preventive medical services1
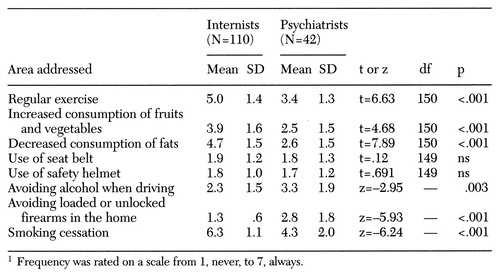 |
Table 3. Mean frequency of internists' and psychiatrists' counseling patients in areas of preventive health1
1. Silberman EK, Lu F, O'Neill P, et al: Developing a primary care role for psychiatrists. Bulletin of the Association for Academic Psychiatry 22:4A, 1994Google Scholar
2. Wulsin LR: An agenda for primary care psychiatry. Psychosomatics 37:93-99, 1996Crossref, Medline, Google Scholar
3. Shore JH: Psychiatry at a crossroad: our role in primary care. American Journal of Psychiatry 153:1398-1403, 1996Link, Google Scholar
4. Kaplan HI, Sadock BJ, Grebb JA: Community (public) psychiatry, in Synopsis of Psychiatry, 7th ed. Edited by Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1994Google Scholar
5. Tsuang MT, Woolson RF: Mortality in patients with schizophrenia, mania, depression, and surgical conditions: a comparison with general population mortality. British Journal of Psychiatry 130:162-166, 1977Crossref, Medline, Google Scholar
6. Tsuang MT, Woolson RF: Excess mortality in schizophrenia and affective disorders: do suicides and deaths solely account for this excess? Archives of General Psychiatry 35:1181-1185, 1978Google Scholar
7. Martin RL, Cloninger CR, Guze SB, et al: Mortality in a follow-up of 500 psychiatric outpatients: I. total mortality. Archives of General Psychiatry 42:47-54, 1985Crossref, Medline, Google Scholar
8. Black DW, Warrack G, Winokur G: The Iowa record-linkage study: I. suicides and accidental deaths among psychiatric patients. Archives of General Psychiatry 42:71-75, 1985Crossref, Medline, Google Scholar
9. US Preventive Services Task Force: Guide to Clinical Preventive Services, 2nd ed. Baltimore, Williams & Wilkins, 1996Google Scholar
10. Clinician's Handbook of Preventive Services: Put Prevention Into Practice. Washington, DC, US Public Health Service, Office of Disease Prevention and Health Promotion, 1994Google Scholar
11. Ely JW, Goerdt CH, Bergus GR, et al: The effect of physician characteristics on compliance with adult preventive care guidelines. Family Medicine 30:34-9, 1998Medline, Google Scholar
12. Goerdt CJ, Ely JW, Bergus GR, et al: Knowledge of preventive care guidelines by residents and faculty. Journal of General Internal Medicine 11(4)(suppl 1):124, 1996Google Scholar
13. Statistical Package for the Social Sciences for Windows, Version 7.0. Chicago, SPSS, 1995Google Scholar
14. Nichol KL, Margolis KL, Wuorenma J, et al: The efficacy and cost-effectiveness of vaccination against influenza among elderly persons living in the community. New England Journal of Medicine 331:778-784, 1994Crossref, Medline, Google Scholar
15. Frame PS, Carlson SJ: A critical review of periodic health screening using specific screening criteria. Journal of Family Practice 2:29-36, 1975Medline, Google Scholar
16. Lewis CE: Disease prevention and health promotion practices of primary care physicians in the United States. American Journal of Preventive Medicine 4(suppl):9-16, 1988Google Scholar
17. Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Pub PHS 534. Washington, DC, US Public Health Service, 1993Google Scholar
18. Montano DE, Phillips WR: Cancer screening by primary care physicians: a comparison of rates obtained from physician self-report, patient survey, and chart audit. American Journal of Public Health 85:795-800, 1995Crossref, Medline, Google Scholar
19. Lurie N, Manning WG, Peterson C, et al: Preventive care: do we practice what we preach? American Journal of Public Health 77:801-804, 1987Google Scholar
20. Lemley KB, O'Grady ET, Rauckhorst L, et al: Baseline data on the delivery of clinical preventive services provided by nurse practitioners. Nurse Practitioner 19:57-63, 1994Crossref, Medline, Google Scholar
21. Bindman AB, Grumbach K, Osmond D, et al: Primary care and receipt of preventive services. Journal of General Internal Medicine 11:269-276, 1996Crossref, Medline, Google Scholar
22. Meissner HI, Potosky AL, Convissor R: How sources of health information relate to knowledge and use of cancer screening exams. Journal of Community Health 17:153-165, 1992Crossref, Medline, Google Scholar
23. Fox SA, Murata PJ, Stein JA: The impact of physician compliance on screening mammography for older women. Archives of Internal Medicine 151:50-56, 1991Crossref, Medline, Google Scholar
24. McPhee SJ, Bird JA: Implementation of cancer prevention guidelines in clinical practice. Journal of General Internal Medicine 5(suppl 5):116-122, 1990Google Scholar
25. McPhee SJ, Richard RJ, Solkowitz SN: Performance of cancer screening in a university general internal medicine practice. Journal of General Internal Medicine 1:275-281, 1986Crossref, Medline, Google Scholar
26. Glassman AH: Cigarette smoking: implications for psychiatric illness. American Journal of Psychiatry 150:546-553, 1993Link, Google Scholar
27. Covey LS, Glassman AH, Stetner F: Major depression following smoking cessation. American Journal of Psychiatry 154:263-265, 1997Link, Google Scholar
28. Hymowitz N, Jaffe FE, Gupta A, et al: Cigarette smoking among patients with mental retardation and mental illness. Psychiatric Services 48:100-102, 1997Link, Google Scholar
29. Addington J, el-Guebaly N, Addington D, et al: Readiness to stop smoking in schizophrenia. Canadian Journal of Psychiatry 42:49-52, 1997Crossref, Medline, Google Scholar
30. Linn LS, Yager J, Leake BD, et al: Differences in the numbers and costs of tests ordered by internists, family physicians, and psychiatrists. Inquiry 21:266-275, 1984Medline, Google Scholar
31. Cheney C, Ramsdell JW: Effect of medical records' checklists on implementation of periodic health measures. American Journal of Medicine 83:129-136, 1987Crossref, Medline, Google Scholar
32. Barnett GO, Winickoff RN: Quality assurance and computer-based patient records. American Journal of Public Health 80:527-528, 1980Crossref, Google Scholar
33. McDonald CJ, Hui SL, Smith DM, et al: Reminders to physicians from an introspective computer medical record: a two-year randomized trial. Annals of Internal Medicine 100:130-138, 1984Crossref, Medline, Google Scholar
34. Litzelman DK, Dittus RS, Miller ME, et al: Requiring physicians to respond to computerized reminders improves their compliance with preventive care protocols. Journal of General Internal Medicine 8:311-317, 1993Crossref, Medline, Google Scholar



