Use of General Medical Services Among Medicaid Patients With Severe and Persistent Mental Illness
Abstract
OBJECTIVE: The aim of this study was to examine patterns of use of general medical services among persons with a severe and persistent mental illness enrolled in Medicaid from 1996 to 1998. METHODS: A total of 669 persons with a severe and persistent mental illness were identified by using statewide clinical criteria. A three-year database of Medicaid claims was developed to examine service use. The main outcome measures were use of outpatient services for a general medical problem, use of dental and vision services, and use of screening tests for women. Service use was examined by primary psychiatric diagnosis (schizophrenic, affective, paranoid, and anxiety disorders), and analyses controlled for the presence of a chronic medical condition, age, race, and sex. RESULTS: This study found high levels of service use for outpatient services but very low levels for primary and preventive services. Although 78 percent of persons with a schizophrenic disorder had an office-based visit during the three-year period, all persons with an anxiety disorder had such a visit. Sixty-nine percent of persons with a schizophrenic disorder had at least one emergency department visit, whereas 83 percent of those with an anxiety disorder had such a visit. Dental and vision visits and the use of mammograms and pap tests followed the same pattern; persons with a schizophrenic disorder had fewer visits and had less overall use than the other diagnostic groups. The use patterns across the four groups were significantly different in outpatient service use, dental and vision service use, and screening tests for women. Compared with persons with a schizophrenic disorder, those with an anxiety disorder were more likely to have had an office-based visit and to have received vision services, those with a paranoid disorder were more likely to have used dental services or received a mammogram, and those with an affective disorder were more likely to have had a pap test. CONCLUSION: Although this group of Medicaid patients with severe and persistent mental illness had access to providers, they received an unacceptably low level of preventive care. Use of health services for general medical problems differed somewhat by primary psychiatric illness.
A substantial body of literature has documented consistently higher morbidity and mortality rates for individuals with severe and persistent mental illness (1). These high morbidity and mortality rates have prompted interest in patterns of use of general medical services as a possible contributing factor to these poor outcomes (2).
The current literature presents a mix of findings on health service use, noting that compared with the general population, persons with serious and persistent mental illness tend to receive services such as immunizations and colorectal cancer screenings at equivalent rates, receive pap tests and mammography less frequently, and receive services from the emergency department more frequently (3,4,5,6). In a study of persons with psychotic disorders, high levels of health service use were found in emergency departments and physicians' offices (7). Dickerson and colleagues (8) found that persons with affective or schizophrenic disorders were more likely to receive medical care services than the general population. Nevertheless, most of these studies have examined service use patterns of persons with serious mental illness as a group, comparing those with a serious mental illness with those without such a condition. A recent study of patients in the Department of Veterans Affairs system examined service use patterns among persons with serious mental illness and found differences by psychiatric condition (9).
Understanding these service use patterns among persons with a serious mental illness provides a foundation on which to build systems designed to meet the needs of this population. However, understanding these patterns is difficult because medical services address a broad range of preventive, acute, and chronic health problems and the recommended frequency varies by the type of service.
There is little reason to believe that these patterns of service use are or should be the same across all psychiatric diagnoses. Diagnostic variability among persons with serious mental illness is wide, and symptoms are diverse. Many of these symptoms interfere with the person's ability to seek health care. For example, impairment differences may influence an individual's willingness to seek out and use care—psychotic patients may be too impaired or suspicious to seek help, and anxious patients may seek out care inappropriately. Different treatments are associated with different diagnoses, and the side effects of medications place people at higher risk of other medical conditions. Newer antipsychotic medications may cause diabetes and may lead to a specific need for medical care.
In this study we examined use of general medical services among persons with a serious mental illness. We examined four diagnostic subgroups: schizophrenic, affective, paranoid, and anxiety disorders. Three types of services were studied: outpatient visits for the treatment of a general medical problem, dental and vision visits, and preventive health screenings for women. We asked two primary research questions: How does use of general medical services among persons with severe and persistent mental illness compare with use reported for the population in Ohio who received Medicaid and screening rates in the general population? How does service use differ among the different groups of persons with mental illness when the analyses controlled for age, sex, race, and chronic medical problem?
Methods
Sample
The institutional review board of Ohio State University approved the study. Persons with a severe mental illness were identified for this study with the assistance of the Franklin County mental health agency. These persons were already classified during their course of treatment as having a severe illness on the basis of clinical criteria developed by the Ohio Department of Mental Health. These criteria incorporated severity by using three measures: the severity of the axis I diagnoses, the duration of symptoms requiring mental health services, and the level of functioning.
Persons who were identified as having severe mental illness were included in our study if they lived in Ohio and were community dwelling, African American or white, aged 18 years or older, and enrolled in Medicaid during all three years of the study (1996 through 1998). Because persons with Medicaid could also be enrolled in Medicare or, because they lived in Ohio, be required to spend down part of their monthly assets to be eligible for Medicaid, this analysis was limited to persons whose only insurance was Medicaid. This factor removed some of the possible unknowns in service use that may have directly influenced the outcomes.
Psychiatric diagnostic category
Mental health diagnoses were obtained from the county mental health agency database. These diagnoses were obtained during the patients' course of treatment and were used by the county to document the primary reason for the patient's mental health disability. Diagnoses were listed by using the International Classification of Diseases, 9th Revision (ICD-9-CM). Specific diagnoses were grouped by major category to aid in analysis. In preliminary analyses 29 diagnostic groups were identified. Because of concern about small samples, the analysis was restricted to categories with more than 60 participants. Four diagnostic categories fit this requirement: schizophrenic disorders (ICD-9-CM code 295), affective disorders (ICD-9-CM code 296), paranoid disorders (ICD-9-CM code 297), and anxiety disorders (ICD-9-CM code 300).
Data sources
The data came from two sources. The 1996 county mental health administrative database was used to identify persons with a serious mental illness, the primary mental health diagnosis, and the Medicaid number of the recipient. The second database was from the Medicaid agency and included demographic data and claims data for 1996, 1997, and 1998. These two databases were merged by using the Medicaid number of the recipient, the only reliable variable common to both files.
Dependent variables
The primary dependent measures were service use measures examined within three categories. The first category was general medical services encounter by location. General medical diagnoses were identified by using the first three digits of the ICD-9-CM code that was listed as the principal diagnosis on the claim. General medical diagnoses included all categories except for those described as mental disorders. The second category was dental and vision visits, identified by using an indicator on the claim form that reported the type of provider. The third category was preventive services among women—pap tests (all women) and mammograms (women aged 40 years and older)—identified with CPT codes.
Independent variables
The independent measures were demographic characteristics and primary psychiatric diagnoses. Analyses were completed to identify chronic health conditions in year 1. Two health conditions were chosen as chronic health conditions: hypertension because of the general prevalence in the population and diabetes because of the increased risk in this group. In addition, these two conditions could influence the use of general medical services.
Analysis
Statistics were completed with SAS version 8.2. Differences in demographic variables (sex, age, and race) and two chronic health problems (hypertension and diabetes) by psychiatric group were tested with Pearson's chi square analysis. Adjusted logistic regression models were estimated to test whether the service use patterns (use compared with no use) differed across psychiatric grouping. To do this analysis, a referent group was needed as a basis for comparison. We chose the group with schizophrenic disorders as the referent group because from clinical work we suspected that this group would likely be the most impaired. Any of the four groups could have been chosen. The models for outpatient, vision, dental, and women's health screening visits were estimated by using all three years of data. Logistic regression models for visits to the emergency department and physicians' offices were estimated by using data from only years 2 and 3, because hypertension and diabetes were determined during year 1. This method controlled for the possibility that individuals were given diagnoses at different time points during the 12-month period, which resulted in appropriate differential use of services. Our methods ensured a single diagnosis for the entire study period. A significance level of .05 was used (10).
Results
Table 1 shows the demographic characteristics and chronic condition data by diagnostic group. A majority of the individuals were white and female, although there were race and sex differences in the diagnostic categories. African Americans and men were given a diagnosis of a schizophrenic disorder more often than their respective comparison group. Most of the participants were aged between 35 and 54 years. Approximately 16 percent of the individuals were aged 55 years and older. Prevalence of hypertension ranged from 25 percent among persons with a paranoid disorder to only 9 percent among those with a schizophrenic disorder. Prevalence of diabetes ranged from 13 percent among persons with a schizophrenic disorder to 24 percent among those with a paranoid disorder. Statistically significant differences were found in the sex, race, and hypertension categories.
Overall, use of general medical services was high for all diagnostic categories, as shown in Table 2. The range across diagnoses is notable for its breadth. Although 78 percent of persons with a schizophrenic disorder had an office-based visit during the three-year period, all persons with an anxiety disorder had such a visit. A similar pattern was seen for emergency department visits. Again, the range across diagnoses is significant. Sixty-nine percent of persons with a schizophrenic disorder had at least one emergency department visit, whereas 83 percent of those with an anxiety disorder had such a visit. Dental and vision visits and the use of mammograms and pap tests followed the same pattern; persons with a schizophrenic disorder had fewer visits and had less overall use than the other diagnostic groups. The use patterns across the four groups were significantly different in outpatient service use, dental and vision service use, and screening tests for women.
Table 3 details the results of the logistic analyses. These odds ratios are relative to those with a schizophrenic disorder. In the fully adjusted models, no significant differences were found for emergency department use, but differences were found in the other five service use categories. Compared with persons with a schizophrenic disorder, those with an anxiety disorder were more likely to have had an office-based visit and to have received vision services, those with a paranoid disorder were more likely to have used dental services or received a mammogram, and those with an affective disorder were more likely to have had a pap test.
Discussion
This study contributes to a growing but still limited body of research that examines the patterns of use of general medical services among persons with severe mental illness and indicates that there may be some differences by psychiatric diagnosis. From these data appropriate service use cannot be determined; yet gaining this knowledge must be the goal. Our results suggest that, to achieve this end, programs that assist individuals with severe mental illness may need to provide very different assistance on the basis of the psychiatric condition. For example, persons with anxiety disorders may need a special liaison to general medical services to protect against overuse of health services, and programs serving those with schizophrenia may need to be more assertive in getting their clients to a general medical doctor.
Furthermore, these results demonstrate overall use of the emergency department to be remarkably high, considerably higher than that of the general Medicaid population in Ohio. Between 1997 and 1998 a survey found that 20 percent of Ohio residents and 21 percent of Ohio residents who received Medicaid reported using the emergency department at least once (11). A similar finding of greater service use among persons with a severe mental illness was documented in Arizona in a study that compared the medical claims of the serious mentally ill population with a general Medicaid population (2).
The use patterns for office visits indicate that this population with severe mental illness has access to health care services and uses services at a much greater rate than the general population of Ohio (11,12). However, despite this high use rate, the rates for preventive care, as evidenced by women's health preventive care, were dismal. When we compared our study's rates of women's health preventive care to those in a national survey, our results were alarming. A review of cancer screening practices from the National Health Interview Survey indicates that the biennial mammography rate was 67 percent, and approximately 80 percent of the general population of women had a pap test in 1998 (13). Several studies of mammography and pap screening among persons with serious mental illness have found substantially higher rates of receiving these tests than those found in our study (14,15). However, those studies were based on self-reports, not on administrative data.
Our study also found low rates of service use for dental and vision services. Little information has been documented on the receipt of dental services in the national population of persons with severe mental illness. Dickerson and colleagues (14) reported a higher rate of dental service use (58 percent) in a group of women with schizophrenia than the rate that we found in our study, but other reports indicate that dental use is lower in our study group than in the public (8). Our findings point to a wide gap in the provision of primary and secondary preventive care for persons with mental illness. This finding is clinically important. Even though this group of persons with mental illness saw a doctor more frequently than the general population, they received an unacceptable level of preventive services.
This study has several possible limitations. Studies based on administrative claims rely on data collected for another purpose. Reliability and specificity of coding in administrative claims research can be inconsistent. Services paid for by another source (including families) are also not included. Considerations of patient preferences in care, provider preferences or bias, type of delivery system that the patient had access to, or clinical appropriateness of care were not evaluated. Each of these can be a source of bias in determining service use.
Conclusions
This analysis showed that persons who have severe mental illness use general medical services at high rates. When these rates were compared with those of the general population, our findings suggested an overuse of emergency department visits and an underuse of screening tests. Differences by mental health diagnosis were found, which indicated that differential approaches may need to be developed that are tailored to the patients' symptoms to ensure appropriate use of general medical services.
Acknowledgment
This study was supported by grant 99-1128 from the office of program evaluation and research at the Ohio Department of Mental Health.
Dr. Salsberry and Dr. Kennedy are affiliated with the College of Nursing at Ohio State University, 1585 Neil Avenue, Columbus, Ohio 43210 (e-mail, [email protected]). Dr. Chipps is with the Ohio State Medical Center in Columbus.
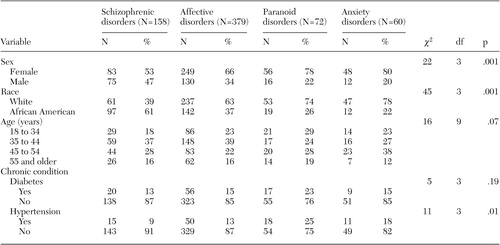 |
Table 1. Demographic characteristics of 669 persons with severe and persistent mental illness who were enrolled in Medicaid in Ohio from 1996 to 1998, by diagnostic group
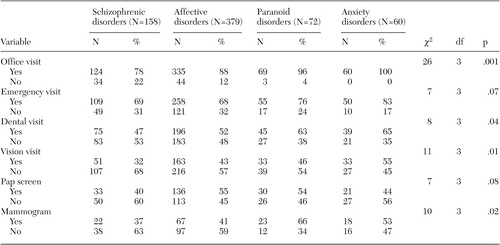 |
Table 2. Use of general medical services by diagnostic category among 669 persons with severe and persistent mental illness who were enrolled in Medicaid in Ohio from 1996 to 1998, by diagnostic group
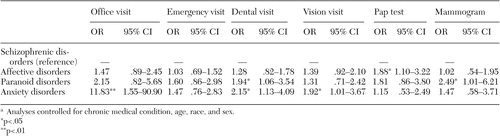 |
Table 3. Multivariate logistic regression results indicating associations between service use and psychiatric disorder among 669 persons with severe and persistent mental illness who were enrolled in Medicaid in Ohio from 1996 to 1998a
a Analyses controlled for chronic medical condition, age, race, and sex.
1. Felker B, Yazel JJ, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356–1363, 1999Google Scholar
2. Berren MR, Santiago JM, Zent MR, et al: Health care utilization by persons with severe and persistent mental illness. Psychiatric Services 50:559–561, 1999Link, Google Scholar
3. Carney CP, Allen J, Doebbeling BN: Receipt of clinical preventive medical services among psychiatric patients. Psychiatric Services 53:1028–1030, 2002Link, Google Scholar
4. Steiner JL, Hoff RA, Moffett C, et al: Preventive health care for mentally ill women. Psychiatric Services 49:696–698, 1998Link, Google Scholar
5. Druss BG: Cardiovascular procedures in patients with mental disorders. JAMA 283:198–199, 2000Crossref, Medline, Google Scholar
6. Petersen LA, Normand SL, Druss BG, et al: Process of care and outcome after acute myocardial infarction for patients with mental illness in the VA health system: are there disparities? Health Services Research 38:41–63, 2003Google Scholar
7. Carr VJ, Johnston PJ, Lewin TJ, et al: Patterns of service use among persons with schizophrenia and other psychotic disorders. Psychiatric Services 54:226–235, 2003Link, Google Scholar
8. Dickerson FB, McNary SW, Brown CH, et al: Somatic healthcare utilization among adults with serious mental illness who are receiving community psychiatric services. Medical Care 41:560–570, 2003Medline, Google Scholar
9. Cradock-O'Leary J, Young AS, Yano EM, et al: Use of general medical services by VA patients with psychiatric disorders. Psychiatric Services 53:874–878, 2002Link, Google Scholar
10. Hair JF, Tatham RL, Anderson RE, et al: Multivariate Data Analysis, 5th ed. Upper Saddle River, NJ, Prentice Hall, 1998Google Scholar
11. Access to Health Care for Ohio Adults, 1998. Columbus, Ohio, Ohio Department of Health, 2002Google Scholar
12. Mascarenhas A, Pathak D, Salsberry P: Association between poor health care access and population characteristics. Columbus, Ohio, Center for Health Outcomes, Policy, and Evaluation Studies, 2001Google Scholar
13. Hiatt K, Klabunde C, Breen N, et al: Cancer screening practices from the National Health Interview Surveys: past, present, and future. Journal of the National Cancer Institute 94:1837–1846, 2002Crossref, Medline, Google Scholar
14. Dickerson FB, Pater A, Origoni AE: Health behaviors and health status of older women with schizophrenia. Psychiatric Services 53:882–884, 2002Link, Google Scholar
15. Folsom DP, McCahill M, Bartels SJ, et al: Medical comorbidity and receipt of medical care by older homeless people with schizophrenia or depression. Psychiatric Services 53:1456–1460, 2002Link, Google Scholar



