Comparison of Psychiatrists' and Other Physicians' Assessments of Their Ability to Deliver High-Quality Care
Abstract
OBJECTIVE: This study compared psychiatrists' assessments of their ability to deliver high-quality care with those of other physicians. METHODS: Data were used from the Community Tracking Study Physician Survey, a national survey of 12,528 physicians. Linear regression models were used to investigate the effects of type of physician (psychiatrist or other physician), managed care involvement, and ability to obtain inpatient care on four measures of physicians' assessments of quality. RESULTS: In models that did not control for difficulty in obtaining inpatient services, assessments of quality were significantly lower among psychiatrists than among other physicians. Furthermore, although managed care involvement was associated with lower assessments of quality for all physicians in these models, the effects were stronger for psychiatrists than for other physicians. However, after difficulty in obtaining inpatient services was controlled for, psychiatrists' and other physicians' assessments of quality were similar. CONCLUSIONS: Compared with other physicians, psychiatrists' assessments of the quality of care that they provide were lower and their assessments were more influenced by involvement with managed care. These differences may be mediated by difficulty in obtaining inpatient services. When designing and administering behavioral health benefits packages, clinical policy makers should consider the possible effects of reduction in inpatient services on quality of care.
Health care in the United States has rapidly evolved from a predominantly fee-for-service system to one in which most care is provided under managed care arrangements. This change has been credited with substantial cost savings, particularly in mental health care. The rate of growth in behavioral health care costs has been lower than that for health care, and the fraction of the health care budget devoted to behavioral health has decreased (1,2,3). Also, hospital stays have decreased more for behavioral disorders than for nonbehavioral disorders (4).
Financing for behavioral health care differs from other health care services in two important ways. First, despite federal and state parity laws (5), copayments and coinsurance rates are frequently higher for behavioral health care than for other medical conditions, and limits on behavioral health inpatient days or outpatient visits are often more stringent (6,7,8,9). Second, mental health services are often coordinated through a separate managed behavioral health organization (MBHO) in a carve-out arrangement in which the financing and administration of behavioral health care services is separated from other health care services (10,11,12,13).
These differences in financing and insurance coverage emerged during a period when behavioral health care costs were growing more rapidly than overall health care costs and likely were a response to this rapid growth. During this time, use patterns often corresponded to what some felt were overly generous insurance benefits. For example, many lengths of stay were exactly 30 days (the maximum number of days allowed by insurers), leading critics to charge that the subjective nature of psychiatric diagnoses and treatment outcomes, coupled with a lack of cost consciousness, led to arbitrarily long inpatient stays or an excessive number of outpatient visits. Ironically, the subjective aspects of mental disorders may now contribute to mental health service constraints, given inherent limitations in the precision of treatment outcome measures.
The impact of changes in the health care system on the use of and access to behavioral health services as well as quality of care is an active area of inquiry (2,10,12,13,14,15,16,17,18,19,20,21). Recent studies of the use of mental health services show fewer inpatient admissions and shorter lengths of stay (10,12,18,21). The number of individuals who use outpatient behavioral health services has increased (2,15), but the cost per episode has decreased (12,18). The evidence is mixed on whether quality of care is better, equivalent, or worse under managed mental health care compared with other methods of financing and delivery (15,16,17,22,23,24,25,26).
A complementary strategy to investigate quality of behavioral health care is to analyze physicians' assessments of their ability to deliver high-quality care (19,20,27,28). This strategy may give us important insights in this area in which there is mixed evidence. By using data from the first wave of the Community Tracking Study Physician Survey (CTS) (29), Reschovsky and colleagues (27) analyzed physicians' responses to questions about their ability to deliver high-quality care. They found that half of all physicians disagreed with at least one of four statements that reflected aspects of quality of care. Psychiatrists were less likely than other specialists to say that they were able to deliver high-quality care. The study found a significant, albeit modest, association between involvement with managed care and disagreement with statements about quality. Sturm and Ringel (28) used data from the second wave of the CTS and also found that psychiatrists were less likely than other specialists or primary care physicians to endorse statements about quality.
In this study we used data from the 1996 through 1997 CTS to compare psychiatrists' self-reported ability to deliver high-quality care with that of other physicians. We built on the work of Reschovsky and colleagues and Sturm and Ringel in two important ways. First, we investigated whether the strength of the relationship between physicians' involvement in managed care and their assessments of quality differed for psychiatrists and other physicians. We hypothesized that the relationship between involvement with managed care and physician-reported quality problems would be stronger for psychiatrists than for other physicians. Second, we investigated one possible reason that psychiatrists' assessments of their ability to deliver high-quality care are lower than those of other physicians, namely that such differences are mediated by physician-reported ability to obtain inpatient care for patients.
Methods
Sample
The data came from the first round of the CTS, a nationally representative cross-sectional telephone survey fielded from 1996 to 1997 (29,30,31). The purpose of the CTS is to "document changes in health care systems over time and track the effects of those changes on people" (32). Physicians who provide direct patient care at least 20 hours per week were eligible for the study. Federal employees, non-direct care specialists (for example, pathologists), residents, interns, and foreign medical graduates licensed only temporarily to practice in the United States were not included. The sampling frame was clustered within 60 randomly selected U.S. communities and was constructed from the master files of the American Medical Association and the American Osteopathic Association. A supplemental national sample was included to increase the precision of national estimates. Interviews were completed for 12,528 physicians (623 psychiatrists and 11,905 other physicians), with a response rate of 65 percent. We used the 1996 through 1997 wave of the CTS rather than the 1998 through 1999 version because it was the only version available that allowed us to adjust for geographic clustering. Sample weights were used to account for sample design and nonresponse. Physicians gave verbal consent to participate in the survey. This study was approved by the institutional review board of the University of California, Los Angeles.
Variables
Dependent variables. Physicians were asked four questions to rate their strength of agreement on a 5-point scale (5, agree strongly; 4, agree somewhat; 3, neither agree nor disagree; 2, disagree somewhat; and 1, disagree strongly) about their ability to provide high-quality care: it is possible to provide high-quality care to all my patients; I have adequate time to spend with my patients during typical office or patient visits; I have the freedom to make clinical decisions that meet my patients' needs; and it is possible to maintain the kind of continuing relationships with patients over time that promote the delivery of high-quality care. Although past studies often dichotomized these variables (27,28), we chose to analyze the original scores, both to enhance power by reflecting the magnitude of potential differences and because we were concerned that the results might be sensitive to differences in cutoff points.
Independent variables. Similar to previous studies that used CTS data (27,33), our study used a set of variables that represented physician characteristics and the practice environment. Our primary measure of managed care involvement was the percentage of revenue from managed care. We dichotomized physicians into two groups: those who received 25 percent or less of their revenue from managed care and those who received more than 25 percent of their revenue from managed care. Approximately half of all psychiatrists in the CTS reported that they received 25 percent or less of their revenue from managed care sources. In sensitivity analyses our results did not differ substantively in models that used a dichotomized measure of managed care revenue and models that used a continuous measure. We modeled the number of managed care contracts (zero, one to five, six or more) with a set of indicator variables. We also dichotomized physicians into psychiatrists or other physicians.
Physicians were asked about their ability to obtain medically necessary services for their patients—specifically, how often they were able to admit patients for nonemergent hospitalization and how often they were able to obtain an adequate number of inpatient days for hospitalized patients. Answers were on a 6-point scale (6, always; 5, almost always; 4, frequently; 3, sometimes; 2, rarely; and 1, never).
The CTS did not directly measure characteristics of the physician's patients. We followed the model used by Landon and colleagues (33) and used the percentage of patient revenue from Medicaid and Medicare as proxies for the proportion of low-income and elderly patients, respectively. Physicians were again classified into groups on the basis of sources of the physician's revenue: greater than or less than or equal to 10 percent of total revenue from Medicaid and greater than or less than or equal to 15 percent of total revenue from Medicare. These cut points divided physicians into roughly equal groups.
In the CTS, practices were grouped into six categories: solo or two-physician practice, group practice (three or more physicians), group or staff-model health maintenance organization (HMO), medical school, hospital based, or other. In our regression analyses, we combined the categories of HMO and other because of the small number of HMO psychiatrists (N=19). A physician could be a full owner, part owner, or employee of the practice.
Our models included whether the physician was salaried and whether compensation was affected by measures of quality of care, practice profiling, patient satisfaction, and physician productivity. In the CTS, owners of solo or two-physician practices were not asked about compensation; we assumed that they were not salaried and that their compensation depended on their own productivity.
Physicians used a 6-point scale to rate the effect of formal practice guidelines, practice profiling, and satisfaction surveys on their practice of medicine, which we termed "care management factors." For each variable we classified physicians into two groups: those who reported a very large, large, or moderate effect and those who reported a small, very small, or no effect. We controlled for gender and year of graduation (before 1971, 1971 through 1985, or after 1985).
Analyses
We first calculated descriptive statistics of the type of practice; ownership; proportion of revenue from managed care, Medicare, and Medicaid; and physician-reported quality by physician type.
We then used multiple linear regression to investigate the effects of managed care involvement and physician type on physicians' assessments of quality. (Our results were essentially the same in logistic regression models.) We allowed the effect of percentage of revenue from managed care to differ for psychiatrists and other physicians through use of an appropriate interaction term. To do this we constructed an interaction term that was 1 for psychiatrists who received more than 25 percent of their revenue from managed care and 0 in other cases. A negative coefficient means that the effect of the percentage of revenue received from managed care had a greater negative effect on psychiatrists' assessments of quality than other physicians' assessments of quality. In a model such as this, with an interaction between type of physician and revenue from managed care, statistical tests or differences in quality assessments between psychiatrists and other physicians is done for both levels of managed care revenue (that is, 0 to 25 percent and 26 to 100 percent). In other words, on the basis of the estimated regression models, we conducted two-sided t tests that compared psychiatrists with other physicians at each level of revenue from managed care. We reported the results from these t tests in the text, but not in the Tables. These models controlled for all independent variables described above, except for difficulty in obtaining inpatient services.
Finally, we investigated whether the relationship between type of physician and physicians' assessments of quality might be mediated by difficulty in obtaining necessary services. To do this assessment we investigated the effects of managed care involvement and physician type on physicians' assessments of quality by using linear regressions that also controlled for difficulty in obtaining inpatient services. To the extent that this added predictor explained the same variation in outcomes as type of physician, we interpreted difficulty in obtaining inpatient services as a possible mediator.
Statistical tests were two-tailed. Analyses were weighted and calculated with SUDAAN Software for the Statistical Analysis of Correlated Data to take into account the complex survey design. The rates of item-level missing data were less than 3 percent for all dependent variables discussed here. The rates of item-level missing data for two predictors—nonemergency hospital admission and adequate number of inpatient days—were 13 percent and 12 percent, respectively, resulting in 18 percent of missing data for the complete-case regression analyses. Actual Ns used in analyses are indicated in the tables.
Results
As shown in Table 1, compared with other physicians, psychiatrists were significantly more likely to be in solo or two-physician practices and significantly less likely to be in group practices. On average, psychiatrists received a significantly smaller percentage of their revenue from managed care than other physicians (35 percent compared with 40 percent, p<.001). Psychiatrists also received a smaller percentage of their revenue from Medicare than other physicians (21 percent compared with 32 percent, p<.001) but a greater percentage from Medicaid (17 percent compared with 14 percent, p=.01).
The mean±SD scores for the four outcomes—ability to provide high-quality care to all patients, adequate time to spend with patients, freedom to make clinical decisions, and ability to maintain continuing relationships with patients over time—were, respectively, 3.9±1.3, 3.7±1.4, 4±1.3, and 3.6±1.5. As shown in Tables 2 and 3, psychiatrists' assessments of their ability to deliver high-quality care were generally lower than those of other physicians, and they also reported more difficulty obtaining nonemergency inpatient hospitalizations and an adequate number of inpatient days.
As shown in Table 4, in multiple regression models psychiatrists' ratings of quality were lower than those of other physicians in both revenue groups (0 to 25 percent and 26 to 100 percent) across all four measures of quality, and these differences were highly significant. Physicians who received a greater percentage of revenue from managed care or who had more managed care contracts reported significantly lower levels of quality. The interaction term of psychiatrist with managed care revenue was negative and significant in two regressions (p<.05) and negative in the other two, although these results were not significant. A negative interaction coefficient means that the percentage of revenue from managed care was associated with a larger negative effect on psychiatrists' quality ratings than on other physicians' quality ratings. Furthermore, the magnitude of the interaction was large (-.25 to -.28) when compared with the main effect of percentage of revenue from managed care (-.02 to -.18).
On the other hand, as shown in Table 5, in models that controlled for reports of ability to obtain nonemergent hospitalization and adequate length of stay, no significant difference was found between psychiatrists and other physicians in three of the four regressions. The only significant difference between psychiatrists and other physicians was with the dependent variable high-quality care in the group who received more than 25 percent of revenue from managed care (t=2.82, p<.01). The interaction term of psychiatrist with managed care revenue was negative in all regressions, although these results were not statistically significant. The effects of percentage of revenue from managed care remained comparable to those shown in Table 4, in which effects were significant in three regressions.
Discussion
In our initial series of multiple regressions, the mean scores of psychiatrists' assessments of the quality of care that they provide were lower than those of other physicians. The size of the effect was moderate, approximately one-half of a point, or two-fifths of a standard deviation, and highly significant. Furthermore, although an increased percentage of revenue from managed care was associated with lower assessments of quality, this effect was stronger for psychiatrists, by approximately one-quarter of a point. These findings, coupled with the fact that psychiatrists actually received less of their income from managed care, might mean that psychiatrists have a greater propensity to be dissatisfied with the health care system in general and with managed care in particular.
However, our second series of regressions suggests an alternative explanation. We found that in models that controlled for ability to obtain nonemergent hospitalizations and adequate length of stay, psychiatrists differed from other physicians in only one of four assessments of quality, and this difference occurred only among psychiatrists and other physicians who received more than 25 percent of their income from managed care. The interactions between psychiatrists and managed care revenue were not significant at the .05 level in any of the four regressions. This finding suggests that psychiatrists' assessments of the quality of care that they provide are lower than those of other physicians because of limited access to psychiatric hospitalizations, a trend that has been well documented for the past 15 years (34,35). It should be noted that a weakening of the association between quality assessments and the independent variables in models that controlled for difficulty in obtaining inpatient services was not a general phenomenon: in these models the percentage of revenue from managed care and the number of managed care contracts remained highly significant negative predictors of physicians' quality assessments.
Psychiatrists received a smaller portion of their income from managed care than other physicians, but previous research suggests that managed care organizations (MCOs) may affect physicians who do not receive any income from managed care (27,36). This effect could occur if MCOs or MBHOs play an important role in establishing community practice patterns. In behavioral health it is likely that MBHO efforts to decrease psychiatric admissions and length of stay have had spillover effects on non-managed care settings, such as Department of Veterans Affairs hospitals and state and county systems. Therefore, MBHOs may have strong effects on the environment in which psychiatrists practice, even if the percentage of revenue that psychiatrists receive from managed care is modest.
One limitation of our study is that the data were from 1996 to 1997. These data were the only publicly available data set that we could obtain that allowed us to adjust for geographic clustering. Although the health care market has continued to evolve, we believe that our results remain relevant. For example, it does not appear that our results reflect a cohort effect, in which younger psychiatrists, trained when shorter stays were the norm, have higher quality ratings than older psychiatrists. In analyses limited to psychiatrists, no significant differences were found in assessments of quality between the three age groups. Also, no evidence exists that access to inpatient services for behavioral care has improved in the past several years (34,35).
Another limitation is that we examined physicians' subjective assessments of quality, not objective measures. Although we do not know of any study that has explicitly investigated the relationship between physicians' assessments and objective quality, our measures have good face validity. Furthermore, physicians' assessments are likely important in their own regard, because the perceived inability to deliver high-quality care likely leads to low morale among psychiatrists.
Conclusions
Our results suggest difficulty in obtaining inpatient services as a possible factor in explaining differences between psychiatrists' and other physicians' assessments of their ability to deliver high-quality care. Limited access to inpatient care was associated with multiple quality measures, suggesting that reductions in inpatient psychiatric services may have more far-reaching effects on quality of care than anticipated. Future research should examine the mechanisms underlying the relationship among access to inpatient care, physicians' assessments of quality, and other measures of quality of care and outcomes. Clinical policy makers should carefully consider possible effects on quality of care when designing and administering behavioral health benefits packages that regulate access to inpatient mental health care.
Acknowledgments
This work was supported by the VISN 16 Mental Illness Research, Education, and Clinical Center of the Department of Veterans Affairs and by grant 044199 from the Robert Wood Johnson Foundation. The authors thank Bruce Landon, M.D., M.B.A., for helpful comments.
Dr. Edlund is affiliated with Department of Veterans Affairs South Central (VISN 16) Mental Illness Research, Education, and Clinical Center in North Little Rock, Arkansas, and the department of psychiatry at the University of Arkansas for Medical Sciences in Little Rock. Dr. Belin is with the department of biostatistics at the University of California, Los Angeles (UCLA) and the department of psychiatry and biobehavioral sciences at UCLA School of Medicine. Dr. Tang and Ms. Liao are with the Health Services Research Center at the UCLA Neuropsychiatric Institute. Dr. Unützer is with the department of psychiatry and behavioral sciences at the University of Washington in Seattle. Send correspondence to Dr. Edlund at Central Arkansas Veterans Health System, Department of Psychiatry, 2200 Fort Roots Drive, Building 58, North Little Rock, Arkansas 72114 (e-mail, [email protected]).
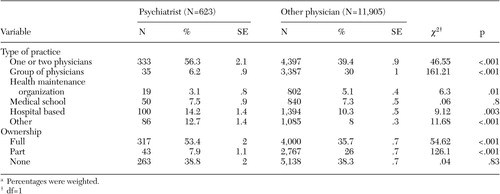 |
Table 1. Ownership, type of practice, and sources of revenue among physicians who participated in the 1996-1997 Community Tracing Study Physician Survey, by type of physiciana
a Percentages were weighted.
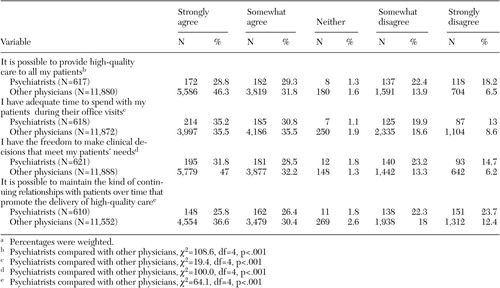 |
Table 2. Assessments of quality of inpatient services among physicians who participated in the 1996-1997 Community Tracing Study Physician Survey, by type of physiciana
a Percentages were weighted.
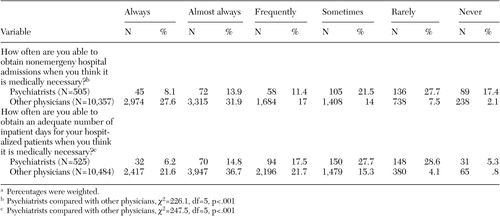 |
Table 3. Assessments of ability to obtain inpatient services among physicians who participated in the 1996-1997 Community Tracing Study Physician Survey, by type of physiciana
a Percentages were weighted.
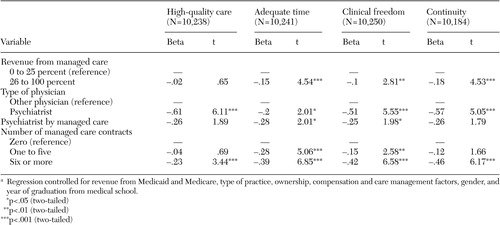 |
Table 4. Multiple regression models of the effects of managed care and physician type on physicians' quality assessmentsa
a Regression controlled for revenue from Medicaid and Medicare, type of practice, ownership, compensation and care management factors, gender, and year of graduation from medical school.
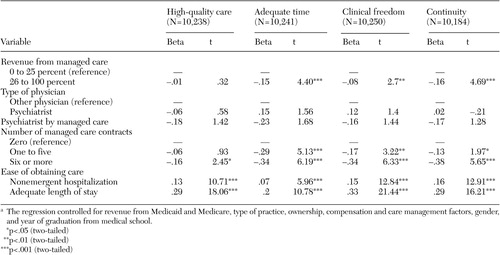 |
Table 5. Multiple regression models of the effects of managed care, physician type, and ability to obtain inpatient services on physicians' quality assessmentsa
a The regression controlled for revenue from Medicaid and Medicare, type of practice, ownership, compensation and care management factors, gender, and year of graduation from medical school.
1. McKusick D, Mark TL, King E, et al: Spending for mental health and substance abuse treatment, 1996. Health Affairs 17 (5):147–157, 1998Google Scholar
2. Mark TL, Coffey RM, King E, et al: Spending on mental health and substance abuse treatment, 1987–1997. Health Affairs 19 (4):108–120, 2000Google Scholar
3. Buck JA, Umland B: Covering mental health and substance abuse services. Health Affairs 16(4):120–126, 1997Google Scholar
4. Wickizer TM, Lessler D: Effects of utilization management on patterns of hospital care among privately insured adult patients. Medical Care 36:1545–1554, 1998Crossref, Medline, Google Scholar
5. Frank RG, Goldman HH, McGuire TG: Will parity in coverage result in better mental health care? New England Journal of Medicine 345:1701–1704, 2001Google Scholar
6. Hennessy KD, Goldman HH: Full parity: steps toward treatment equity for mental and addictive disorders. Health Affairs 20 (4):58–67, 2001Google Scholar
7. Sturm R, Pacula RL: Mental health parity and employer-sponsored health insurance in 1999–2000: I. Limits. Psychiatric Services 51:1361, 2000Link, Google Scholar
8. Pacula RL, Sturm R: Mental health parity and employer-sponsored health insurance in 1999–2000: II. Copayments and coinsurance. Psychiatric Services 51:1487, 2000Link, Google Scholar
9. Gitterman DP, Sturm R, Scheffler RM: Toward full mental health parity and beyond. Health Affairs 20(4):68–76, 2001Google Scholar
10. Goldman W, McCulloch J, Sturm R: Costs and use of mental health services before and after managed care. Health Affairs 17 (2):41–52, 1998Google Scholar
11. Oss ME, Drissel AB, Clary J: Managed Behavioral Health Market Share in the United States, 1997–98. Gettysburg, Penn, Behavioral Health Industry News, 1997Google Scholar
12. Huskamp HA: Episodes of mental heath and substance abuse treatment under a managed behavioral health care carve-out. Inquiry 36:147–161, 1999Medline, Google Scholar
13. Frank RG, Huskamp HA, McGuire TG, et al: Some economics of mental health 'carve-outs.' Archives of General Psychiatry 53:933–937, 1996Crossref, Medline, Google Scholar
14. Grembowski DE, Martin D, Patrick DL, et al: Managed care, access to mental health specialists, and outcomes among primary care patients with depressive symptoms. Journal of General Internal Medicine 17:258–269, 2002Crossref, Medline, Google Scholar
15. Merrick EL: Treatment of major depression before and after implementation of a behavioral health carve-out plan. Psychiatric Services 49:1563–1567, 1998Link, Google Scholar
16. Merrick EL: Effects of a behavioral health carve-out on inpatient-related quality indicators for major depression treatment. Medical Care 37:1023–1033, 1999Crossref, Medline, Google Scholar
17. Schoenbaum M, Zhang W, Sturm R: Costs and utilization of substance abuse care in a privately insured population under managed care. Psychiatric Services 49:1573–1578, 1998Link, Google Scholar
18. Huskamp HA: How a managed behavioral health care carve-out plan affected spending for episodes of treatment. Psychiatric Services 49:1559–1562, 1998Link, Google Scholar
19. Sturm R: The impact of practice setting and financial incentives on career satisfaction and perceived practice limitations among surgeons. American Journal of Surgery 183:222–225, 2002Crossref, Medline, Google Scholar
20. Sturm R: Effect of managed care and financing on practice constraints and career satisfaction in primary care. Journal of the American Board of Family Practice 15:367–377, 2002Medline, Google Scholar
21. Dickey B, Sharon-Lise TN, Norton EC, et al: Managing the care of schizophrenia: lessons from a 4-year Massachusetts Medicaid study. Archives of General Psychiatry 53:994–952, 1996Crossref, Google Scholar
22. Stein B, Orlando M, Sturm R: The effect of copayments on drug and alcohol treatment following inpatient detoxification under managed care. Psychiatric Services 51:195–198, 2000Link, Google Scholar
23. Busch AB, Frank RG, Lehman AF: The effect of a managed behavioral health carve-out on quality of care for Medicaid patients diagnosed as having schizophrenia. Archives of General Psychiatry 61:442–448, 2004Crossref, Medline, Google Scholar
24. Olmstead T, White WD, Sindelar J: The impact of managed care on substance abuse treatment services. Health Services Research 39:2, 2004Crossref, Google Scholar
25. Ray WA, Daugherty JR, Meador KG: Effect of mental health "carve-out" program on the continuity of anti-psychotic therapy. New England Journal of Medicine 348:1855–1894, 2003Crossref, Medline, Google Scholar
26. Manning WG, Liu CF, Stoner TJ, et al: Outcomes for Medicaid beneficiaries with schizophrenia under a prepaid mental health carve-out. Journal of Behavioral Health Services and Research 26:442–450, 1999Crossref, Medline, Google Scholar
27. Reschovsky J, Reed M, Blumenthal D, et al: Physicians' assessments of their ability to provide high-quality care in a changing health care system. Medical Care 39:254–269, 2001Crossref, Medline, Google Scholar
28. Sturm R, Ringel JS: The role of managed care and financing in medical practices: how does psychiatry differ from other medical fields? Social Psychiatry and Psychiatric Epidemiology 38:427–435, 2003Google Scholar
29. Kemper P, Blumenthal D, Corrigan JM, et al: The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 36:221–233, 1996Google Scholar
30. Potter F, Strouse R, Sinclair, et al: Report on Survey Methods for the Community Tracking Study's 1998–99 Round Two Physician Survey. Technical pub no 32. Washington, DC, Center for Studying Health System Change, 2001. Available at www.hschange.comGoogle Scholar
31. Community Tracking Study. Physicians Survey Summary File: User's Guide and Codebook. Technical pub no 29. Washington, DC, Center for Studying Health System Change, 2001. Available at www.hschange.comGoogle Scholar
32. Design and Methods for the Community Tracking Study. Center for Studying Health System Change. Available at www.hschange.org/index.cgi?data=01Google Scholar
33. Landon BE, Reschovsky J, Reed M, et al: Personal, organizational, and market level influences on physicians' practice patterns: results of a national survey of primary care physicians. Medical Care 39:889–905, 2001Crossref, Medline, Google Scholar
34. Smith MW, Chen S: Current trends in outpatient pharmacy in VA specialized mental health treatment. Psychiatric Services 55:315–317, 2004Link, Google Scholar
35. Mark TL, Coffey RM: What drove private health insurance spending on mental health and substance abuse care, 1992–1999? Health Affairs 22(1):165–172, 2003Google Scholar
36. Baker LC: Association of managed care market share and health expenditures for fee-for-service Medicare patients. JAMA 281:432–437, 1999Crossref, Medline, Google Scholar



