Predictors of the Stage of Residential Planning Among Aging Families of Adults With Severe Mental Illness
Abstract
OBJECTIVE: This study identified predictors of the extent of residential planning carried out by aging families of adults with severe mental illness according to the conceptual framework of the Double ABCX model of family coping and adaptation. METHODS: Mail surveys were completed by 157 mothers (mean age, 67 years) from 41 states who lived with and provided care to offspring with serious mental disorders (mean age, 38 years). Seventy-six percent of the offspring were men (N=120). Sixty percent of the offspring had been given a diagnosis of schizophrenia or schizoaffective disorder (N=94), 20 percent had multiple diagnoses (N=31), and 16 percent had bipolar disorder (N=25). RESULTS: Higher stages of planning were associated with use of avoidance as a means of coping, discussion of plans with the offspring with a disability, the desire to have family members assume future care responsibilities, lower subjective burden of providing care, and more self-perceived adverse age-related change. The model accounted for 20 percent of the variance in residential planning; over half of this variance was associated with coping behaviors and appraisals of the caregiving context. CONCLUSIONS: In addition to providing relevant information and alleviating feelings of intense burden that undermine residential planning, service providers can best assist older parents by encouraging them to recognize age-related changes in themselves that signal the need to plan and by helping them to involve the entire family in the planning process.
Between one- and two-thirds of adults with severe mental illness reside with their families, most with aging parents (1,2,3). As parents age, they face the reality that declining abilities and health problems will eventually limit their capacity to provide care (4). Thus it is not surprising that older parents repeatedly express great apprehension over what will happen to their offspring with severe mental illness when the parents become frail or pass away (1,3,5,6,7,8).
Aging parents must plan adequately for the future care of their offspring with lifelong disabilities. Without definite plans, offspring who outlive their parents may experience inappropriate emergency placements in an unprepared service system (9,10,11). However, if plans exist, relocation trauma can be averted by preparing offspring for the intended transition and by fostering independence (3,9,10). Moreover, until parents who are elderly make future plans, a sense of unfinished business may prevent acceptance of their impending death with equanimity (12).
Although the ability of aging parents to plan for the future has serious implications for families and the service system, only a handful of investigators have examined these issues (8,9,10,13). A consistent finding across these studies was that only 10 to 20 percent of older caregivers had made definite plans about future residential arrangements for their offspring with a disability. Yet one study also found that most parents (66 percent, or 104 parents) had established financial plans for their offspring with a disability (13). Thus, despite parents' awareness of the general need for planning, residential planning is an especially difficult problem for parents to resolve.
Research about factors that facilitate or impede residential planning among older parents with offspring with a disability has been scarce. Two studies involving older Israeli parents reported that caregivers who were overwhelmed with daily hassles were unable to take the necessary steps toward placement (14,15). Hatfield and Lefly (9) sampled 210 older caregivers from selected regions in the United States and found major obstacles to planning: personal problems of caregivers (anxiety about the future, insufficient knowledge, and limited finances), characteristics of the care recipient (resistance to change, refusal of help, and emotional instability), and characteristics of the service system (limited housing options and uncoordinated services). In Smith and colleagues' (13) national study of 157 older mothers, a majority of participants mentioned awareness of age-related changes in themselves or their spouses as the primary reason for planning, indicated the need for help with planning, and wished that their offspring without a disability would assume future care.
Although these past studies provide insight into variables that might affect which stage of residential planning older parents are in, the findings of these studies are inconclusive. One shortcoming is that these studies examined mainly caregivers who were not representative of the U.S. population. Two studies involved samples of older Israeli parents (14,15), and the third sampled older American parents and other relatives from only a few states (9). These studies were also largely atheoretical and did not build on past research with similar caregiver populations. Finally, because the investigators relied primarily on univariate statistics, they did not consider how multiple variables act together to affect planning.
The study reported here examined predictors of future residential planning among a national sample of older mothers who care at home for their offspring with severe mental illness. The predictors were examined within the multivariate framework of the Double ABCX model of family stress and coping (16). Consensus exists that family outcomes are best understood from a stress and coping paradigm (17,18), and the Double ABCX model has been used in past research to identify predictors of residential planning among older parents of adults with mental retardation (19,20).
In the Double ABCX model, A refers to objective stressors of caregiving; B indicates mediators, specifically resources and coping behaviors that are used in response to stressors; C conveys family members' appraisals of the situation; and X denotes a relevant family outcome (16). Hypothesized causality leads from objective stressors (A) to appraisals (C), with the impact of the stressors and appraisals on the outcome (X) being mediated by resources and coping skills (B). Double refers to the accumulation of problems that are secondary to caregiving, such as changes in caregivers' functional ability, that effect adaptation.
In this study, the stage of residential planning that was reported by older mothers was the outcome. Following the Double ABCX framework, independent variables were classified as objective stressors, appraisals, or mediators (resources and coping behaviors). The study's hypothesis was that mediators and appraisals would have more of a proximal effect on residential planning than objective stressors. Several positive aspects of family caregiving were also included, given recent claims about the explanatory importance of resilience among families of adults with lifelong disabilities (21). Background characteristics that might influence residential planning were considered as well. Table 1 summarizes the proposed model and states the hypothesized relationship between each predictor variable and stage of residential planning (4,9,10,15,18,19,20,22,23,24,25,26,27,28,29).
Methods
Participants
The sample used in this study was identical to that from an earlier descriptive study of permanency planning by Smith and colleagues (13). Mothers aged 50 years and older who lived with a mentally ill offspring were recruited between 1995 and 1997 through announcements in newsletters from the National Alliance for the Mentally Ill. Participation was restricted to mothers because they tend to be the primary caregiver (6).
The recruitment yielded 196 mothers from 41 states, 157 of whom met the criteria of living with their offspring. Participants' mean±SD age was 67±7.7 years. A total of 144 participants (92 percent) were non-Hispanic white, 96 (61 percent) were married, 154 (98 percent) had at least a high school education, and 124 (79 percent) reported their health as good or excellent. Offspring were considered to have diagnoses of severe mental illness if they were reported by their mothers to have diagnoses of schizophrenia or schizoaffective disorder (94 offspring, or 60 percent), multiple disorders (31 offspring, or 20 percent), bipolar disorder (25 offspring, or 16 percent), or other severe psychiatric illnesses (7 offspring, or 5 percent). A total of 120 offspring were men (76 percent), and their age ranged from 20 to 58 years (mean, 38±8.2 years). Most offspring (114, or 73 percent) were rated by their mothers to be in good or excellent physical health. A third of offspring (N=52) engaged in activities outside the home (for example, day programs), whereas half (N=78) spent their typical day at home. Seventy-three mothers (47 percent) reported that their offspring relied on them for help with everyday chores, and 64 mothers (41 percent) reported that their offspring relied on them for help with chores plus daily structure.
This sample was similar to that found in previous studies involving the National Alliance for the Mentally Ill, in which the typical family pattern has been an aging parent, usually a mother in her late 50s to 70s, who cares for a son approaching middle age (30).
Procedure
Mothers who indicated by phone or mail that they were willing to participate in the study were mailed a questionnaire about their family caregiving circumstances and a letter of informed consent (N=171). The questionnaire was adapted from an instrument used in a previous study that surveyed older mothers of adults with mental retardation (20). Ninety-two percent (N=157) of the surveys were completed by eligible respondents and returned in a self-addressed stamped envelope. The study was approved by the institutional review board at the University of Maryland, College Park.
Measures
Stage of residential planning was assessed by asking respondents to indicate which of five ascending stages best described their current state of planning for the future residence of their offspring: "No discussions have occurred yet"; "Some discussions have occurred, but they were not serious"; "There has been serious consideration of residential alternatives"; "Some plans have been made, but they are not definite"; and "Definite plans are made." This measure originated in previous research about older mothers of adults with mental retardation (20) and coincided with the view that residential planning is a protracted process (31). The instruments that were used to assess the predictor variables are summarized in Table 1.
Data analysis
A hierarchical regression analysis was performed by using SPSS 10.0 for Windows to examine individual predictors of residential planning stage. Predictors were organized into blocks on the basis of the Double ABCX model (16). This procedure yielded five equations in which each block was entered according to the prioritized logic of the model. This procedure also permitted simultaneous control of each independent factor in the model.
Results
Only 17 mothers (11 percent) reported that definite residential plans had been made for their offspring, whereas 28 (18 percent) reported having plans that were not definite. Thirty mothers (19 percent) reported serious consideration or discussion of alternatives, 58 (37 percent) reported discussions that were not serious, and 24 (15 percent) had given this matter no attention.
Zero-order correlations, means, standard deviations, and the observed range for all model variables are presented in Table 2. Higher stages of residential planning were associated at statistically significant levels with the mother's age, less use of avoidance as a means of coping, discussion of residential plans with the offspring with a disability, the desire to have family members assume future care responsibilities, and lower subjective burden of providing care. None of the objective stressors or family resources were significantly related to stage of planning at the bivariate level.
The results of the hierachical regression analysis based on the Double ABCX model are shown in Table 3. The SPSS collinearity diagnostic statistics (that is, tolerance, variation inflation index, and condition index) revealed no multicollinearity problems among the model's independent variables. Inspection of P-P (probability-probability) and residual plots revealed that multiple regression assumptions about normality (kurtosis=−.876), linearity, and homoscedasticity were met.
As hypothesized, variables that were categorized as appraisals and coping behaviors were the strongest predictors of the stage of residential planning. Higher stages of planning were associated with less avoidance coping, discussion of plans with the offspring with a disability, the desire to have family members assume future care responsibilities, lower subjective burden, and greater self-perception of adverse age-related change. The model accounted for 20 percent of the variance in residential planning, and more than half of this variance was associated with coping behaviors and appraisals.
Discussion
Contrary to the study hypotheses, neither the objective stressors of caregiving nor the resources available to the family were significantly related to the stage of residential planning. However, consistent with the Double ABCX model, the bivariate correlations suggest that some variables in these categories may exert indirect effects on planning. For example, the two appraisals that emerged as the strongest predictors of planning stage in the regression analysis—the mothers' greater subjective burden and self-perception of adverse age-related change—were found at the bivariate level to be associated with more behavioral problems and less family cohesion. It is also noteworthy that the mothers' age remained a significant predictor of planning stage throughout the regression analysis until the mothers' appraisals of self and the caregiving situation were entered into the final equation. These findings suggest that greater subjective burden and the perception of becoming older, rather than chronological age itself, instigate residential planning.
Consistent with past research about this population, only a small percentage of older mothers in the study reported here had made definite plans for future living arrangements of their offspring (8,9,10,13). Moreover, use of avoidance coping was inversely related to stage of planning at both the univariate and the multivariate levels of analysis. These findings reinforce previous assertions that future planning is an arduous and tormenting process to undertake for older parents of adults with lifelong disabilities of any type (3,4,20). Therefore, it is not surprising that several additional findings of the study reported here bear a striking similarity to those previously observed among older mothers of adults with mental retardation.
As in previous research on parents of adults with mental retardation (20), the objective demands of caregiving had a less immediate effect on residential planning than either coping behaviors or appraisals. Also, as with past research on older mothers of adults with mental retardation, the appraisal of being adversely affected by the aging process was one of the strongest predictors of residential planning stage. Thus it appears that the decision of aging parents to execute residential planning is affected more by parents' self-perceived ability to persist in the caregiver role than by the actual demands of caregiving. If parents' awareness of becoming more disabled provokes realization of the need to plan, then practitioners face the task of assisting those who have not yet planned to engage in self-exploration of their increasing limitations (20).
Subjective burden is another appraisal found to be related to residential planning in both the study reported here and in research about older mothers of adults with mental retardation (20). The tendency for parents who reported a higher burden to engage in less planning may be explained, in part, by past research about family members who care for persons who are frail and elderly (32). This research showed that the competing demands of caregiving induced "tendencies to denyor dismiss the stressfulness of events in order to reduce the amount of informationor arousal requiring immediate attention" (32). Similarly, Rimmerman and Keren (15) asserted that parents of adults with severe mental illness who feel overwhelmed with daily hassles are unable to take necessary steps toward placement, such as getting information about residential settings or exploring the procedures needed for application. Thus older parents who feel intensely burdened by immediate caregiving responsibilities may lack sufficient energy or patience to confront the demanding task of residential planning. Yet, in the absence of longitudinal data, one cannot rule out the opposite direction of causality wherein older mothers of adults with long-term disabilities may feel less burdened after taking steps toward resolving the future of their offspring.
Another similarity between aging mothers of adults with mental illness and aging mothers of adults with mental retardation concerns the use of avoidance in facing the demands of planning. As in the study reported here, increased use of avoidance was found in previous studies to be related to less residential planning among older mothers of adults with mental retardation (20,33). According to Cook (6), one reason that older mothers shun planning is to preserve what little self-esteem their offspring have left by avoiding situations that might lead to failure or further deterioration, such as moving away from the parental home. Joffres (10) similarly reported that older parents do not involve offspring with disabilities in planning because parents fear that such involvement would devastate their offspring. Moreover, research on family caregiving to persons who are elderly suggests that denial of the negative consequences of aging limits discussions of the future as caregiving dyads avoid thinking and talking about what lies ahead (34). Thus practitioners should realize that denial of what the future may hold is an issue that transcends multiple caregiving contexts.
Another key finding of the study is that mothers who involved their offspring in discussions about the future were further along in residential planning than those who did not. This finding coincides with Joffre's (10) observation that the end of co-residence often reflects the desire of the mentally ill offspring or has been initiated by the offspring, a phenomenon not uncommon among offspring with mental retardation. Although Hatfield and Lefly (9) claim that families can be stymied in their planning efforts if their relative with severe mental illness refuses to go along with the plans made, fewer than half of the older mothers in the sample from this study who had involved their offspring in planning discussions also reported parent-offspring agreement about these discussions (13). This finding suggests that parents may need help from mental health professionals with involving the offspring in the planning process and resolving family disagreements about the offspring's future living arrangements.
Greater residential planning was also associated with the desire to have family members as future caregivers, even though only one-quarter of older mothers thought such arrangements would definitely occur (13). This finding reinforces the conclusion of other authors that family discussions, especially those involving siblings of the offspring with a disability, are an important component of the planning process (20,27,28). Thus, in addition to learning about available resources and how to obtain them, many families need help with involving siblings and other family members in future care (9).
Contrary to the study hypotheses, neither the use of formal services nor the availability of informal support from siblings of the offspring with severe mental illness was significantly related to residential planning stage at either the bivariate or the multivariate levels. This finding is remarkably different from past research in which these two variables were found to have direct positive effects on residential planning stage among older mothers of adults with mental retardation (20). One likely explanation for these discrepant findings is that mothers of adults with mental illness typically have smaller social support networks and fewer substitute caregivers to call on because of the higher levels of social stigma and disruptive behaviors that are associated with mental illness (35,36,37).
Evidence also exists that older parents of adults with severe mental illness view their overall interaction with the service system as unsatisfactory and a contributing factor to their overall burden (7,22). On the other hand, Hatfield and Lefly (9) noted that older caregivers had little criticism about professional assistance with planning. Instead, older caregivers attributed obstacles to planning to themselves and to their relative than to the service system. Nevertheless, very few older parents actually turn to mental health professionals for planning assistance (9,13,15).
Several limitations of the study reported here are noteworthy. First, despite a national scope, the sample was self-selected, drawn entirely from National Alliance for the Mentally Ill membership, and lacked ethnic and cultural diversity. Second, without longitudinal data it is impossible to draw firm conclusions about the directionality of the hypothesized relationships between variables. As mentioned above, for some relationships, causality may actually be in the opposite direction than hypothesized here. Third, all data were self-reported by study participants and may not reflect their true planning behaviors. Fourth, by focusing on planning stage, this study overlooked other facets of planning and placement, such as future intentions to place, preferences for placement, requests for placements, urgency of placement, and actual placement (38).
The low amount of variance (20 percent) explained in the multiple regression analysis indicates that the proposed model does not include all meaningful predictors of residential planning. Future research is needed to explore the potential impact of other factors, such as the specific roles of offspring with severe mental illness and other family members in the planning process, as well as characteristics of the service system that either facilitate or impede residential planning by aging families.
Conclusions
Despite the limitations of this study, it sheds important new light on a virtually unexplored topic of great relevance to adults with severe mental illness, their families, and the service system intended to meet their needs. Most notably, the findings suggest that in addition to providing relevant information and alleviating the subjective burden that undermines residential planning, service providers can best assist older parents by encouraging them to acknowledge age-related changes that signal the need to plan and by helping them to involve the entire family in the planning process.
Acknowledgment
This study was funded by the Graduate Research Board at the University of Maryland, College Park.
Dr. Smith is affiliated with the School of Family and Consumer Studies at Kent State University, 144 Nixson Hall, Kent, Ohio 44242 (e-mail, [email protected]).
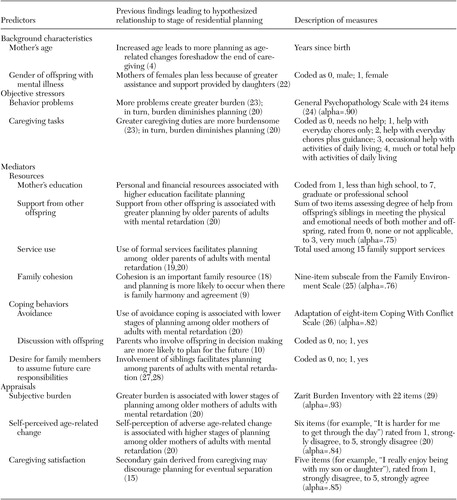 |
Table 1. Summary of proposed model and measures used to predict the residential planning stage among 157 aging mothers of adults with mental illness
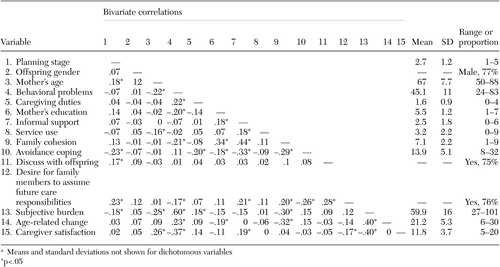 |
Table 2. Bivariate correlations, means, standard deviations, and observed ranges for model variables among 157 aging mothers of adults with mental illnessa
a Means and standard deviations not shown for dichotomous variables
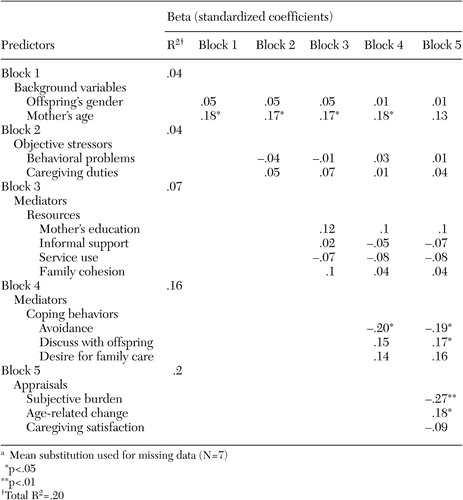 |
Table 3. Results of regression analysis of residential planning stage on predictors among 157 aging mothers of adults with mental illnessa
a Mean substitution used for missing data (N=7)
1. Lefly HP: Aging parents as caregivers of mentally ill adult children: an emerging social problem. Hospital and Community Psychiatry 38:1063–1070, 1987Abstract, Google Scholar
2. Skinner EA, Steinwachs DM, Kasper JD: Family perspectives on service needs of people with serious and persistent mental illness. Innovations and Research 1(3):23–30, 1992Google Scholar
3. Lefley HP, Hatfield AB: Helping parental caregivers and mental health consumers cope with parental aging and loss. Psychiatric Services 50:369–375, 1999Link, Google Scholar
4. Jennings J: Elderly parents as caregivers for their adult dependent children. Social Work 32:430–433, 1987Medline, Google Scholar
5. Cohler BJ, Pickett SA, Cook JA: The psychiatric patient grows older: issues in family care, in Aging and Caregiving. Edited by Liebowitz BE, Light E. New York, Springer, 1991Google Scholar
6. Cook JA: Who "mothers" the chronically mentally ill? Family Relations 27:42–49, 1988Google Scholar
7. Francell CG, Conn VS, Gray DP: Families' perceptions of burden of care for chronic mentally ill relatives. Hospital and Community Psychiatry 39:1296–1300, 1988Abstract, Google Scholar
8. Kaufmann AV: Older parents who care for adult children with serious mental illness. Journal of Gerontological Social Work 29:35–55, 1998Crossref, Google Scholar
9. Hatfield AB, Lefly HP: Helping elderly caregivers plan for the future care of a relative with mental illness. Psychiatric Rehabilitation Journal 24:103–107, 2000Crossref, Google Scholar
10. Joffres C: Barriers to residential planning: perspectives from selected older parents caring for adult offspring with lifelong disabilities. Canadian Journal on Aging 21:303–311, 2002Crossref, Google Scholar
11. Smith GC, Tobin SS: Practice witholder parents of developmentally disabled adults. Clinical Gerontologist 14:59–77, 1993Crossref, Google Scholar
12. Smith GC,TobinSS: Permanency planning among older parents of adults with lifelong disabilities. Journal of Gerontological Social Work 14:35–59, 1989Crossref, Google Scholar
13. Smith GC, Hatfield A, Miller D: Future planning by older mothers of adults with serious mental illness. Psychiatric Services 55:1162–1166, 2000Link, Google Scholar
14. Duvdevany I, Keren N: Thought, consideration, and future planning for out-of-home placement among parental caregivers of dependent adult children with psychiatric disabilities. International Journal of Rehabilitation Research 25:207–213, 2002Crossref, Medline, Google Scholar
15. Rimmerman A, Keren N: Letting go: parental attitudes toward out-of-home placement of their children with psychiatric disability. Psychiatric Rehabilitation Journal 19:3–8, 1995Crossref, Google Scholar
16. McCubbin HI, Patterson JM: Family adaptation to crises, in Family Stress, Coping, and Social Support. Edited by McCubbin HI, Cauble AE, Patterson, JM. Springfield, Thomas, 1982Google Scholar
17. Gatz M, Bengtson VL, Blum MJ: Caregiving families, in Handbook of the Psychology of Aging, 3rd ed. Edited by Birren JE, Schaie KW. New York, Academic Press, 1990Google Scholar
18. Rungreangkulkij S, Gillis, CL: Conceptual approaches to studying family caregiving for persons with severe mental illness. Journal of Family Nursing 6:341–366, 2000Crossref, Google Scholar
19. Pruchno RA, Patrick JH: Effects of formal and familial residential plans for adults with mental retardation on their aging mothers. American Journal on Mental Retardation 104:38–52, 1999Crossref, Medline, Google Scholar
20. Smith GC, Tobin SS, Fullmer EM: Elderly mothers caring at home for offspring with mental retardation: a model of permanency planning. American Journal on Mental Retardation 99:487–499, 1995Medline, Google Scholar
21. Lustig DC: Family caregiving of adults with mental retardation: key issues for rehabilitation counselors. Journal of Rehabilitation 65:26–35, 1999Google Scholar
22. Cook JA, Cohler BJ, Pickett SA, et al: Life-course and severe mental illness: implications for caregiving within the family of later life. Family Relations 46:427–436, 1997Crossref, Google Scholar
23. Lukissa DA: Family burden in chronic mental illness: a review of research studies. Journal of Advanced Nursing 21:248–255, 1995Crossref, Medline, Google Scholar
24. Katz MM, Lyerly SB: Methods for measuring adjustment and social behavior in the community:1. Rationale, description, discriminative validity, and scale development. Psychological Reports 13:503–535, 1963Google Scholar
25. Moos RH, Moos BS: Family Environment Scale Manual, 2nd ed. Palo Alto, Calif, Consulting Psychologists Press, 1986Google Scholar
26. Fiefel H, StrockS: Coping with conflict situations: middle aged and elderly men. Psychology and Aging 4:26–33, 1989Crossref, Medline, Google Scholar
27. Pruchno RA, Patrick JH, Burant CJ: Mental health of aging women with children who are chronically disabled: examination of a two-factor model. Journal of Gerontology: Social Sciences 51B:S284-S296, 1996Google Scholar
28. Seltzer G, Begun A, Seltzer MM, et al: Adults with mental retardation and their aging mothers: impacts on siblings. Family Relations 40:310–317, 1991Crossref, Google Scholar
29. Zarit SH, Zarit JM: The Memory and Behavior Problem Checklist and the Burden Interview. Technical Report, Pennsylvania State University, 1983Google Scholar
30. Lefly HP: Family Caregiving in Mental Illness. Thousand Oaks, Calif, Sage, 1996Google Scholar
31. Blacher J, Hanneman R: Out-of-home placement of children and adolescents with severe handicaps: behavioral intentions and behavior. Research in Developmental Disabilities 14:145–160, 1993.Crossref, Medline, Google Scholar
32. Stephens MAP, Norris VK, Kinney JM, et al: Stressful situations in caregiving: relations between caregiver coping and well-being. Psychology and Aging 3:208–209, 1988Crossref, Medline, Google Scholar
33. Prosser H: The future care plans of older adults with intellectual disabilities living at home with family carers. Journal of Applied Research in Intellectual Disabilities 10:15–32, 1997Crossref, Google Scholar
34. Pecchioni LL: Implicit decision-making in family caregiving. Journal of Social and Personal Relationships 18:219–237, 2001Crossref, Google Scholar
35. Greenberg JS, Seltzer MM, Greenley JR: Aging parents of adults with disabilities: the gratifications and frustrations of later-life caregiving. Gerontologist 33:542–550, 1993Crossref, Medline, Google Scholar
36. Greenberg JS, Seltzer MM, Krauss MW, et al: The differential effects of social support on the psychological well-being of aging mothers of adults with mental illness or mental retardation. Family Relations 46:383–394, 1997Crossref, Google Scholar
37. Lefly HP: Synthesizing the family caregiving studies: implications for service planning, social policy, and further research. Family Relations 46:443–450, 1997Crossref, Google Scholar
38. Essex EL, Seltzer MM, Krauss MW: Residential transitions of adults with mental retardation: predictors of waiting list use and placement. American Journal on Mental Retardation 101:613–629, 1997Medline, Google Scholar



