Patients' and Staff's Perceptions of the Psychiatric Ward Environment
Abstract
OBJECTIVE: This study examined the extent to which patients' and staff's perceptions of the psychiatric ward atmosphere and the working conditions of staff influence patient and staff satisfaction. METHODS: A total of 640 staff members on 42 wards completed the Ward Atmosphere Scale (WAS) and the Working Environment Scale-10 (WES-10). A total of 424 patients on the same wards completed the WAS. Both patients and staff members answered three questions about their general satisfaction with the ward. The ward means were used as the unit of analysis. RESULTS: The staff members had significantly higher scores than the patients on nine of the 11 WAS subscales. Patients' and staff's WAS scores were moderately correlated. No significant correlation was found between patients' and staff's scores on the three satisfaction items. Patient satisfaction was strongly correlated with patients' WAS scores and was moderately correlated with staff's WAS scores but was not significantly correlated with staff's WES-10 scores. Staff satisfaction was moderately correlated with staff's WAS and WES-10 scores but was not correlated with patients' WAS scores. CONCLUSIONS: Different aspects of the treatment climate seem to be important for patient and staff satisfaction. The ward atmosphere seems to be more important for patient satisfaction than for staff satisfaction. The working environment is strongly related to staff satisfaction but seems to be unrelated to patient satisfaction.
Although patients who have psychoses are treated primarily in the community, inpatient units play an important role in the treatment of patients who have severe psychotic disorders and suicidality (1,2). Several studies have demonstrated the importance of the treatment environment for inpatients with psychoses (3,4,5,6,7,8). The Ward Atmosphere Scale (WAS) is the most widely used instrument for capturing aspects of the treatment environment (9).
The ward atmosphere may be experienced differently by different groups, giving the impression that patients and staff live in "different worlds," even though they share the same physical and social environment (10,11,12,13,14). These differences in perception are important, because they directly challenge the common views that staff's perceptions of the ward atmosphere reflect those of inpatients (15,16) and that patients' and staff's WAS scores can be pooled (17,18).
Studies of differences between patient's and staff's perceptions of the treatment environment have had inconsistent results (19,20,21,22), probably because the studies have used individual WAS scores, whose reliability is unsatisfactory for most subscales (23). In contrast, mean WAS scores have satisfactory reliability. However, to our knowledge, only two studies have examined differences between patient's and staff's scores at the ward level. Moos (10) found that staff's scores were higher on all the WAS subscales except for the order and organization subscale, on which staff and patients had equal scores, and the staff control subscale, on which staff had lower scores. Friis (24) replicated these findings, except that staff's scores were lower on the order and organization subscale in that study.
To better understand the different perspectives of patients and staff, it is important also to examine other aspects of the treatment climate, such as patient and staff satisfaction, and the work environment as perceived by staff. Patient satisfaction is considered to be a critical health care indicators (25). The potentially stressful nature of a poor work environment is associated with reduced job satisfaction, absenteeism, somatic complaints, burnout, and depression among staff (26,27,28,29,30).
However, only two studies have examined various aspects of staff's working conditions and patient satisfaction. Garman and colleagues (31) found a significant positive relationship between staff burnout and patient satisfaction. Corrigan and associates (32) found a strong relationship between different styles of team leadership and consumer satisfaction. To our knowledge, no previous studies have explicitly examined the relationship between the core dimensions of the working environment and patient satisfaction. We undertook such an investigation by including a short and user-friendly working-environment questionnaire comprising ten items—the Working Environment Scale-10 (WES-10). The WES-10 has been shown to measure the core dimensions of the work environment (33).
Our main aim was to further examine the different perspectives of patients and staff. First, we wanted to examine whether we would obtain the same findings as those of Moos (10) and Friis (24), which showed that patients and staff perceive the ward atmosphere differently. Because many aspects of inpatient treatment have changed since the 1970s—for example, inpatient stays are shorter, and a higher percentage of patients have psychoses—these earlier findings need to be replicated in the current inpatient setting. Second, we wanted to examine the relationship between patient and staff satisfaction and the extent to which patient and staff satisfaction are related to WAS and WES-10 scores. We hypothesized that patient and staff satisfaction would be significantly correlated and that the working environment as perceived by staff would be significantly correlated with patient satisfaction. Furthermore, we hypothesized that WAS scores would be most strongly correlated with patient satisfaction and that WES-10 scores would be most strongly correlated with staff satisfaction.
Methods
During the period 1990 through 2000 a total of 640 staff members on 42 wards for psychotic patients completed the WAS and the WES-10. A total of 424 inpatients on the same wards completed the WAS during the same period. All data were collected within five days on each ward, and each ward was rated only once. All the psychiatric wards were part of the community hospital system in Norway. The chairman of the regional ethical committee approved the study.
Most of the wards were short-term wards (36 wards), but six intermediate and long-term wards were also included. We included wards only when more than two-thirds of the patients had diagnoses within the psychotic range. So that reliable means would be obtained for each ward, at least five patients had to complete the WAS. If fewer than five patients on a ward completed the questionnaires, that ward was excluded from the study. All staff members—physicians, psychologists, nurses, and aides—were included in the study. Night staff were excluded, however, because of difficulties in obtaining an acceptable number of completed questionnaires from the night staff. Each staff member was asked about his or her duration of employment on the psychiatric ward. Ninety-six staff members (15 percent) had been employed for less than six months, 141 (22 percent) between six months and 18 months, 128 (20 percent) between 18 months and three years, and 275 (43 percent) for more than three years.
Staff and patients participated in the study on a voluntary basis. Participants were asked to complete a modified version of the WAS for the ward as they experienced it, or a "real ward" WAS (WAS-R). The WAS-R is a self-report questionnaire containing 100 statements about the ward, each requiring a true or false answer. We used a revised version of the WAS-R comprising 80 items, as described previously (23,34). In addition, we modified the true-or-false format to a 4-point scale ranging from 0, totally disagree, to 3, totally agree.
The revised WAS comprised 11 subscales: involvement (a measure of how active and energetic patients are in the program), support (a measure of how much patients help and support each other and how supportive the staff are toward patients), spontaneous behavior (a measure of the level of open expression of feelings by patients and staff), autonomy (a measure of how self-sufficient and independent patients are in making their own decisions), practical orientation (a measure of the extent to which patients learn practical skills and are prepared for release from the program), personal problem orientation (a measure of the extent to which patients seek to understand their feelings and personal problems), angry and aggressive behavior (a measure of how much patients argue with other patients and staff, become openly angry, and display other aggressive behavior), order and organization (a measure of how important order and organization are in the program), program clarity (a measure of the extent to which patients know what to expect in their day-to-day routine and the explicitness of program rules and procedures), staff control (a measure of the extent to which the staff use procedures to keep patients under necessary controls), and staff's attitude toward expressed feelings (a measure of the extent to which staff encourage patients to express their feelings openly).
The WES-10 is also a self-report questionnaire. The staff rated the items on a 5-point scale ranging from 1, totally disagree, to 5, totally agree. The WES-10 measures four clinically meaningful subscales and has been examined in a previous study (33). The four subscales are self-realization (a measure of the extent to which the staff members feel supported and whether they feel that they are able to use their knowledge working on the ward), workload (a measure of the number of tasks imposed on the staff members and the extent to which they feel that they should have been in several places at the same time), conflict (a measure of the extent to which the staff members experience conflicts and loyalty problems), and nervousness (a measure of the extent to which staff are worried about going to work and the extent to which they feel nervous or tense on the ward). The mean±SD scores for the four subscales were 3.64±.22 for self-realization, 3.42±.36 for workload, 2.06± .28 for conflict, and 1.99± .21 for nervousness.
Both patients and staff responded to three questions developed by Moos (35) to capture general satisfaction: How satisfied are you with this ward?; How much do you like the patients on this ward?; and How much do you like the staff on this ward? The questions were rated on a 5-point scale ranging from 1, very unsatisfied, to 5, very satisfied. The staff members' mean±SD scores on these three questions were 4.03±.33 for question 1; 4.20±.20 for question 2; and 4.43±.21 for question 3. The patients' respective scores on the same questions were 3.74±.46, 3.82±.31, and 4.05±.43.
In a previous study (23), we found that even if the internal consistency of the WAS subscales was doubtful at an individual level, it was satisfactory at the ward level. This finding is in accordance with the literature, which suggests that a Cronbach's alpha greater than .7 is satisfactory for individual comparisons and that a Cronbach's alpha greater than .5 is satisfactory for group comparisons (36,37). Consequently, the ward means were used in all the statistical analyses of the WAS subscales, the WES-10 subscales, and the three general satisfaction items. Because we had changed the original true-or-false rating scale (0 or 1) to a 4-point scale ranging from 0 to 3, we divided the sum of the item scores by 3. Because of the reduced number of items, we divided the sum score by the total number of items included and multiplied the resultant value by 10. This approach allowed us to compare the mean values obtained in this study with the mean values obtained in previous studies that used the original ten-item, 2-point scale. Consequently, the mean WAS subscale scores reported here range from 0 (low) to 10 (high).
Nonpaired t tests were used to analyze the differences between patients' and staff members' perceptions of the ward atmosphere. Correlations between the WAS subscales, WES-10 subscales, and general satisfaction items were calculated as Pearson product-moment coefficients. Data were analyzed by using the Statistical Package for the Social Sciences (version 11.0).
Results
As can be seen from Table 1, the mean scores for staff were significantly higher than those for patients on nine of the 11 WAS subscales. No significant difference between groups was found on the order and organization subscale, whereas the staff scored significantly lower than the patients on the staff control subscale.
The subscale scores for patients and staff were moderately correlated. The strongest correlation was between autonomy scores (r=.58), and the weakest correlation was between spontaneous behavior scores (r=.27). The median intercorrelation coefficient was .41. No significant correlations were found between patients and staff on the three satisfaction items.
As can be seen from Table 2, patients' WAS scores were strongly correlated with the three patient satisfaction items but not with the three staff satisfaction items. Table 3 shows that the staff WAS scores were fairly strongly correlated with the three staff satisfaction items. The staff perceptions of involvement, personal problem orientation, and angry and aggressive behavior were also significantly correlated with the patients' general liking for the ward. Tables 2 and 3 indicate that satisfaction was more strongly linked to perceived ward atmosphere for patients than for staff, probably because staff satisfaction is also strongly dependent on the work environment.
As can be seen from Table 4, the work environment scores were strongly correlated with staff members' general liking of the ward, liking of patients, and liking of staff. In contrast, no significant relationship was found between the three patient satisfaction items and the work environment as perceived by staff.
Discussion and conclusions
Our finding that WAS scores were significantly higher among staff than among patients on nearly all WAS subscales is consistent with the findings of Moos (10) and Friis (24). Both our data and data from those studies suggest that staff tend to view the treatment environment more favorably than do patients. As pointed out by Main and colleagues (38), staff's perceptions are expected to be higher on dimensions that represent positive aspects of their roles and lower in areas that could have negative implications. This expectation is consistent with our results, with the exception of the angry and aggressive behavior subscale scores. A low level of angry and aggressive behavior has been associated with a better treatment outcome and a higher level of patient satisfaction (7,39,40,41).
Our study showed no significant correlation between patient and staff satisfaction and no significant relationship between patient satisfaction and the work environment as perceived by staff. The main reason for the lack of correlation between patient and staff satisfaction may be that different aspects of the treatment environment are related to patient and staff satisfaction. Patient satisfaction was strongly correlated with patients' WAS scores and was moderately correlated with staff's WAS scores but was not correlated with WES-10 scores. In contrast, staff satisfaction was moderately correlated with staff's WAS and WES-10 scores but not with patients' WAS scores.
Consequently, it appears that the ward atmosphere is more important for patient satisfaction than for staff satisfaction. It is important to consider the different roles and viewpoints of patients and staff, each of whom are on the ward for different reasons. Most notable is that, unlike most of the patients, staff members can leave the ward after their shifts and may withdraw from the ward milieu if they experience it as too stressful. Thus the ward atmosphere is likely to be more important for patient satisfaction than for staff satisfaction.
Several studies have shown a significant relationship between the work environment and burnout among mental health workers (26,27,28,29,30). Garman and associates (31) found a significant relationship between burnout and patient satisfaction in inpatient and community programs that used psychosocial rehabilitation approaches. On the basis of the results of these studies, we expected to find a significant correlation between patient and staff satisfaction. The main reason for the contrary results in our study may be that we examined primarily short-term units. A shorter inpatient stay may give patients less access to different aspects of the treatment environment and may strengthen the impression that patients and staff live in "different worlds." This explanation is supported to some extent by the stronger correlation between patients' and staff's WAS scores in a sample from the 1970s (42), when patients were admitted for a longer time than in our study. The average correlations between patients' and staff's WAS scores were .61 in the 1970s (24) and .41 in our study.
It is possible that our study would have had different results if all patients and staff members had completed the questionnaires. We did not collect information about patients who did not complete the questionnaires. It is possible that the patients who refused or were unable to complete the questionnaires were the more severely disturbed patients. However, in a previous study (8), perceptions of the ward atmosphere did not differ between the more severely disturbed patients and other patients. Moreover, an average of ten patients completed the questionnaires on each ward, which should have minimized any possible selection bias.
We used three questions to capture general satisfaction with the treatment climate. It could be argued that a more sophisticated instrument would have yielded different results. The reliability of these three items has not been examined. However, the use of ward means instead of individual scores increases the reliability of the satisfaction scores (43).
Our study provides new information about the different perspectives of patients and staff on the treatment environment. The ward atmosphere seems to be most important for patient satisfaction, and staff tend to view the treatment environment more favorably than do patients. Our data suggest that patients' and staff's scores should be analyzed separately and not pooled to provide one single measurement of the treatment environment. Furthermore, our data suggest that the commonly held view that the working conditions of staff influence patient satisfaction and their perceptions of the treatment environment needs to be moderated.
The authors are affiliated with the division of psychiatry of Ulleval University Hospital, N-0407 Oslo, Norway (e-mail, [email protected]).
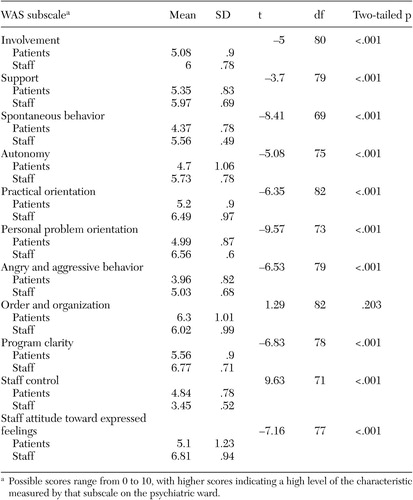 |
Table 1. Differences between patients' and staff's scores on the 11 subscales of the Ward Atmosphere Scale (WAS) (N=640 staff and 424 patients)
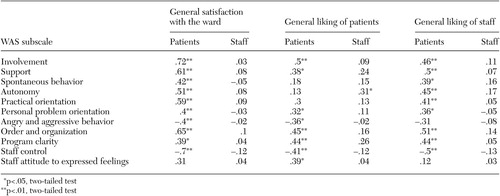 |
Table 2. Correlations between patients' scores on subscales of the Ward Atmosphere Scale (WAS) and patients' and staff's general liking of the ward, general liking of patients, and general liking of staff
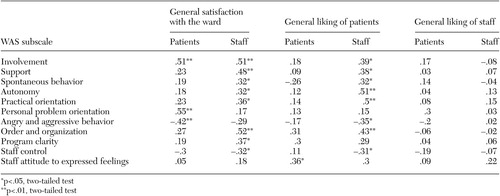 |
Table 3. Correlations between staff's scores on subscales of the Ward Atmosphere Scale (WAS) and patients' and staff's general liking of the ward, general liking of patients, and general liking of staff
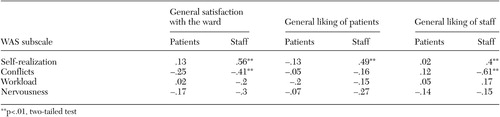 |
Table 4. Correlations between scores on the Working Environment Scale 10 and the general satisfaction items of the Ward Atmosphere Scale (WAS) for patients and staff
1. Rittmannsberger H, Pachinger T, Keppelmuller P, et al: Medication adherence among psychotic patients before admission to inpatient treatment. Psychiatric Services 55:174–179, 2004Link, Google Scholar
2. Dilonardo JD, Connelly CE, Seifert RF, et al: Scheduled intermittent hospitalization for psychiatric patients. Psychiatric Services 49:504–509, 1998Link, Google Scholar
3. Eklund M, Hansson L: Relationship between characteristics of the ward atmosphere and treatment outcome in a psychiatric day-care unit based on occupational therapy. Acta Psychiatrica Scandinavica 95:329–335, 1997Crossref, Medline, Google Scholar
4. Timko C, Moos RH: Outcomes of the treatment climate in psychiatric and substance abuse programs. Journal of Clinical Psychology 54:1137–1150, 1998Crossref, Medline, Google Scholar
5. Timko C, Moos RH: Determinants of the treatment climate in psychiatric and substance abuse programs: implications for improving patient outcomes. Journal of Nervous and Mental Disease 186:96–103, 1998Crossref, Medline, Google Scholar
6. Smith J, Gross C, Roberts J: The evolution of a therapeutic environment for patients with long-term mental illness as measured by the Ward Atmosphere Scale. Journal of Mental Health 5:349–360, 1996Crossref, Google Scholar
7. Melle I, Friis S, Hauff E, et al: The importance of ward atmosphere in inpatient treatment of schizophrenia on short-term units. Psychiatric Services 47:721–726, 1996Link, Google Scholar
8. Middelboe T, Schjødt T, Byrsting K, et al: Ward atmosphere in acute psychiatric inpatient care: patients' perceptions, ideals, and satisfaction. Acta Psychiatrica Scandinavica 103:212–219, 2001Crossref, Medline, Google Scholar
9. Moos RH: Evaluating Treatment Environments: The Quality of Psychiatric and Substance Abuse Programs. New Brunswick, NJ, Transaction, 1997Google Scholar
10. Moos RH: Evaluating Treatment Environments: A Social Ecological Approach. New York, Wiley, 1974Google Scholar
11. Archer RP, Amuso KF: Comparison of staff's and patients' perceptions of the ward atmosphere. Psychological Reports 46:959–965, 1980Crossref, Medline, Google Scholar
12. Caplan CA: Nursing staff and patient perceptions of the ward atmosphere in a maximum security forensic hospital. Archives of Psychiatric Nursing 7:23–29, 1993Crossref, Medline, Google Scholar
13. Miller TW, Lee LI: Quality assurance: focus on environmental perceptions of psychiatric patients and nursing staff. Journal of Psychiatric Nursing and Mental Health Services 18:9–14, 1980Crossref, Google Scholar
14. Skodol AE, Plutchik R, Karasu TB: Expectations of hospital treatment: conflicting views of patients and staff. Journal of Nervous and Mental Disease 168:70–74, 1980Crossref, Medline, Google Scholar
15. Squier RW: The relationship between ward atmosphere and staff attitude to treatment in psychiatric in-patient units. British Journal of Medical Psychology 67:319–331, 1994Crossref, Medline, Google Scholar
16. Strasser DC, Falconer JA, Martino-Saltzmann D: The rehabilitation team: staff perceptions of the hospital environment, the interdisciplinary team environment, and interprofessional relations. Archives of Physical Medicine and Rehabilitation 75:177–182, 1994Medline, Google Scholar
17. Lanza ML, Kayne HL, Hicks C, et al: Environmental characteristics related to patient assault. Issues in Mental Health Nursing 15:319–335, 1994Crossref, Medline, Google Scholar
18. Lehman AF, Strauss JS, Ritzler BA, et al: First-admission psychiatric ward milieu: treatment process and outcome. Archives of General Psychiatry 39:1293–1298, 1982Crossref, Medline, Google Scholar
19. Herrera JM, Lawson WB: Effects of consultation on the ward atmosphere in a state psychiatric hospital. Psychological Reports 60:423–428, 1987Crossref, Medline, Google Scholar
20. Milne D: Planning and evaluating innovations in nursing practice by measuring the ward atmosphere. Journal of Advanced Nursing 11:203–210, 1986Crossref, Medline, Google Scholar
21. Jansson JA, Eklund M: Stability of perceived atmosphere over time, diagnosis, and gender for patients with psychosis. Nordic Journal of Psychiatry 56:407–412, 2003Google Scholar
22. Schjødt T, Middelboe T, Mortensen EL, et al: Ward atmosphere in acute psychiatric inpatient care: differences and similarities between patient and staff perceptions. Nordic Journal of Psychiatry 57:215–220, 2003Crossref, Medline, Google Scholar
23. Rossberg JI, Friis S: A suggested revision of the Ward Atmosphere Scale. Acta Psychiatrica Scandinavica 108:374–380, 2003Crossref, Medline, Google Scholar
24. Friis S: Measurements of the perceived ward milieu: a reevaluation of the Ward Atmosphere Scale. Acta Psychiatrica Scandinavica 73:589–599, 1986Crossref, Medline, Google Scholar
25. Shipley K, Hilborn B, Hansell A, et al: Patient satisfaction: a valid index of quality of care in psychiatric service. Acta Psychiatrica Scandinavica 101:330–333, 2000Crossref, Medline, Google Scholar
26. Fagin L, Carson J, Leary J, et al: Stress, coping, and burn out in mental health nurses: findings from three research studies. International Journal of Social Psychiatry 42:102–111, 1996Crossref, Medline, Google Scholar
27. Gulliver P, Towell D, Peck E: Staff morale in the merger of mental health and social care organizations in England. Journal of Psychiatric and Mental Health Nursing 10:101–107, 2003Crossref, Medline, Google Scholar
28. Jones JG, Janman K, Payne RL, et al: Some determinants of stress among psychiatric nurses. International Journal of Nursing Studies 24:129–144, 1987Crossref, Medline, Google Scholar
29. McCowan B: Self reported stress and its effects on nurses. Nursing Standard 42:33–38, 2001Google Scholar
30. Onyett S, Pillinger T, Muijen M: Job satisfaction and burnout among members of community mental health teams. Journal of Mental Health 6:65–66, 1997Google Scholar
31. Garmann AN, Corrigan PW, Morris S: Staff burnout and patient satisfaction: evidence of relationships at the care unit level. Journal of Occupational Health Psychology 7:235–241, 2002Crossref, Medline, Google Scholar
32. Corrigan PW, Lickey SE, Campion J, et al: Mental health team leadership and consumers' satisfaction and quality of life. Psychiatric Services 51:781–785, 2000Link, Google Scholar
33. Rossberg JI, Eiring Ø, Friis S: Work environment and job satisfaction: a psychometric evaluation of the Working Environment Scale-10. Social Psychiatry and Psychiatric Epidemiology, in pressGoogle Scholar
34. Rossberg JI, Friis S: Do the Spontaneity and Anger and Aggression subscales of the Ward Atmosphere Scale form homogeneous dimensions? A cross-sectional study of 54 wards for psychotic patients. Acta Psychiatrica Scandinavica 107:118–123, 2003Crossref, Medline, Google Scholar
35. Moos RH: Ward Atmosphere Scale Manual. Palo Alto, Calif, Consulting Psychologists Press, 1989Google Scholar
36. Helmstadter G: Principles of Psychological Measurement. New York, Appleton-Century-Crofts, 1964Google Scholar
37. Streiner DL, Normann GR: Health Measurement Scales: A Practical Guide to Their Development and Use. New York, Oxford University Press, 1989Google Scholar
38. Main S, McBride AB, Austin JK: Patient and staff perceptions of a psychiatric ward environment. Issues in Mental Health Nursing 12:149–157, 1991Crossref, Medline, Google Scholar
39. Friis S: Characteristics of a good ward atmosphere. Acta Psychiatrica Scandinavica 74:469–473, 1986Crossref, Medline, Google Scholar
40. Klass DB, Growe GA, Strizich M: Ward treatment milieu and posthospital functioning. Archives of General Psychiatry 34:1047–1052, 1977Crossref, Medline, Google Scholar
41. Moos RH, Schwartz J: Treatment environment and treatment outcome. Journal of Nervous and Mental Disease 154:264–275, 1972Crossref, Medline, Google Scholar
42. Friis S: The ward atmosphere: a crucial dimension of inpatients setting: measurements, clinical relevance, and some influencing factors: an empirical study. Academic dissertation, Oslo University, department of medicine, 1984Google Scholar
43. Perkins DO, Wyatt RJ, Bartko JJ: Pennywise and pound-foolish: the impact of measurement error on sample size requirements in clinical trials. Biological Psychiatry 47:762–766, 2000Crossref, Medline, Google Scholar



