Trends in Discharge Disposition, Mortality, and Service Use Among Long-Stay Psychiatric Patients in the 1990s
Abstract
OBJECTIVE: This study examined changes in discharge disposition, mortality, and service use among three cohorts of highly vulnerable long-stay psychiatric patients in the Department of Veterans Affairs (VA) mental health system during the 1990s, a period of extensive bed closures. METHODS: National VA administrative databases were used to identify and prospectively follow three long-stay cohorts: mental health inpatients who had been hospitalized for at least one year as of the end of fiscal year 1991 (N=2,343), 1994 (N=1,853), and 1997 (N=1,156). The cohorts were compared in baseline demographic and diagnostic characteristics as well as discharge disposition, mortality, and service use over a three-year follow-up period. RESULTS: Nationally, the number of occupied long-stay beds decreased by 50 percent between 1991 and 1997. Over time, significant changes were noted in long-stay patients' principal diagnoses and discharge dispositions. Compared with the 1991 cohort, the 1994 and 1997 cohorts had a higher proportion of patients with psychotic disorders (69 percent, 77 percent, and 75 percent, respectively) and were more likely to be discharged from the hospital during the three-year follow-up period (33 percent, 54 percent, and 53 percent, respectively). However, among patients who were discharged, no substantial differences were noted in either mortality or overall VA service use across the three cohorts. CONCLUSIONS: The delivery of inpatient VA mental health services changed dramatically during the 1990s. This study provided evidence that continuing efforts to close VA mental health beds have not resulted in substantially adverse changes in mortality rates or in the extent to which long-term inpatients remain connected with the VA system after discharge.
The delivery of mental health services changed substantially during the 1990s in the United States, largely through cost-driven reductions in inpatient care. In the private sector, for example, the use of inpatient services has declined by about a third in recent years (1,2,3,4). Major transformations have also occurred in the public sector (5,6) and are well documented for the Department of Veterans Affairs (VA) mental health care system (7). Between fiscal years 1994 and 1997, the VA eliminated 5,987 mental health beds nationally, nearly 45 percent of the 1994 total of 13,571 beds (8).
Despite increasing pressures to reduce inpatient services and bed capacity, studies that have evaluated the consequences of recent changes in the mental health system are limited. Studies of the impact of Medicaid managed care on clinical outcomes have been initiated (9); some of these reported worse outcomes (10), but others did not (11,12). However, none of these studies focused on the effects of large-scale bed closures. Several studies of the impact of bed closures and other efforts to curtail mental health inpatient costs in the VA system have recently been published and have shown little or no association with outcomes such as cross-system use of psychiatric services (13,14), rates of incarceration (15), and reduced treatment effectiveness for posttraumatic stress disorder (16). Although the studies have focused on veterans with severe mental illness, many of whom require brief, episodic inpatient care, they have not specifically examined the effects of bed closures on the most vulnerable inpatients—those who have been hospitalized for an extended period, such as a year or more.
Recent studies of non-VA state hospital downsizings and closings have focused to a greater extent on long-stay populations and have reported improvements in level of functioning and quality of life (17,18) but not full community integration (19) after discharge. Although these studies provide important evidence that even persons hospitalized for prolonged periods can do well after discharge, they are somewhat limited in that they typically reflect the closing of a single facility rather than more systemwide changes. In addition, studies of the process of deinstitutionalizing state psychiatric patients have often focused on the results of legal mandates or consent decrees through which funds have been specifically set aside to enhance community-based services and to monitor outcomes (20,21,22). Moreover, these case studies, which have evaluated a particular state's efforts to reduce inpatient care, have not shed light on the potential impact that more naturalistic, ongoing changes in a mental health system might have on different cohorts of long-stay patients over time.
In the study reported here, we used national VA administrative data to identify and prospectively follow up three cohorts of long-stay inpatients, defined as those who had been hospitalized for at least a year. Spanning a period of accelerated change in the VA mental health system, the data for the three cohorts were drawn from the early, middle, and late 1990s, respectively. We were interested in determining whether the proportion of long-stay patients being discharged from inpatient units increased over time and whether there were any changes in discharge destination among the patients who were discharged. In addition, we sought to determine whether there were substantial changes in three-year mortality rates across cohorts and in the extent to which discharged patients continued to have contact with the VA system after discharge.
Methods
Subjects and procedures
An annual census is conducted of all current VA inpatients at the end of every fiscal year (September 30). For each inpatient, an administrative record is generated that includes data on factors such as demographic characteristics (for example, age, sex, and race), date of admission, bed section, and principal diagnosis. We used census files from fiscal years 1991, 1994, and 1997 to identify and describe three cohorts of long-stay patients, defined as inpatients occupying psychiatric or substance abuse beds who had a length of stay of at least one year at the end of the fiscal year. The years 1991 and 1994 were selected because they correspond to periods before and at the start of, respectively, accelerated bed closures in the VA system; 1997 was chosen because the process of closing beds was well under way at that time (8).
For patients in each cohort, we determined the discharge disposition and vital status over a three-year follow-up period, ending on September 30 of 1994, 1997, and 2000 for the three cohorts, respectively. Discharge disposition was determined by using census files from subsequent years as well as the VA Patient Treatment File, a national discharge abstract database that documents all discharges from VA inpatient facilities. We categorized patients' discharge disposition as one of the following: discharged to the community, discharged to a VA nursing home, discharged to a community nursing home, other placement (for example, a halfway house or a boarding house), died in the hospital, or continued as an inpatient. Because many long-stay patients were discharged from the hospital only to be readmitted shortly thereafter, we considered readmissions that occurred within 30 days to be continuations of the index inpatient stay. Thus, for the purposes of this study, long-stay patients had to be out of a VA hospital for more than 30 days in order to be considered successfully discharged.
In addition to documenting trends in discharge disposition, we examined differences in overall mortality among the three cohorts. For each cohort, we calculated the three-year mortality rate for all patients as well as the specific mortality rate for those who were discharged alive. Data on inhospital deaths obtained from the Patient Treatment File were supplemented with mortality data from the VA's Beneficiary Identification and Records Locator Subsystem (BIRLS), a computerized database of deceased veterans who have received VA death benefits. In terms of completeness of mortality ascertainment in the veteran population, the BIRLS has been shown to be comparable to alternatives such as the National Death Index (23) and records of the Social Security Administration (24).
Finally, to gauge the extent to which patients who were discharged to different settings in the three cohorts remained connected with VA health services, we used administrative workload data to determine use of services during the third year after baseline (fiscal year 1994, 1997, and 2000, respectively, for the three cohorts). Specifically, we determined whether discharged patients who survived the follow-up period received any inpatient or outpatient psychiatric or substance abuse services, community-based mental health services (for example, VA community residential care and intensive case management), inpatient or outpatient medical or surgical services, nursing home services, or any of these VA health services.
Among patients who made at least one outpatient visit, we also determined the mean number of visits in order to gauge the intensity of service use. Service use data were obtained from computerized national workload files, including the Patient Treatment File, the Outpatient Care File, and the Extended Care File, which, taken together, document all episodes of VA care.
This study was approved by the institutional review board of the VA Connecticut Healthcare System.
Data analysis
Differences in baseline characteristics, discharge disposition, mortality rates, and service use across the three cohorts were compared by using analysis of variance F tests for continuous variables and chi square tests for categorical variables. All analyses were performed with SAS version 6.12 (25).
Results
Description of the cohorts
As expected, given the trend in VA bed closures, we identified a decreasing number of long-stay inpatients between 1991 (N=2,359), 1994 (N=1,863), and 1997 (N=1,178). Information on discharge disposition was missing for less than 2 percent of each cohort; thus the baseline sample sizes were 2,343, 1,853, and 1,156, respectively. All the patients were occupying psychiatric beds as opposed to substance abuse beds. The three groups were not fully mutually exclusive. The study included 3,794 unique patients, approximately a third (N=1,211) of whom belonged to more than one cohort; 9 percent (N=347) were in all three cohorts.
The characteristics of the three groups are summarized in Table 1. Compared with those in the 1991 and 1994 cohorts, members of the 1997 cohort had a shorter mean length of stay and were, on average, approximately three years older at baseline. The three groups did not differ significantly in sex or race. However, the cohorts did differ in principal diagnoses. The proportion of patients with a principal diagnosis of schizophrenia or another psychotic disorder increased from 69.4 percent in the 1991 cohort to 77.0 percent in the 1994 cohort and held fairly steady at 75.3 percent in the 1997 cohort. The proportion of patients who had disorders categorized as "other" decreased by a corresponding amount during the same period.
Discharge disposition and mortality
As mentioned above, many long-stay patients were initially discharged only to be readmitted shortly thereafter. Of the patients in the 1991 cohort, 155 (6.6 percent) were discharged and then readmitted within 30 days, compared with 170 (9.2 percent) in the 1994 cohort and 108 (9.3 percent) in the 1997 cohort (χ2=12.22, df=2, p=.002). As can be seen from Table 2, considerable changes in discharge disposition were observed between the 1991 and 1994 cohorts. Compared with the 1991 cohort, a smaller proportion of patients in the 1994 cohort remained in the hospital (36 percent compared with 49 percent) or died in the hospital (10 percent compared with 18 percent) during the three-year follow-up period. By contrast, a larger proportion of these patients were discharged to the community (28 percent compared with 17 percent) or to a nursing home (23 percent compared with 13 percent).
In terms of the proportion of patients who remained in the hospital, died in the hospital, or were discharged, the overall pattern of discharge disposition was nearly identical for the 1994 and 1997 cohorts. One noteworthy difference between the two cohorts was the apparent shift away from placement in community nursing homes to VA nursing home placements. That is, although the total percentage of patients who were discharged to a nursing home remained similar for the period 1994 to 1997 (23 percent) and the period 1997 to 2000 (22 percent), the relative proportion admitted to VA versus community nursing homes increased substantially. In the 1994 cohort, long-stay patients were discharged to VA and community nursing homes in roughly equal numbers, whereas VA nursing home placements outnumbered community nursing home placements by more than two to one in the 1997 cohort.
Table 2 also lists the three-year mortality rates for the three cohorts. Overall mortality was higher in the 1991 cohort (22 percent) than in the 1994 and the 1997 cohorts (17 percent and 19 percent, respectively), primarily because of the 1991 cohort's higher inhospital mortality rate. However, among the patients who were discharged, no significant difference in mortality over the follow-up period was observed across cohorts.
Use of VA health services
Table 3 presents the proportion of surviving discharged patients who used a variety of VA health services during the third year after baseline. Overall, any contact with the VA health care system remained high throughout the study period. Eighty-eight percent of discharged patients in the 1991 cohort, 87 percent in the 1994 cohort, and 83 percent in the 1997 cohort continued to receive some form of VA care during the third year after baseline.
As can be seen from Table 3, subsequent use of services varied considerably by discharge destination and cohort. Across the three cohorts, patients who were discharged to community nursing homes were consistently least likely to remain connected with any VA health services. Although this finding is based on a relatively small sample (N=60), it was especially true of patients in the 1997 cohort: only a third of patients in this cohort who were discharged to community nursing homes used any VA services in fiscal year 2000, down from about 70 percent in the 1991 and 1994 cohorts. This dramatic decline in service use among these patients was consistent across all health service categories considered.
Table 3 also shows that follow-up contact with a range of mental health services was greatest among long-stay patients who were discharged to the community or to alternative settings, such as halfway houses and boarding houses, whereas the proportion of patients who used psychiatric or substance abuse services was generally lower among those who were discharged to VA nursing homes. However, these data did not capture the use of services provided directly in VA nursing homes by consulting psychiatrists. Follow-up use of any medical or surgical services was greatest among patients who were discharged to VA nursing homes—probably reflecting the elevated medical morbidity in this group of patients—although, in general, the use of these services declined slightly over time.
The proportions of patients who received any VA outpatient care during the third year after baseline are shown in Table 4, along with the mean number of visits among those who had at least one mental health or medical or surgical outpatient contact. Overall, approximately half of the surviving discharged patients from each cohort received at least some outpatient care (53 percent, 55 percent, and 47 percent, respectively). Across the three cohorts, the highest proportions appeared to be among those who were discharged to the community or to alternative settings, whereas the lowest rates were found among those who were discharged to either a VA or a community nursing home. Among patients who made at least one outpatient visit, the intensity of service use was low: an average of little more than one visit during the third year after baseline.
Discussion
During the mid-1990s, the Veterans Health Administration was restructured into a more decentralized system of 22 semiautonomous Veterans Integrated Service Networks serving geographically defined populations (26). As part of the restructuring process, administrative directives and financial incentives were used to transform the VA health care system from one focused on acute inpatient care and medical specialization to one grounded in outpatient and primary care.
Between fiscal years 1995 and 2000, the number of veterans receiving inpatient mental health care decreased by 38.5 percent (from 123,217 to 75,745), whereas the number receiving outpatient mental health care increased by 23.2 percent (from 545,004 to 671,368); this change in mental health service delivery was associated with a 24.9 percent reduction in per patient cost (from $3,560 to $2,673) (8). It was within this context of rapid and substantial service system changes that we sought to examine recent trends in discharge disposition, mortality, and service use among VA long-stay psychiatric patients—an especially vulnerable subgroup of mental health service users.
We found that, nationally, the number of occupied long-stay beds decreased by 50 percent between the end of fiscal year 1991 and 1997. Over time, there were significant changes in the principal diagnoses and discharge dispositions of long-stay patients. However, among patients who were discharged, no substantial differences were noted in either mortality rates or overall use of VA services across the three cohorts.
Compared with the 1991 cohort, the 1994 and 1997 cohorts included a significantly higher proportion of patients with a primary diagnosis of schizophrenia or another psychotic disorder. To some extent, this shift may reflect the greater likelihood of discharge among inpatients who have less severe psychiatric disorders and retention of those with behavioral problems and tendencies that would complicate subsequent placement (27). Fisher and colleagues (28) found that 69 percent of long-stay patients in Massachusetts state hospitals had exhibited a significant problematic behavior—for example, committed physical assault or had violent episodes—in the previous 30 days.
Between the 1991 and the 1994 cohorts, there was also a significant shift in readmission and discharge disposition. Discharge was attempted but unsuccessful (readmission within 30 days) for a greater proportion of patients in the 1994 cohort than in the 1991 cohort. Nevertheless, more than half of the patients in the 1994 cohort were discharged from the hospital for more than 30 days by the end of the three-year follow-up period, compared with a third of the patients in the 1991 cohort.
With the accelerated pace of VA bed closures well under way, the pattern of readmission and discharge disposition was nearly identical in the 1994 and 1997 cohorts. An exception was an apparent shift away from placement in community nursing homes in favor of VA nursing homes. It is not clear from these data what motivated this change. However, it is possible that a serial discharge process is in effect, such that patients are first discharged to a VA nursing home for a relatively short stay and then transferred to a community facility.
A notable finding of this study was that, among patients who were discharged, no significant change was noted in mortality rates during the three-year follow-up period across the three cohorts. This finding is consistent with those of studies that showed little or no adverse impact of VA bed closures on other outcomes, including rates of incarceration (15) and cross-system use of state psychiatric services (13,14). As these earlier studies have indicated, many VA facilities coupled inpatient bed closures with increased expenditures on outpatient and community care. The expansion of outpatient capacity in conjunction with inpatient downsizing may reduce the risk of adverse outcomes.
Among surviving patients who were discharged, the overall use of any VA health services in the third year after baseline was high in all three cohorts—more than 80 percent—suggesting that a majority of patients remained at least somewhat connected with the VA system. The patients who were discharged to community nursing homes were the least likely to receive any follow-up care. Data on the use of non-VA services were not available, so we do not know the extent to which these and other patients may have substituted services in other health care settings for VA care. This limitation of the data is particularly striking given the low intensity of use of VA outpatient services in the three cohorts.
It is also unclear why the use of VA services declined so dramatically among patients who were discharged to community nursing homes in the 1997 cohort compared with those in the other two cohorts. Although it is possible that this finding reflects an idiosyncrasy of the small sample, future studies should seek to examine the reasons for and potential implications of this decline in connectedness with VA services.
Several limitations of this study deserve comment. First, as is often the case in record-linkage studies of this kind, the database merges were based on a single personal identifier—Social Security number—and some matches may have been missed because of miscoding. Second, the validity of the administrative data we used is unknown. However, the general validity of VA administrative data has previously been demonstrated (29). Third, mortality and service use are somewhat blunt measures of patient outcome. Information was not available on outcomes such as clinical status, quality of life, and functioning after discharge. Such data are costly to collect and are rarely gathered before the implementation of major service system changes, thereby making follow-up comparisons difficult to perform. However, in case studies in which these kinds of data have been collected, the results have been encouraging in terms of demonstrating improvements in level of functioning and quality of life (17,18).
Fourth, data were not available on comorbid medical conditions, which potentially limits the interpretation of mortality estimates. Finally, because some patients belonged to more than one cohort, the three groups were not entirely independent. Thus computed chi square and F statistics were overestimated, and, accordingly, p values were underestimated. Nevertheless, even if one were to use a more conservative alpha level to test significance—for example, p<.01—similar conclusions would be drawn.
Conclusions
Between 1991 and 1997, the VA reduced its psychiatric long-stay population by 50 percent. Using available secondary administrative data sources, this study provided evidence that continuing efforts to close VA mental health beds and limit inpatient services have not resulted in substantially adverse changes in mortality rates or in the extent to which patients remain connected with the VA health care system after discharge.
Dr. Desai is an epidemiologist and mental health services researcher at the Department of Veterans Affairs Mental Illness Research, Education, and Clinical Center (MIRECC) and Northeast Program Evaluation Center (NEPEC) in West Haven, Connecticut. Dr. Rosenheck is codirector of the MIRECC and director of the NEPEC. Both authors are also affiliated with the department of psychiatry at Yale University School of Medicine in New Haven, Connecticut. Send correspondence to Dr. Desai at the VA Connecticut Healthcare System, NEPEC (182), 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]).
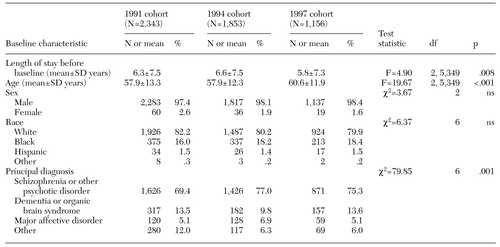 |
Table 1. Baseline characteristics of the 1991, 1994, and 1997 cohorts of long-stay psychiatric patients in the Department of Veterans Affairs mental health care system
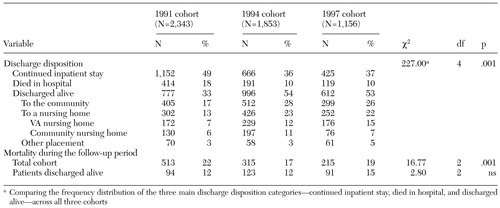 |
Table 2. Discharge disposition and mortality during a three-year follow-up period for the 1991, 1994, and 1997 cohorts of long-stay psychiatric patients in the Department of Veterans Affairs (VA) health care system
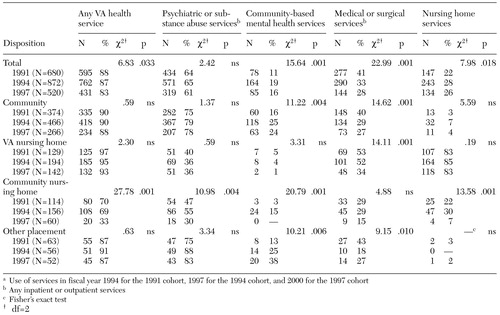 |
Table 3. Proportion of discharged patients who used a variety of Department of Veterans Affairs (VA) health services during the third year after baselinea among those who survived the three-year follow-up period, by discharge disposition and cohort
a Use of services in fiscal year 1994 for the 1991 cohort, 1997 for the 1994 cohort, and 2000 for the 1997 cohort
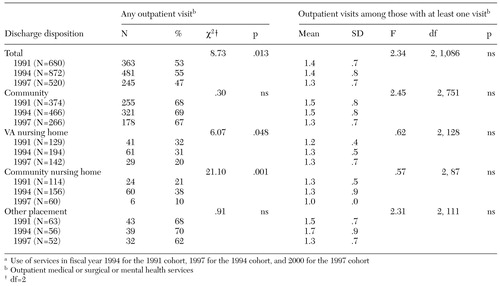 |
Table 4. Use of Department of Veterans Affairs (VA) outpatient services in the third year after baselinea among discharged patients who survived the three-year follow-up period, by discharge disposition and cohort
a Use of services in fiscal year 1994 for the 1991 cohort, 1997 for the 1994 cohort, and 2000 for the 1997 cohort
1. Ma CA, McGuire TG: Costs and incentives in a behavioral health carve-out. Health Affairs 17(2):53-69, 1998Google Scholar
2. Goldman W, McCulloch J, Sturm R: Costs and use of mental health services before and after managed care. Health Affairs 17 (2):40-52, 1998Google Scholar
3. Rosenheck RA, Druss B, Stolar M, et al: Effect of declining mental health service use on employees of a large corporation. Health Affairs 18(5):193-203, 1999Google Scholar
4. Leslie DL, Rosenheck R: Shifting to outpatient care? Mental health care use and cost under private insurance. American Journal of Psychiatry 156:1250-1257, 1999Abstract, Google Scholar
5. Geller JL: The last half-century of psychiatric services as reflected in Psychiatric Services. Psychiatric Services 51:41-67, 2000Link, Google Scholar
6. Closing and Reorganizing State Psychiatric Hospitals:1996: State Mental Health Agency Profile System Highlights. Alexandria, Va, National Association of State Mental Health Program Directors Research Institute, 1997Google Scholar
7. Rosenheck R, Horvath T: The impact of VA reorganization on patterns of mental health care. Psychiatric Services 49:53, 1998Link, Google Scholar
8. Rosenheck R, Greenberg G, DiLella D: Department of Veterans Affairs National Mental Health Program Performance Monitoring System: Fiscal Year 2000 Report. West Haven, Conn, Northeast Program Evaluation Center, 2001Google Scholar
9. Mechanic D, Schlesinger M, McAlpine DD: Management of mental health and substance abuse services: state of the art and early results. Milbank Quarterly 73:19-55, 1995Crossref, Medline, Google Scholar
10. Popkin MK, Lurie N, Manning W, et al: Changes in the process of care for Medicaid patients with schizophrenia in Utah's Prepaid Mental Health Plan. Psychiatric Services 49:518-523, 1998Link, Google Scholar
11. Dickey B, Norton E, Norman SL, et al: Managed mental health experience in Massachusetts. New Directions for Mental Health Services 78:115-122, 1998Medline, Google Scholar
12. Hausman JW, Wallace N, Bloom JR: Managed mental health experience in Colorado. New Directions in Mental Health Services 78:107-114, 1998Medline, Google Scholar
13. Rosenheck R, Frisman L, Essock S: Impact of VA bed closures on use of state psychiatric services. Journal of Behavioral Health Services and Research 28:58-66, 2001Crossref, Medline, Google Scholar
14. Rosenheck R, Banks S, Pandiani J: Does closing inpatient beds in one public mental health system result in increased use of hospital services in other systems? Mental Health Services Research 2:183-189, 2000Google Scholar
15. Rosenheck RA, Banks S, Pandiani J, et al: Bed closures and incarceration rates among users of Veterans Affairs mental health services. Psychiatric Services 51:1282-1287, 2000Link, Google Scholar
16. Rosenheck R, Fontana A: Impact of efforts to reduce inpatient costs on clinical effectiveness: treatment of posttraumatic stress disorder in the Department of Veterans Affairs. Medical Care 39:168-180, 2001Crossref, Medline, Google Scholar
17. McGrew JH, Wright ER, Pescosolido BA, et al: The closing of Central State Hospital: long-term outcomes for persons with severe mental illness. Journal of Behavioral Health Services and Research 26:246-261, 1999Crossref, Medline, Google Scholar
18. Okin RL, Borus JF, Baer L, et al: Long-term outcome of state hospital patients discharged into structured community residential settings. Psychiatric Services 46:73-78, 1995Link, Google Scholar
19. Dewees M, Pulice RT, McCormick LL: Community integration of former state hospital patients: outcomes of a policy shift in Vermont. Psychiatric Services 47:1088-1092, 1996Link, Google Scholar
20. Geller JL, Fisher WH, Simon LJ, et al: Second-generation deinstitutionalization: II. the impact of Brewster v Dukakis on correlates of community and hospital utilization. American Journal of Psychiatry 147:988-993, 1990Link, Google Scholar
21. McGrew JH, Wright ER, Pescosolido BA: Closing of a state hospital: an overview and framework for a case study. Journal of Behavioral Health Services and Research 26:236-245, 1999Crossref, Medline, Google Scholar
22. Rothbard AB, Richman E, Hadley TR: "Unbundling" of state hospital services in the community: the Philadelphia State Hospital story. Administration and Policy in Mental Health 24:391-398, 1997Crossref, Medline, Google Scholar
23. Fisher SG, Weber L, Goldberg J, et al: Mortality ascertainment in the veteran population: alternatives to the National Death Index. American Journal of Epidemiology 141:242-250, 1995Crossref, Medline, Google Scholar
24. Page WF, Braun MM, Caporaso NE: Ascertainment of mortality in the US veteran population: World War II veteran twins. Military Medicine 160:351-355, 1995Crossref, Medline, Google Scholar
25. SAS Institute: The SAS System for Windows, Release 6.12. Cary, NC, SAS Institute, 1996Google Scholar
26. Kizer KW, Fonseca ML, Long LM: The veterans healthcare system: preparing for the twenty-first century. Hospital and Health Services Administration 42:283-298, 1997Medline, Google Scholar
27. Holloway F, Wykes T, Petch E, et al: The new long stay in an inner city service: a tale of two cohorts. International Journal of Social Psychiatry 45:93-103, 1999Crossref, Medline, Google Scholar
28. Fisher WH, Barreira PJ, Geller JL, et al: Long-stay patients in state psychiatric hospitals at the end of the 20th century. Psychiatric Services 52:1051-1056, 2001Link, Google Scholar
29. Kashner TM: Agreement between administrative files and written medical records: a case of the Department of Veterans Affairs. Medical Care 36:1324-1336, 1998Crossref, Medline, Google Scholar



