Datapoints: The Impact of VA Reorganization on Patterns of Mental Health Care
In October 1995 the Veterans Health Administration of the Department of Veterans Affairs (VA) was restructured into 22 Veterans Integrated Service Networks serving geographically defined populations. The goal of this decentralization was to transform the VA health care system from one focused on acute inpatient care and medical specialization to one grounded in ambulatory and primary care (1).
Table 1 presents national VA workload data on unduplicated counts of patients treated in specialized inpatient and outpatient psychiatric and substance abuse programs in fiscal years 1993 through 1997, before and after the reorganization.
The number of inpatients treated annually in both psychiatric and substance abuse programs declined by less than 1 percent in the three fiscal years preceding the reorganization (1993 through 1995) but fell by 19 percent in the second year after the reorganization. However, the number of inpatients receiving substance abuse services fell by almost 50 percent, far exceeding the 7 percent drop for psychiatric inpatient services. In contrast, the number of outpatients receiving psychiatric and substance abuse services increased steadily both before and after the reorganization.
Changes in the intensity of care, measured by the average length of inpatient stay per episode and the average annual number of outpatient contacts per user, paralleled trends in inpatient and outpatient service use. The biggest changes occurred in substance abuse services, with decreases in the length of inpatient stays and increases in the number of user contacts.
The number of patients who received any specialty mental health treatment, either inpatient or outpatient, increased by about 8 percent in the two years following the reorganization. However, 4,538 fewer veterans (about 3 percent) received substance abuse treatment in fiscal year 1997 than in 1995, the year before the reorganization.
Dr. Rosenheck is director of the Northeast Program Evaluation Center of the Veterans Affairs Connecticut Healthcare System in West Haven and clinical professor of psychiatry at Yale University in New Haven, Connecticut. Dr. Horvath is chief consultant for mental health at VA headquarters in Washington, D.C., and professor of psychiatry at the State University of New York at Stony Brook. Address correspondence to Dr. Rosenheck, Northeast Program Evaluation Center (182), VA Medical Center, 950 Campbell Avenue, West Haven, Connecticut 06516. With this issue Harold Alan Pincus, M.D., and Terri L. Tanelian, M.A., become coeditors of this column.
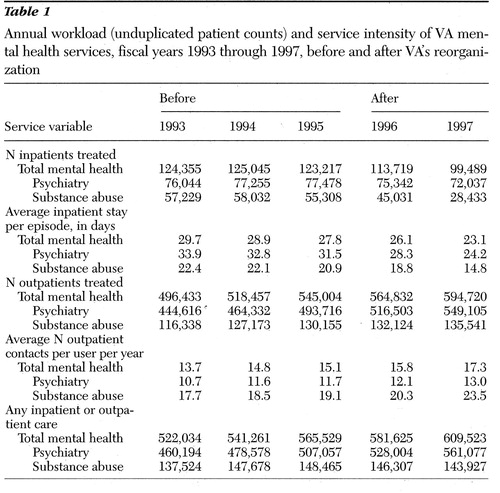 |
Table 1. Annual workload (unduplicated patient counts) and service intensity of VA mental health services, fiscal years 1993 through 1997, before and after VA's reorganization
1. Kizer KW, Fonseca ML, Long LL: The veterans healthcare system: preparing for the twenty-first century. Hospital and Health Administration 42:283-298, 1997Google Scholar



