Ethnic Matching of Clients and Clinicians and Use of Mental Health Services by Ethnic Minority Clients
Abstract
OBJECTIVES: Research in the United States has indicated that matching clients from a minority group with clinicians from the same ethnic background increases use of community mental health services and reduces use of emergency services. This study assessed the effects of matching clients from a non-English-speaking background with bilingual, bicultural clinicians in a mental health system in Australia that emphasizes community-based psychiatric case management. METHODS: In an overall sample of 2,935 clients served in the western region of Melbourne from 1997 to 1999, ethnic minority clients from a non-English-speaking background who received services from a bilingual, bicultural case manager were compared with ethnic minority clients who did not receive such services and with clients from an English-speaking background. The clients' engagement with three types of services—community care teams, psychiatric crisis teams, and psychiatric inpatient services—was assessed. RESULTS: Compared with ethnic minority clients who were not matched with a bilingual clinician, those who were matched generally had a longer duration and greater frequency of contact with community care teams and a shorter duration and lower frequency of contact with crisis teams. Clients born in Vietnam who were matched with a bilingual clinician had a shorter annual mean length of hospital stay and a lower annual mean frequency of hospital admission than Australian-born clients. CONCLUSIONS: The benefits of matching clients with psychiatric case managers on the basis of ethnic background include a lower level of need for crisis intervention and, for clients from some ethnic groups, fewer inpatient interventions. These Australian results support findings of the effectiveness of client-clinician ethnic matching in the United States.
In Western nations, ethnic minority groups have experienced difficulties in gaining access to mental health care (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15). Relative to the majority population, members of ethnic minority groups are underrepresented among patients receiving mental health services (1,2,3,4,5) and tend to underutilize mental health services (5,6,7,8,9,10,11,12,13,14,15).
Underutilization and underrepresentation have been attributed to barriers to initial access to mental health services (1,2,5) and to early dropout (16), which have been attributed to a wide variety of factors. These factors include insufficient knowledge of the mental health care system in the ethnic community, clinicians' failure to recognize mental illness among ethnic minority clients, ethnic minority groups' association of substantial stigma with disclosure of emotional or psychiatric problems, substantial delays or use of alternative forms of managing mental health problems before seeking psychiatric care, and initial perceptions and experiences suggesting that the mental health system does not provide acceptable or appropriate care for members of ethnic minority groups.
Definitions of "ethnic minorities" vary across countries and across studies (4). In Australia, researchers commonly distinguish between persons born in a country where English is not the main language (persons with a non-English-speaking background) and those born in countries where English is the main language (persons with an English-speaking background). Groups with a non-English-speaking background in Australia have been reported to underutilize mental health services relative to groups with an English-speaking background (1,2,3). Two major state surveys, in New South Wales (1) and Victoria (2), indicated that persons with a non-English-speaking background are underrepresented among clients of psychiatric services compared with persons born in Australia. Clients with a non-English-speaking background had significantly fewer contacts with community services than Australian-born clients (1,2,17). Although to our knowledge no Australian research has examined the use of psychiatric emergency or crisis services among persons with a non-English-speaking background, research in the United States has suggested that ethnic minority groups may use such services more frequently than the majority group (19,20).
In addition, some studies have examined the duration of hospital stay among patients from ethnic minority groups. Brief hospitalization may reflect timely admission and treatment early in an episode of psychosis, which may be related to adequate community-based monitoring by case managers. In the Australian research, no study has found briefer hospital stays among groups with a non-English-speaking background, relative to the Australian-born group, and several studies have found equal (1,5,18,21) or longer (2,17,22) stays among patients from a non-English-speaking background.
Several studies have reported a higher proportion of involuntary admissions among patients from a non-English-speaking background than among their counterparts from an English-speaking background (1,2,3,5,21). The higher proportion of involuntary admissions might reflect the reluctance of persons from a non-English-speaking background to use mental health services, for the reasons outlined above, but it may also be due to clinicians' difficulty or bias in conducting cross-cultural assessments.
Matching clients from a non-English-speaking background with bilingual, bicultural mental health clinicians is one of the most commonly suggested strategies for improving access to and use of mental health services by ethnic minorities (16,23,24,25,26,27,28,29,30). However, to our knowledge, no research on the effectiveness of this strategy has been conducted in Australia, even though research in the United States has suggested that client-clinician ethnic matching reduces clients' rates of premature termination of therapy (16,24,25,26), increases their contact with clinical services (16,25,27,28,29), reduces their contact with emergency or crisis services (28,30), and reduces the number of days they spend in the hospital (28). Ethnic matching may also improve the effectiveness of therapeutic processes such as counseling (31).
The study reported here focuses on the effects on clients' service use of the introduction of a bilingual, bicultural case management program in a psychiatric service system in western Melbourne, Australia. This region, which covers approximately one-third of the total area of Melbourne, is the most densely populated area in Melbourne with respect to immigrants. Approximately 33 percent of the adult population in this area was born in a non-English-speaking country (N=216,949), and 37 percent (N=238,036) live in a household where a language other than English is spoken (2). Beginning in the middle of 1996, the psychiatric service system in western Melbourne employed 11 bilingual, bicultural staff members in case management positions within continuing care teams, which provide assessment, medical care, medication management, and case management. The bilingual case managers were employed at four area mental health services with catchment area populations ranging between 100,000 and 150,000. The languages spoken by these staff members were selected on the basis of perceived need in the catchment areas and included Italian, Greek, Vietnamese, Macedonian, Croatian, and Turkish.
The roles of the bilingual case managers included direct case management, secondary consultation, peer training, community education and support, and education of family members and other caregivers. These case managers saw a mix of clients from both non-English-speaking and English-speaking backgrounds. The bilingual clinicians were able to converse with clients from a non-English speaking background in their preferred language, whereas other clinicians relied on interpreters to converse with similar clients. The bilingual staff members felt they had a better understanding of their ethnic clients' culture and immigration experience, which helped them establish better rapport, provide more accurate assessments and culturally consonant explanations of mental illness and treatment, and communicate more easily with clients' family members.
The purpose of this study was to examine the effects of client-clinician ethnic matching on mental health service use by clients from a non-English-speaking background. Specifically, we hypothesized that clients from a non-English-speaking background who received services from a bilingual, bicultural case manager from the same background would have more contact with community care teams, less contact with emergency crisis assessment and treatment teams, a shorter inpatient hospital stay, and a lower incidence of involuntary admission compared with similar clients who did not receive services from a bilingual, bicultural case manager.
Methods
The study had a quasi-experimental design and used administrative data that were routinely collected by the area mental health services. Service use data for ethnic minority clients who were matched with a bilingual case manager were compared with service use data for ethnic minority clients who were not so matched and with clients who were not members of ethnic minority groups.
Sample
The sample consisted of 2,935 people who had contact with the mental health service system for one week or more over the two-year evaluation period from 1997 to 1999. Seventy-five percent of the overall group (N=2,201) had a diagnosis of a psychotic disorder, including bipolar affective disorder. Fifty-three percent (N=1,614) were male, and 26 percent (N=763) were born in a non-English-speaking country.
The data were obtained from the Psychiatric Records Information Systems Manager (PRISM) database, the official psychiatric case register in Victoria, for the 1997-1998 and 1998-1999 annual periods. Information on contacts with continuing care teams, contacts with crisis assessment and treatment teams, and hospital admissions was collected. Demographic data for the clients were obtained from the same database. Approval of the ethics committee of the University of Melbourne was obtained.
Measures
The main measures in the study were the frequency and duration of clients' face-to-face (direct) and telephone contact with continuing care teams; the frequency and duration of clients' face-to-face and telephone contact with crisis assessment and treatment teams; and the frequency, duration, and legal status of clients' hospital admissions. The measures were calculated as rates per year, because clients had spent different periods in contact with mental health services. To explore the effect of clients' being treated by a bilingual case manager, the proportion of clients' contacts with a bilingual case manager relative to all contacts with a case manager was used as the independent variable in the analyses.
Statistical analysis
Most of the variables were positively skewed. Equations for normalizing the data were developed by using STATA (32). The frequency of direct contact was normalized with the following equation: natural logarithm × ([frequency of direct contact + 1] - .9811728). All other variables were transformed by using the natural logarithm function. The Kolmogorov-Smirnov test was used to check that the transformed variables did not significantly depart from normality (33). The median frequency and duration of contact and the length of stay and number of hospital admissions were calculated from untransformed data that were trimmed of the top 5 percent of cases.
The main aim of the analysis was to examine the effect of client-clinician ethnic matching on service use by ethnic minority clients. The client was the unit of analysis. Simultaneous multiple regression analysis (34) was used to examine the relationship of the clients' country of birth, age, sex, diagnosis, and contact with a bilingual case manager with the service use variables described above. Regression analyses examining the duration and frequency of contact with crisis assessment and treatment teams and those examining the use of inpatient services included the duration and frequency of contacts with continuing care teams as predictors to control for possible differences in outcomes due to differences in inputs—for example, bilingual case managers may have spent more time than the other case managers with their ethnic minority clients.
In addition, because the bilingual case managers tended to be younger and less experienced than the other case managers in the study, services received from the bilingual case managers may have had effects for all clients that could have confounded the results. To control for these possible confounding effects, we added an interaction variable to the regression analyses to measure exposure to bilingual case managers of clients with and without an English-speaking background. The interaction variable was created by recoding country of birth as -1 for clients with an English-speaking background and 1 for clients with a non-English-speaking background and multiplying this value by the proportion of contacts a client had with a bilingual case manager. Higher positive values for this variable indicated a greater amount of contact between clients with a non-English-speaking background and a case manager of the same ethnic background, and higher negative values indicated a greater amount of contact between clients with an English-speaking background and a bilingual case manager with any background. A score of zero meant that the client received case management services from a case manager who was not bilingual.
Additional analyses clarifying the direction of trends were conducted by recoding the proportion of contacts with a bilingual case manager as a dichotomous variable differentiating no involvement with a bilingual case manager from any involvement with a bilingual case manager.
Results
The results for clients' contact with continuing care teams are summarized in Table 1. Younger clients, female clients, and clients with a nonpsychotic diagnosis had more frequent telephone and face-to-face contacts and a longer duration of both types of contact. Both clients from a non-English-speaking background and those from an English-speaking background who had more contact with a bilingual case manager also had more frequent contact and a longer duration of total contact with continuing care teams. Clients with an English-speaking background had more frequent telephone contacts than clients with a non-English-speaking background, but no significant differences between those groups were found in the frequency of direct contact or in the duration of either type of contact.
Clients with a non-English-speaking background who were matched with a bilingual case manager had more frequent direct contacts and a greater total duration of direct contacts than clients from a non-English-speaking background or clients from an English-speaking background who were not matched with a bilingual case manager, but no effect of ethnic matching on telephone contacts was found. By using Cohen's criteria (35), the size of all of these effects could be described as small (beta values of around .1 or less).
Table 2 shows the results for clients' contacts with crisis assessment and treatment teams. Clients who had a diagnosis of a disorder other than psychosis had more frequent telephone and direct contacts with crisis teams and a longer total duration of such contacts, compared with clients with a diagnosis of a psychosis. Clients who had more frequent telephone contact with their case manager in the continuing care team also had more contact with the crisis teams. Younger clients tended to have more telephone contact with the crisis teams than older clients, but this difference did not hold for face-to-face contacts.
Clients from a non-English-speaking background matched with a bilingual case manager tended to have fewer telephone and direct contacts and a shorter total duration of telephone contact with crisis teams than clients from a non-English-speaking background or clients from an English-speaking background who were not matched with a bilingual case manager. Again, these effects were small.
The results relating to hospital admission are summarized in Table 3. Clients who were born in a non-English-speaking country and clients who had more frequent contact with a continuing care team had longer hospital stays. Clients with a non-English-speaking background who were matched with a bilingual case manager had a shorter hospitalization than clients from a non-English-speaking background who were not matched with a bilingual case manager.
Table 3 also summarizes findings for admission rates and the legal status of admissions—that is, whether the admission was compulsory or voluntary. Diagnosis was the only statistically significant predictor for these two variables; clients with a diagnosis other that a psychotic disorder were admitted more frequently, but those with a psychosis were more likely to be admitted involuntarily.
To examine whether ethnic matching was particularly effective in specific ethnic groups, we did separate regression analyses comparing results for each ethnic group with those for Australian-born clients. The most pronounced effect of ethnic matching was for clients born in Vietnam. Client-clinician ethnic matching was associated with greater contact with continuing care teams for the Vietnamese, Greek, and Italian clients and less contact with crisis assessment and treatment teams for the Vietnamese, Greek, and Macedonian clients compared with the Australian-born clients. Vietnamese clients who were matched with a bilingual case manager had fewer inpatient admissions and a shorter duration of hospitalization than Australian-born clients (results available from the corresponding author).
Discussion
Like several studies of client-clinician ethnic matching in the United States (16,25,27,28,29), this Australian study found that clients with a non-English-speaking background who were matched with a bilingual, bicultural case manager had a higher frequency and longer duration of contact with community services than similar clients who were not matched with a bilingual case manager. This result was found for both direct and telephone contacts.
Supporting the findings of Jerrell (28) and Snowden and associates (30), we also found that ethnic matching was associated with a lower level of contact with emergency crisis assessment and treatment team services for clients with a non-English-speaking background. As for hospitalization, we expected that ethnic matching would be associated with a lower number of admissions, a lower rate of involuntary admission, and shorter stays for clients with a non-English-speaking background. We found an effect for the number of admissions and length of stay, but only for Vietnamese clients.
Ethnic matching was associated with a higher level of contact with community mental health services. This association may have been related to clients' feeling more at ease with case managers of the same background and thus choosing to attend community clinics rather than to avoid them. Similarly, clients who were matched with a bilingual case manager may have been encouraged to contact community services because the shared language minimized the possibility of being misunderstood by mental health staff. The bilingual, bicultural case manager may also have had a better understanding of the client's illness concepts, and clients with a non-English-speaking background may have been more likely to contact community mental health services because they felt that their illness and beliefs were understood.
Because of their higher rate of contact with a continuing care team, clients with a non-English-speaking background who were seen by a bilingual case manager may have received more treatment and may have been less likely to have their treatment interrupted. As a result, they may have had better overall functioning than similar clients who did not have a bilingual case manager. They may also have had fewer relapses and therefore may have required the services of the crisis assessment and treatment team less frequently. Because of their higher rate of contact with community services, any potentially serious symptoms may have been noticed at an early stage of a relapse and an intervention implemented before a crisis occurred. Alternatively, those clients may have turned to the bilingual case manager as a source of support during crises, or they may have been referred back to the bilingual case manager from the crisis assessment and treatment team sooner, because the crisis team staff considered the bilingual case manager better able to work with those clients because of their shared language and culture. The higher rate of contact with continuing care teams for these clients suggests that the bilingual case manager may have taken on some of the crisis response role usually handled by staff of the crisis assessment and treatment team.
Effective community-based treatment may lead to fewer illness relapses and therefore to a lower level of need for hospital admissions. In the study reported here, Vietnamese clients who were seen by a bilingual case manager had fewer hospital admissions per year and spent less time in the hospital per year compared with Australian-born clients or with Vietnamese clients not seen by a bilingual case manager. Several explanations are possible to account for the effect on hospitalization for Vietnam-born clients only. Vietnamese clients generally have poorer English language ability than clients from other ethnic groups in Australia, and communication with staff who are not bilingual may be more difficult for Vietnamese clients and may result in misunderstanding of these clients. Such misunderstanding may lead to misdiagnosis and inappropriate treatment for a mental health problem, which then may have to be addressed in the hospital.
In addition, the cultural distance between the Australian and Vietnamese cultures may be greater than that between the Australian culture and the cultures of other non-English-speaking immigrants to Australia (36). This cultural distance may result in comparatively more cultural misunderstanding of Vietnamese clients, compared with other client groups, and may mean that Vietnamese clients feel less comfortable with nonbilingual mental health workers compared with other clients. The mental health problems of Vietnamese clients may remain untreated until a critical stage in the illness is reached and hospitalization is required, as suggested previously (37).
Finally, like more recent immigrants, Vietnamese clients may experience more current settlement issues, such as finding work, sponsoring relatives to migrate, and coping with diminished social networks and thus may have a high incidence of illness related to these factors. Bilingual case managers may be more attuned to those factors than other staff members and by helping clients with such problems may decrease their rate of hospitalization.
These findings should be interpreted with caution. One limitation of the study was that the clients were not randomly assigned to case managers. Interpreting the correlation between ethnic matching and service use as causal, although consistent with theory, could be regarded as somewhat speculative. The overall amount of variance explained by the predictor models was small, and the effect of any one variable, including ethnic matching, on service use was modest. These modest effects may have been due partly to the way in which the data were provided. Calculating rates of contact for people with very different durations of contact with services, which varied from two weeks to two years, may have increased the apparent variance of the data.
Conclusions
Matching clients with case managers who shared the clients' ethnic background was associated with a higher rate of clients' contact with case managers and a lower rate of contact with crisis services, but the decrease in use of crisis services was not due to increased case manager contact alone. For Vietnamese clients, ethnic matching also reduced the frequency and the duration of hospitalization. These results suggest that ethnic matching should also result in better social functioning for clients from a non-English-speaking background and that the effect of ethnic matching may be more pronounced for more recently arrived groups or those with poorer English language skills.
The results of this study suggest that mental health programs serving culturally and linguistically diverse communities can achieve better service use outcomes by recruiting bilingual staff. The benefits of having bilingual staff members are likely to be most pronounced for newly arrived immigrant groups, and financial efficiencies may be furthered by reducing the number of unnecessary inpatient admissions in these groups. In addition, the results suggest that improvements introduced by client-clinician ethnic matching can be generalized across national boundaries and across substantially different psychiatric treatment systems.
The authors are affiliated with the Victorian transcultural psychiatry unit at St. Vincent's Hospital in Melbourne, Victoria, Australia. Dr. Ziguras is also with the Brotherhood of St. Laurence in Victoria. Dr. Klimidis is also with the Centre for International Mental Health in the department of psychiatry at the University of Melbourne. Send correspondence to Dr. Klimidis, Victorian Transcultural Psychiatry Unit, St. Vincent's Hospital, Bolte Wing, Nicholson Street, Fitzroy, Victoria 3065, Australia (e-mail, [email protected]).
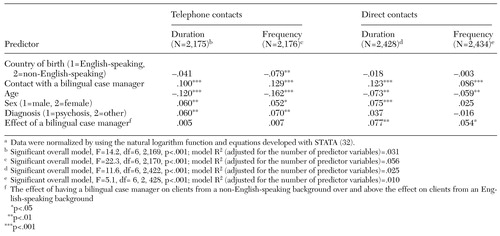 |
Table 1. Standardized regression coefficients showing the relationships between predictors of service use and contacts with continuing care teams among 2,935 clients of the mental health service system in western Melbourne, Australia, 1997-1999a
a Data were normalized by using the natural logarithm function and equations developed with STATA (32).
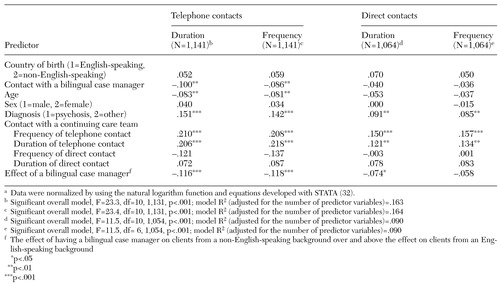 |
Table 2. Standardized regression coefficients showing the relationships between predictors of service use and contacts with crisis assessment and treatment teams among 2,935 clients of the mental health service system in western Melbourne, Australia, 1997-1999a
a Data were normalized by using the natural logarithm function and equations developed with STATA (32).
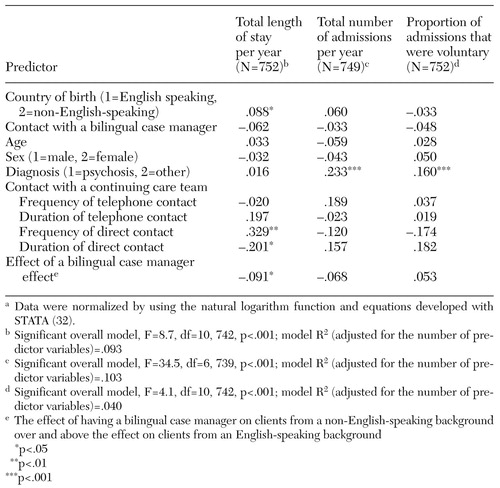 |
Table 3. Standardized regression coefficients showing the relationships between predictors of service use and hospital admission variables among 2,935 clients of the mental health service system in western Melbourne, Australia, 1997-1999a
a Data were normalized by using the natural logarithm function and equations developed with STATA (32).
1. McDonald B, Steel Z: Immigrants and Mental Health: An Epidemiological Analysis. Sydney, Australia, Transcultural Mental Health Centre, 1998Google Scholar
2. Klimidis S, Lewis J, Miletic T, et al: Mental Health Service Use by Ethnic Communities in Victoria, Part I. Melbourne, Australia, Victorian Transcultural Psychiatry Unit, 1999Google Scholar
3. Bruxner G, Burvill P, Fazio S, et al: Aspects of psychiatric admission of migrants to hospitals in Perth, Western Australia. Australian and New Zealand Journal of Psychiatry 31:532-542, 1998Crossref, Google Scholar
4. Minas I: Transcultural psychiatry. Current Opinion in Psychiatry 9:144-148, 1996Crossref, Google Scholar
5. Stolk Y: Access to Psychiatric Services by People of Non-English-Speaking Background in the Western Metropolitan Region of Melbourne: I. An Analysis of Psychiatric Service Use in 1993/94. Melbourne, Australia, Victorian Transcultural Psychiatry Unit, 1996Google Scholar
6. Meinhardt K, Vega W: A method for estimating underutilization of mental health services by ethnic groups. Hospital and Community Psychiatry 38:1186-1190, 1987Abstract, Google Scholar
7. Padgett D, Patrick C, Burns B, et al: Ethnicity and the use of outpatient mental health services in a national insured population. American Journal of Public Health 84:222-226, 1994Crossref, Medline, Google Scholar
8. Gallo J, Marino S, Ford D, et al: Filters on the pathway to mental health care: II. sociodemographic factors. Psychological Medicine 25:1149-1160, 1995Crossref, Medline, Google Scholar
9. Snowden L: African American service use for mental health problems. Journal of Community Psychology 27:303-313, 1999Crossref, Google Scholar
10. Hough R, Landsverk J, Karno M: Utilization of health and mental health services by Los Angeles Mexican-American and non-Hispanic whites. Archives of General Psychiatry 44:702-709, 1987Crossref, Medline, Google Scholar
11. Leong F: Asian Americans' differential patterns of utilization of inpatient and outpatient public mental health services in Hawaii. Journal of Community Psychology 22:82-96, 1994Crossref, Google Scholar
12. Matsuoka J, Breaux C, Ryujin D: National utilization of mental health services by Asian Americans and Pacific Islanders. Journal of Community Psychology 25:141-145, 1997Crossref, Google Scholar
13. Temkin-Greener H, Clark K: Ethnicity, gender, and utilization of mental health services in a Medicaid population. Social Science and Medicine 26:989-996, 1988Crossref, Medline, Google Scholar
14. Scheffler R, Browne Miller A: Differences in mental health service utilization among ethnic subpopulations. International Journal of Law and Psychiatry 14:363-376, 1991Crossref, Medline, Google Scholar
15. Cheung P, Spears G: Illness aetiology constructs, health status and use of services among Cambodians in New Zealand. Australian and New Zealand Journal of Psychiatry 29:257-265, 1995Crossref, Medline, Google Scholar
16. Sue S, Fujino D, Hu L, et al: Community mental health services for ethnic minority groups: a test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology 59:533-540, 1991Crossref, Medline, Google Scholar
17. Trauer T: Ethnic differences in the utilisation of public psychiatric services in an area of suburban Melbourne. Australian and New Zealand Journal of Psychiatry 29:615-623, 1995Crossref, Medline, Google Scholar
18. Klimidis S, McKenzie D, Lewis J, et al: Continuity of contact with psychiatric services: immigrant and Australian-born patients. Social Psychiatry and Psychiatric Epidemiology 35:554-563, 2000Crossref, Medline, Google Scholar
19. Hu T, Snowden L, Jerrell J, et al: Ethnic populations in public mental health: services choice and level of use. American Journal of Public Health 81:1429-1434, 1991Crossref, Medline, Google Scholar
20. Snowden L, Holschuh J: Ethnic differences in emergency psychiatric care and hospitalization in a program for the severely mentally ill. Community Mental Health Journal 25:281-291, 1992Crossref, Google Scholar
21. Hassett A, George K, Harrigan S: Admissions of elderly patients from English-speaking and non-English-speaking-background to an inpatient psychogeriatric unit. Australian and New Zealand Journal of Psychiatry 33:576-582, 1999Crossref, Medline, Google Scholar
22. Falconer B, Ziguras S: Results of the Royal Park Corporation ethnic health audit, in Surviving Mental Illness: Families, Clients and the Mental Health System. Proceedings of the 4th Annual Mental Health Service Conference. Edited by Robertson S, Teeson M, Kellehear K, et al. Sydney, Australia, Mental Health Services Conferences Inc of Australia and New Zealand, 1994Google Scholar
23. Dana R, Behn J, Gonwa T: Checklist for the examination of cultural competencies in social services agencies. Research on Social Work Practice 2:220-223, 1992Crossref, Google Scholar
24. Flaskerud J, Liu L: Effects of an Asian client-therapist language, ethnicity, and gender match on utilization and outcome of therapy. Community Mental Health Journal 27:31-42, 1991Crossref, Medline, Google Scholar
25. Fujino D, Okazaki S, Young K: Asian-American women in the mental health system: an examination of ethnic and gender match between therapist and client. Journal of Community Psychology 22:164-176, 1994Crossref, Google Scholar
26. Takeuchi D, Sue S, Yeh M: Return rates and outcomes from ethnicity-specific mental health programs in Los Angeles. American Journal of Public Health 85:638-643, 1995Crossref, Medline, Google Scholar
27. Flaskerud J, Hu L: Participation in and outcome of treatment for major depression among low-income Asian-Americans. Psychiatry Research 53:289-300, 1994Crossref, Medline, Google Scholar
28. Jerrell J: The effects of client-therapist match on service use and costs. Administration and Policy in Mental Health 23:119-126, 1995Crossref, Google Scholar
29. Ying Y, Hu L: Public outpatient mental health services: use and outcome among Asian Americans. American Journal of Orthopsychiatry 64:448-455, 1994Crossref, Medline, Google Scholar
30. Snowden L, Hu T, Jerrell M: Emergency care avoidance: ethnic matching and participation in minority-serving programs. Community Mental Health Journal 31:463-473, 1995Crossref, Medline, Google Scholar
31. Atkinson D, Lowe S: The role of ethnicity, cultural knowledge, and conventional techniques in counseling and psychotherapy, in Handbook of Multicultural Counseling. Edited by Ponterotto J, Casas J, Suzuki L, et al. Thousand Oaks, Calif, Sage, 1995Google Scholar
32. Stata Statistical Software, Release 5.0. College Station, Tex, Stata Corp, 1997Google Scholar
33. Siegel S, Castellan N: Nonparametric Statistics for the Behavioral Sciences. New York, McGraw-Hill, 1988Google Scholar
34. Statistical Package for the Social Sciences, Version 9.0. Chicago, SPSS, 1998Google Scholar
35. Cohen J, Cohen P: Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ, Erlbaum, 1975Google Scholar
36. Minas H, Stuart G, Klimidis S: Language, culture and psychiatric services: a survey of Victorian clinical staff. Australian and New Zealand Journal of Psychiatry 28:250-258, 1994Crossref, Medline, Google Scholar
37. Stuart G, Minas I, Klimidis S, et al: English language ability and mental health service utilisation: a census. Australian and New Zealand Journal of Psychiatry 30:270-277, 1996Crossref, Medline, Google Scholar



