Long-Stay Patients in State Psychiatric Hospitals at the End of the 20th Century
Abstract
Objectives: The purpose of this study was to assess the characteristics of long-stay patients in contemporary state psychiatric hospitals and to identify factors representing possible barriers to alternative placements for these patients. METHODS: All patients in inpatient units of the Massachusetts Department of Mental Health who had been hospitalized for at least three years as of April 1, 1999, were assessed by their treatment teams with a standardized data collection instrument. Domains assessed included medical problems, need for nursing care, psychiatric diagnosis, and history of problematic behaviors. RESULTS: The 330 individuals identified as long-stay patients had an array of medical problems and nursing care needs that likely would have been manageable in other long-term-care settings. A total of 276 patients had at least one significant medical problem. However, some patients exhibited behavioral problems that might have complicated such placements, especially when behavioral problems co-occurred with the need for medical supervision. A total of 228 patients had exhibited a significant problematic behavior in the previous 30 days. CONCLUSIONS: Although the number of long-stay patients in state psychiatric hospitals declined dramatically during the second half of the 20th century, a small group of patients still requires care in this setting. State psychiatric hospitals continue to occupy a significant niche in the mental health system.
At the end of the 20th century, mental health policy makers focused much of their attention on reducing the use and duration of inpatient psychiatric treatment. In many locales privatization, coupled with restrictions on hospitalization that had been brought about by managed care, significantly reduced the number and duration of inpatient episodes. However, against this backdrop of change there remains a group of individuals who have severe mental illness and who require prolonged care and treatment in public psychiatric hospitals. These individuals pose a challenge to efforts undertaken in the past decade by many state mental health agencies to further reduce the number of beds in state hospitals.
This article describes the contemporary population of long-stay patients in state psychiatric hospitals in Massachusetts. We studied individuals who had been hospitalized for at least three years as of April 1, 1999—six years after the culmination of a significant effort to close state hospitals (1,2,3). We examined the needs and characteristics of these patients in several domains, considered the barriers to discharge and alternative placement, and evaluated the implications of these data for the long-term-care function of the mental health system and the role of state hospitals in fulfilling that function.
Background
The long-term care and treatment of persons who have severe mental illness became a core function of public psychiatric hospitals in the 19th century. By the mid-20th century the census of psychiatric patients in America's state hospitals on any given day exceeded half a million. The process that is popularly called deinstitutionalization, which began shortly thereafter and continued for the rest of the century, significantly reduced the state hospital population. Thus by the mid-1990s just over 72,000 patients resided in these facilities, which translates to a reduction of nearly 90 percent (4,5). Several factors contributed to this decline, including the availability of new pharmacologic treatments for mental illness and the reform of legal mechanisms for involuntary admission and retention in state hospitals. Of particular importance to long-stay populations was the expanded availability of long-term-care settings—such as nursing homes—and the development of community-based residential programs for persons with mental illness, which enabled individuals who did not require acute treatment to be placed in noninstitutional settings (6,7,8,9,10).
Deinstitutionalization has been characterized as entailing two separate but related processes: the transfer of individuals from the hospital to the community and the transfer of the state psychiatric hospital's functions to alternative community-based settings (11). Viewed from this perspective, the long-term-care function and populations of state hospitals can be said to have "co-evolved" with other elements of the larger long-term-care system. For example, descriptions of the state psychiatric hospital population in the first half of the 20th century, before the advent of community-based care, suggest that there was a subpopulation of state hospital patients who had little, if any, clinical need for treatment in a psychiatric facility but who remained hospitalized because they required some nursing or custodial services and lacked the social or economic resources to obtain these services elsewhere (12,13,14).
The expansion of the nursing home industry and federal reimbursement for nursing home care, the development of community-based residential programs for persons with mental illness, and other programmatic innovations have provided alternative settings in which many of these individuals could be placed instead of being admitted to a state hospital (8). The availability of these alternative settings, particularly when coupled with appropriate supportive care, greatly facilitated the reduction of long-stay populations in state hospitals. Indeed, in an intensive court-ordered deinstitutionalization effort in western Massachusetts, the subpopulation of long-stay patients in psychiatric state hospitals was the easiest group to permanently deinstitutionalize (15,16).
During the second half of the 20th century, deinstitutionalization greatly reduced the size of the nation's state hospital population. However, the pace at which this reduction proceeded diminished in the 1970s and 1980s. During that period the long-stay population, although it underwent considerable attrition, nevertheless continued to maintain a presence in state psychiatric hospitals. This population consisted of two groups: a dwindling number of "old long-stay" patients who were hospitalized before deinstitutionalization began and who remained despite it, and a cadre of "new long-stay" patients who began prolonged hospitalizations during the period despite efforts to prevent them (11). The 1990s witnessed renewed efforts by many states to further downsize or to close many of their remaining state psychiatric hospitals (2,3) and to shift the locus of acute inpatient treatment to local general hospitals (17,18).
In Massachusetts, as elsewhere, these privatization efforts were accompanied by expansions in the availability of various kinds of community-based residential programs. However, as with similar efforts that had been attempted earlier, these interventions further reduced—but still did not eliminate—the long-stay population. The patients who remained were those whose behavioral tendencies and other characteristics made them the most difficult to place in the existing array of community settings (19).
Methods
The setting for this study was the system of inpatient facilities maintained by the Massachusetts Department of Mental Health. The long-stay psychiatric patients who were the focus of the study are individuals who, according to the department, were receiving continuing treatment. Since July 1996 these services have constituted the mental health department's primary responsibility for providing inpatient services, given that the acute inpatient system has been mostly privatized. Patients who are served in the continuing-treatment system are those who were admitted for acute treatment to a Department of Mental Health facility before July 1996 without being discharged or were transferred for extended treatment from the acute psychiatric unit of a general hospital or private psychiatric specialty hospital after that date.
The medical directors of all eight Department of Mental Health inpatient facilities were asked to identify patients who were hospitalized as of April 1, 1999, and who met the preceding criteria. Because the study focused on the long-stay patient population, and because we determined that there was significant turnover in that population during the first three years of continuing treatment, only patients who had a length of stay of three years or more were included in the study. Patients who met these criteria were assessed in a variety of domains by the treatment team responsible for their care—arguably the group of individuals who were best qualified to make such assessments.
A structured data collection protocol was used systemwide. This protocol incorporated elements of several instruments with established validity and reliability that were designed for the assessment of persons with severe mental illness, including the New York Level of Care Survey (20), the Nurses Observation Scale for Inpatient Evaluation (21), and the Current Evaluation of Risk and Functioning-Revised (22). In addition, data on patient history were systematically collected from patient records.
In addition to patients' demographic and diagnostic information, data were gathered on length of stay, medical conditions, current (previous 30 days) and lifetime problematic behavioral tendencies that co-occurred with their psychiatric symptoms, and current and lifetime psychosocial histories. The treatment teams provided their opinions about the supports and services that would be required by each patient if he or she were discharged. They also gave their assessments of each patient's readiness for discharge at the time of the assessment and, for patients who were assessed as not being ready, a likely timetable for discharge. The instrument allowed multiple categories in all domains to be selected for each patient.
Results
Patient characteristics
A total of 330 patients met the inclusion criteria and were included in the study. The mean±SD age of the patients was 48.8±12 years, with a range of 21 to 93 years. They were predominantly between the ages of 31 and 60, although a substantial number of patients were 61 or older. The demographic and diagnostic characteristics of these patients are summarized in Table 1. These data show that the long-stay population in Massachusetts state psychiatric hospitals is disproportionately male and disproportionately Caucasian. Schizophrenia or another psychotic disorder was the primary diagnosis for about three-quarters of the patients assessed.
Although patients with mood disorders (depressive and bipolar disorders) were identified by the treatment teams and are commonly observed in state hospital populations and in acute treatment settings, these disorders accounted for only about 10 percent of diagnoses in the long-stay population. A diagnosis of co-occurring substance abuse was noted for about 30 percent of the patients. This proportion is lower than that observed in many populations of persons who have severe mental illness and may reflect the difficulty in identifying such a diagnosis among patients who have been hospitalized for extended periods and thus have been prevented from abusing substances.
Length of stay
Some individuals in our sample were "old long-stay" patients—that is, they had already experienced a long hospitalization at the start of the deinstitutionalization process. The median length of stay was just over seven years, but a substantial number of patients had been hospitalized for more than ten years at the time of assessment, including some patients with stays ranging from 20 to 30 years. One individual, among the state's last remaining old long-stay patients, had been hospitalized for 52 years (data not shown).
Medical conditions
The treatment teams noted a substantial number of medical conditions among the assessed patients, including serious illnesses such as heart disease and cancer. The frequencies of various medical conditions are listed in Table 2. The most commonly observed medical condition was obesity, noted for about 30 percent of the patients. Respiratory disorders were also common; nearly a quarter of the patients were diagnosed as having chronic obstructive pulmonary disease or another serious respiratory problem. A substantial number of patients had more than one diagnosis; the mode was two, and one individual had ten diagnoses. Only 16 percent of the patients had no physical problems at the time of assessment.
Problematic behaviors
The array of problematic behaviors observed in the 30 days before assessment—that is, while the patients were hospitalized—and problematic behaviors that patients were known to have displayed over the course of their lives, both in the hospital and in the community, are summarized in Table 3. These behaviors included the broad category of problems that led to their present hospitalization, such as poor self-care or dangerousness to self or others, as well as more specific behavioral tendencies that had caused difficulties in the hospital or in other environments. This latter category included characteristics that posed problems for hospital staff, such as assaultiveness; behaviors requiring close monitoring, such as abnormal water intake; and other behaviors that might represent threats to public safety, such as a propensity to engage in offensive or illegal sexual behaviors.
Behavioral problems and patients' needs
An important consideration in assessing the possibility of transferring long-stay patients from the state hospital to alternative settings is the need to balance "nursing home-like" functions with behavioral management. The scope of this problem is evident in the overlap of behavioral and medical problems observed in the 30 days before assessment. A total of 217 patients (66 percent) exhibited what staff described as poor self-care even while supervised, and 92 patients (28 percent) were considered to be a danger to themselves or others. Seventy-six patients (23 percent) were in both of these categories.
A similar analysis of lifetime behaviors provided an indication of the potential for placement outside an institutional setting. A total of 272 patients (83 percent) had a history of self-care that was sufficiently poor to raise staff concerns, and 244 (74 percent) were rated as having a history of being dangerous to others; 211 patients (64 percent) exhibited both of these behaviors.
Readiness for discharge
The treatment teams were asked to identify the kinds of settings to which each patient could be discharged, if any. Forty-six patients (14 percent) were deemed to be ready for discharge at the time of assessment, and an additional 36 patients (11 percent) were considered likely to be discharged within six months. Settings that were deemed appropriate included nursing homes, community residential programs with various levels of staffing, and other miscellaneous settings.
Six months after the assessment, the Department of Mental Health client tracking system was queried for the number of patients who had been identified as being ready for discharge and who had actually been discharged. At six months only 19 patients (6 percent) had left the hospital. These 19 accounted for 23 percent of the individuals who had been rated by staff as being ready for discharge at the time of assessment or within the six-month time frame. Note that the assessments of readiness for discharge were based on the judgments of the patients' treatment teams. Clearly the members of these teams knew the patients best; however, the reliability and validity of the assessment process and the consistency of the process across sites or even across teams within sites has not been established. Moreover, such assessments clearly cannot account for changes in patients' clinical status or the availability of community placements over a six-month period.
Discussion
The data presented here describe a group of individuals who had experienced long stays in state psychiatric hospitals—stays that spanned decades in some cases—in an era when such hospitalizations are becoming less and less common. These data, along with observations by members of the treatment team, suggest that for many patients the factors that prevent or delay discharge are not confined to psychiatric symptoms. Indeed, for many individuals it is not their psychiatric illness alone but a combination of behavioral tendencies and clinical factors that necessitates continued hospitalization.
Several patients had medical conditions that might have restricted the range of alternative settings in which they could have been placed. For example, patients who have diabetes or hypertension may require an enhanced level of supervision to ensure that they follow an appropriate medication and dietary regimen. Patients who have impaired vision or hearing or who suffer from arthritis may be restricted in the kinds of physical settings in which they can be placed and may require some assistance in activities of daily living. Likewise, individuals who have difficulty swallowing, who have gastrointestinal disorders, or who are obese may need close dietary supervision. Clearly all of these services could be provided in nursing homes or comparable settings. However, as we have indicated, a co-occurring set of undesirable behavioral tendencies may make such placement difficult for some of these individuals. Thus these patients remain hospitalized.
Another group of patients had behavioral histories that suggested that their placement in a setting with less supervision might trigger a chain of events with undesirable consequences. For example, individuals who have exhibited severe substance abuse or medication noncompliance in previous episodes of community living may repeatedly engage in assaultive or other dangerous behaviors, even if supervised. Although such patients may appear to be clinically stable and to function reasonably well in the supervised environment of state hospitals, members of the treatment team must be cognizant of the course of events that might unfold after discharge and weigh the possible risks to patients and others when assessing readiness for discharge.
Our data also suggest that, in serving the continuing-treatment population, state hospitals are performing an important social function. As we have observed, a number of the patients had histories of dangerous behaviors, including sexual assaultiveness and child molestation. Some of these patients began their state hospital stays as forensic patients, having been referred by the courts to restore their competence to stand trial or having been committed civilly in lieu of criminal sanctions. Thus the criminal justice system, family members, or the community may oppose the release of some individuals to community settings.
Finally, our sample included a subgroup of individuals whose hospital stays had been so long that the appropriateness of transferring them to an alternative setting may have been questionable. For example, it is unclear whether persons who have resided in a state hospital for two decades or more would benefit significantly from a change in residence at that point in their lives. Clearly the preferences of the individuals themselves must be weighed carefully in any decision about their transfer.
Conclusions
In President John F. Kennedy's February 1963 message to Congress about mental health and mental retardation, he argued that "if we apply our medical knowledge and social insights fully, all but a small portion of the mentally ill can eventually achieve wholesome and constructive social adjustment" (23). The president was essentially correct in that belief: in the 37 years since he issued his mandate that a "bold new approach" be taken in the treatment of mental illness, many persons who once might have undergone long-term hospitalization have been spared that experience, thanks to innovations in pharmacologic, psychosocial, and other treatments. The data we have presented also confirm President Kennedy's belief that some individuals need to be hospitalized for extended periods.
At the end of the 20th century the long-advocated replacement of the state hospital by alternative settings and services has in many locales been nearly—if not fully—accomplished. In Massachusetts and in many other states the privatization of acute inpatient treatment and the expansion of community-based services have shifted many of the original functions of state hospitals to other settings. Mental health advocates and policy makers will continue to seek resources to further expand the community-based system and to further reduce reliance on state hospitals.
But therein lies a dilemma. Many of the patients identified in this study may be ready for discharge but may await the availability of services that will enable them to leave the hospital. For some of the patients who were assessed as not being ready for discharge and not likely to be ready in the foreseeable future, the reason may have been that the constellation of community services required to meet their needs in the community either does not exist or would be too costly to create.
In the case of one state hospital, almost the entire patient population, including patients who had been hospitalized for decades, was discharged over a period of about ten years. This outcome required that substantial resources be allocated to planning and creating a range of community placements appropriate to each patient's needs (14,15). However, our data suggest that even if such resources were universally available, obstacles to discharge might nevertheless remain for some patients. The community's resistance to the discharge of individuals who have problematic behavioral histories is likely to persist, regardless of the resources available.
These factors, coupled with the pervasive stigma surrounding mental illness (24), virtually ensure the perpetuation of at least a small long-stay population of psychiatric patients in state hospitals for the foreseeable future. That said, the "small portion" of individuals to whom President Kennedy alluded deserve the best possible care and an optimal environment in which to reside. In meeting the needs of these patients, state hospitals and their long-term-care function continue to occupy a unique and important niche in the system of care for persons who have severe mental illness.
Acknowledgments
The study was supported in part by a Center for Excellence grant from the Massachusetts Department of Mental Health to the Center for Mental Health Services Research at the University of Massachusetts Medical School.
Dr. Fisher, Dr. Geller, Mr. White, and Dr. Lincoln are with the department of psychiatry at the University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, Massachusetts 01655 (e-mail, [email protected]). Dr. Barreira and Ms. Sudders are with the Massachusetts Department of Mental Health in Boston. An earlier version of this paper was presented at the annual meeting of the American Public Health Association on November 11, 1999, in Chicago.
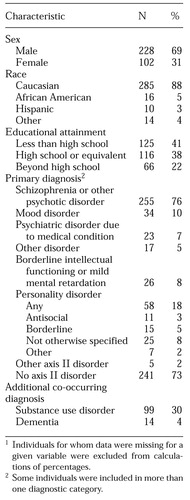 |
Table 1. Demographic and diagnostic characteristics of 330 long-stay psychiatric patients in Massachusetts state hospitals1
1 Individuals for whom data were missing for a given variable were excluded from calculations of percentages
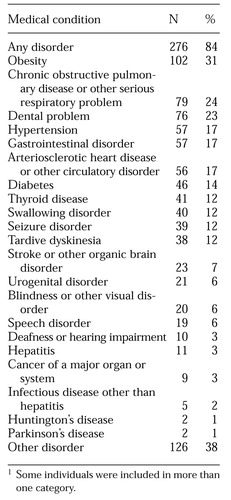 |
Table 2. Prevalence of selected medical problems among 330 long-stay psychiatric patients in Massachusetts state hospitals1
1 Some individuals were included in more than one category
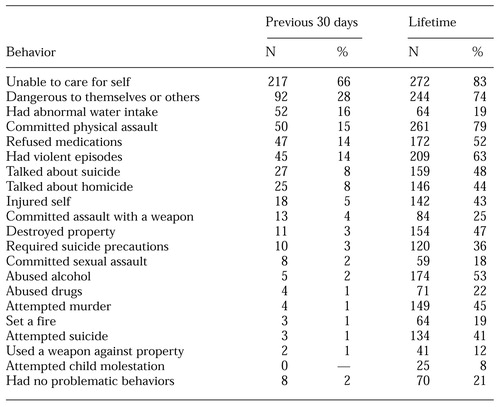 |
Table 3. Current and past problematic behaviors among 330 long-stay psychiatric patients in Massachusetts state hospitals
1. Closing and Re-organizing State Psychiatric Hospitals:1996: State Mental Health Agency Profile System Highlights. Alexandria, Va, National Association of State Mental Health Program Directors Research Institute, 1997Google Scholar
2. Upshur CC, Benson PR, Clemens E, et al: Closing state mental hospitals in Massachusetts: policy, process, and impact. International Journal of Law and Psychiatry 20:199-217, 1997Crossref, Medline, Google Scholar
3. McGrew JH, Wright ER, Pescosolido BA, et al: The closing of Central State Hospital: long-term outcomes for persons with severe mental illness. Journal of Behavioral Health Services Research 26:246-261, 1999Crossref, Medline, Google Scholar
4. Keisler C, Sibulkin A: Mental Hospitalization: Myths and Facts About a National Crisis. Newbury Park, Calif, Sage, 1987Google Scholar
5. Center for Mental Health Services: Mental Health: United States:1998. Edited by Manderscheid RW, Henderson MJ. DHHS pub (SMA) 99-3285. Washington, DC, US Government Printing Office, 1998Google Scholar
6. Geller JL, Fisher WH: The linear continuum of transitional residences: debunking the myth. American Journal of Psychiatry 150:1070-1076, 1993Link, Google Scholar
7. Dorwart RA, Hoover CW: A national study of transitional hospital services in mental health. American Journal of Public Health 84:1229-1234, 1994Crossref, Medline, Google Scholar
8. Brown P: Transfer of Care: Psychiatric Deinstitutionalization and Its Aftermath. New York, Routledge, 1985Google Scholar
9. Geller JL: The last half-century of psychiatric services as reflected in Psychiatric Services. Psychiatric Services 51:41-71, 2000Link, Google Scholar
10. Fisher WH, Geller JL, Pearsall DT, et al: The impact of a continuum of services for the deinstitutionalized, chronically mentally ill elderly. Administration and Policy in Mental Health 18:397-410, 1991Crossref, Google Scholar
11. Bachrach LL: Deinstitutionalization: An Analytical Review and Sociological Perspective. DHEW publication (ADM) 76-351. Washington, DC, US Government Printing Office, 1976Google Scholar
12. Bachrach LL: The state of the state mental hospital in 1996. Psychiatric Services 47:1071-1078, 1996Link, Google Scholar
13. Grob G: Mental Illness and American Society, 1875-1940. Princeton, NJ, Princeton University Press, 1983Google Scholar
14. Morrissey JP, Goldman HH, Klerman LV, et al: The Enduring Asylum: Cycles of Institutional Reform at Worcester State Hospital. New York, Grune & Stratton, 1980Google Scholar
15. Geller JL, Fisher WH, Wirth-Cauchon JL, et al: Second generation deinstitutionalization: I. Brewster v Dukakis's impact on state hospital case mix. American Journal of Psychiatry 147:982-987, 1990Link, Google Scholar
16. Geller JL, FisherWH, Simon LJ, et al: Second-generation deinstitutionalization: II. Brewster v Dukakis's impact on community and hospital utilization. American Journal of Psychiatry 147:988-993, 1990Link, Google Scholar
17. Dorwart RA, Epstein S: Privatization and Mental Health Care: A Fragile Balance. Westport, Conn, Auburn House, 1983Google Scholar
18. Salit SA, Marcos LR: Have general hospitals become chronic care institutions for the mentally ill? American Journal of Psychiatry 148:892-897, 1991Google Scholar
19. Fisher WH, Simon L, Geller JL, et al: Case mix in the "downsizing" state hospital. Psychiatric Services 47:255-262, 1996Link, Google Scholar
20. New York Level of Care Survey. Albany, New York Office of Mental Health, 1976Google Scholar
21. Honigfeld G, Klett CJ: The Nurses' Observation Scale for Inpatient Evaluation: a new scale for measuring improvement in chronic schizophrenia. Journal of Clinical Psychology 21:65-71, 1965Crossref, Medline, Google Scholar
22. Lambert DR, McCorkle BH, Fenby BL, et al: Current Evaluation of Risk and Functioning: Revised (CERF-R). Boston, Massachusetts Department of Mental Health, 1999Google Scholar
23. Kennedy JF: Message From the President of the United States Relative to Mental Illness and Mental Retardation. Presented to the House of Representatives, Feb 5, 1963Google Scholar
24. Link BG, Phelan JC, Bresnahan M, et al: Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health 89:1328-1333, 1999Crossref, Medline, Google Scholar



