Co-occurrence of HIV and Serious Mental Illness Among Medicaid Recipients
Abstract
OBJECTIVE: The authors estimated the treated period prevalence of HIV infection in the Medicaid population and the rate of HIV infection among persons with serious mental illness in that population. METHODS: This cross-sectional study used Medicaid claims data and welfare recipient files for persons aged 18 years or older for fiscal years 1994 through 1996 in Philadelphia. Claims data were merged with welfare recipient files to calculate the treated period prevalence of serious mental illness, defined as a schizophrenia spectrum disorder or a major affective disorder, and HIV infection in the Medicaid population and the odds of receiving a diagnosis of HIV infection among those who had a diagnosis of serious mental illness. RESULTS: The treated period prevalence of HIV infection was .6 percent among Medicaid recipients who did not have a diagnosis of a serious mental illness and 1.8 percent among those who did. After sex, age, race, and time on welfare during the study period were controlled for, patients with a schizophrenia spectrum disorder were 1.5 times as likely to have a diagnosis of HIV infection, and patients with a diagnosis of a major affective disorder were 3.8 times as likely. CONCLUSIONS: The rate of HIV infection is significantly elevated among persons with serious mental illness. Further studies are needed to determine modes of transmission of HIV, special treatment needs, and effective strategies for reducing the risk of HIV infection.
The Centers for Disease Control and Prevention reported 57,806 new cases of AIDS in the United States in 1997 (1). Although this figure represents a reduction from the 1996 figure, prevalence estimates indicate that .6 percent of men and .1 percent of women are infected with HIV (2). The availability of more effective treatments suggests that even as the incidence of new cases decreases, prevalence will not decrease proportionately, because mortality has been reduced in recent years, leaving a growing number of people infected with HIV.
It has been argued that persons with serious mental illnesses such as schizophrenia and major affective disorders are more likely than other people to contract HIV-related diseases. Reviews of HIV risks associated with schizophrenia suggest that this greater risk is a function of lower socioeconomic status, homelessness, higher rates of substance use, and risky sexual behavior, including unprotected sex and prostitution (3,4). It is not known whether serious mental illness per se is associated with an elevated risk of HIV infection or whether persons with serious mental illness have a greater risk as a result of their greater likelihood of poverty, substance use, high-risk sexual behavior, and other factors known to be associated with HIV infection.
Certainly, with few exceptions, studies that have examined the prevalence of HIV seropositivity among persons with psychiatric disorders have found higher rates than those that would be expected in the general population. In a convenience sample of 971 psychiatric inpatient residents, 5.2 percent were seropositive (5). In a sample of 118 psychiatric inpatients with co-occurring psychiatric and substance dependence diagnoses, 27 (23 percent) were seropositive. Although a history of intravenous drug use doubled the risk of seropositivity, a diagnosis of depression independently predicted seropositivity as well (6). In a sample of 62 psychiatric patients in a shelter for homeless men, 12 (19 percent) were found to be seropositive (7). At least five other studies using samples of more than 200 found seropositivity rates of 5 to 7 percent in psychiatric populations (8,9,10,11,12).
The prevalence of psychiatric disorders has also been found to be high among seropositive persons. In a case-control comparison of HIV referrals and general medical referrals, patients who were HIV-positive were five times as likely as other patients to be referred for psychiatric services (13). Myers and colleagues (14) found a greater risk of psychiatric disorders among African-American males in an inner-city community who were HIV positive than among those in the same community who were seronegative.
Walkup and colleagues (15) crossed the New Jersey HIV-AIDS registry and Medicaid claims and found that 5.7 percent of persons listed on the registry had received a diagnosis of schizophrenia, which is much higher than the national prevalence rate of 1 percent (16). They also found that 6.8 percent of persons on the registry had received a diagnosis of a major affective disorder, for a total of 12.5 percent with a serious mental illness. Because their study relied exclusively on Medicaid claims—that is, their subjects were enrollees who had received some treatment—it was not possible to compare the risk of having both serious mental illness and HIV infection with the risk in the Medicaid-enrolled population who may or may not have received treatment.
Although these studies all suggest a high rate of comorbidity between HIV infection and serious mental illness, they share some methodological weaknesses that cloud interpretation of the findings. Most studies used convenience samples, and few compared the rates of seropositivity among persons who had psychiatric disorders with rates among persons who did not.
Despite a strong theoretical rationale for developing community prevalence estimates of HIV infection or AIDS among persons with serious mental illness, such studies are lacking. Without such data, it is impossible to estimate the relative risk of HIV infection among persons with serious mental illness or the relative risk of serious mental illness among persons with HIV infection or AIDS. This relative risk is important for several reasons. If the prevalence of HIV infection is higher among persons with serious mental illness than it is in the general population, then studies of the mechanisms of this additional risk and programs to reduce the risk are needed. In addition, if a significant portion of persons who are infected with HIV are also seriously mentally ill, then treatment programs for HIV infection and AIDS must have a strong psychiatric treatment component.
In this study, we had two hypotheses. The first was that the rate of HIV infection among persons with a diagnosis of a serious mental illness in the Medicaid population in Philadelphia would be significantly higher than the rate in the general Medicaid population. Our second hypothesis was that the rate of serious mental illness among persons with HIV infection would be significantly higher than the rate in the general Medicaid population.
Methods
Sample
The study sample comprised 391,454 individuals aged 18 years or older who were living in Philadelphia and who were eligible for Medicaid at any time between July 1, 1993, and June 30, 1996. Individuals were included in the study only if the welfare recipient files contained valid data on their sex, age, and race. Client Information System Medicaid identifiers were used to match individuals in this data set to the Medicaid claim files.
Measures
Medicaid claim files from July 1993 through June 1996 were used to identify patients who had received treatment for serious mental illness or for HIV infection. Because the Medicaid claim files were inconsistent in their use of the last two digits of the five-digit ICD-9 codes and because diagnoses for a given person were not reliable beyond broad categories of illness, the codes were truncated to three digits. A diagnosis of a schizophrenia spectrum disorder was defined as at least one inpatient or two outpatient ICD-9 codes of 295, and a diagnosis of a major affective disorder was defined as at least one inpatient or two outpatient ICD-9 codes of 296 in the Medicaid claims from the specialty mental health sector. This algorithm was developed by Lurie and colleagues (17) to ensure the accuracy of diagnoses and has been used in similar analyses of Medicaid claims, including the study in New Jersey by Walkup and colleagues (15).
This approach is more conservative than using any treatment for a serious mental illness in any setting by any type of provider, which would probably produce higher estimates of co-occurrence. To ensure that a diagnosis of serious mental illness was made by a mental health professional, only specialty mental health claims were used. However, this definition of serious mental illness is limited by the nature of claims data and does not reflect the degree of impairment or chronicity associated with a diagnosis. ICD-9 codes 042 (HIV infection with specified conditions), 043 (HIV infection that causes other specified conditions), and 044 (other HIV infections) were used to identify an HIV-related diagnosis.
The welfare recipient files from the same period were used to identify the denominator population. These files provide demographic information and the exact dates of individuals' entry into and exit from welfare for each welfare episode.
Analyses
First, any Medicaid claim that contained a diagnosis of HIV infection or serious mental illness was identified. These claims were then aggregated at the individual level to produce three dichotomous markers indicating the presence or absence of HIV infection, schizophrenia spectrum disorder, and a major affective disorder.
Next, the treated period prevalence for any diagnosis of serious mental illness or HIV infection for the sample was calculated. Logistic regression was used to calculate the odds ratio for having an HIV or AIDS-related diagnosis given a diagnosis of a serious mental illness, with age, sex, race, and previous time on welfare controlled for.
Results
Sample description
Basic demographic characteristics of the sample as well as the treated period prevalence of HIV infection and serious mental illness within each group are summarized in Table 1. Of the 391,454 individuals in the sample, 58.8 percent were black, 23.5 percent were white, 3.6 percent were Asian, 11.1 percent were Hispanic, and 2.1 percent were identified as "other"; 58.3 percent were women. The mean±SD age of the study subjects was 40.3±17.6 years. The median time on welfare between July 1993 and June 1996 was 1.9 years.
During the observation period, 8,208 persons (2.1 percent) were treated for a schizophrenia spectrum disorder, and 8,993 (2.3 percent) were treated for a major affective disorder. A total of 2,368 persons (.6 percent) received treatment for HIV infection or AIDS during the period.
Table 2 characterizes the co-occurrence of HIV infection and diagnoses of serious mental illness in the sample. The treated period prevalence of HIV infection or AIDS among Medicaid recipients without a diagnosis of a serious mental illness was .6 percent, compared with 1.2 percent for Medicaid recipients with a schizophrenia spectrum diagnosis and 2.3 percent for those with a diagnosis of a major affective disorder. A total of 4.1 percent of persons who were treated for HIV infection were also treated for schizophrenia, and 8.8 percent were treated for a major affective disorder, compared with only 2.8 percent of the rest of the Medicaid population (χ2= 499.53, df=2, p<.001).
Logistic regression
The results of the logistic regression with diagnosis of HIV infection as the dependent variable are summarized in Table 3. After controlling for sex, age, race, and time on welfare during the study period, the odds ratio for treatment for HIV infection given a diagnosis of schizophrenia was 1.5 (95 percent confidence interval=1.3 to 1.7) and 3.8 (CI=3.5 to 4.1) given a diagnosis of an affective disorder.
Discussion and conclusions
We found that persons on Medicaid with a diagnosis of serious mental illness were about five times as likely as the general Medicaid population to have received a diagnosis of HIV infection. We also replicated the results of other studies in finding that the risk of HIV infection was substantially greater for nonwhites, for persons living in more persistent poverty, and for men. A greater risk of HIV infection among persons with serious mental illness persisted after controlling for age, sex, race, and time on welfare. Although it is possible that seropositivity precedes or is causally related to the development of a major affective disorder, especially major depression, it is likely that schizophrenia and major affective disorders are risk factors for HIV infection.
We used an algorithm that called for the inclusion only of patients who had two outpatient claims or one inpatient claim for services within the specialty mental health sector (17). We used this approach for several reasons, one of which was to replicate and extend the study by Walkup and colleagues (15). If we had instead used any diagnosis of serious mental illness by any type of provider, and if misdiagnosis by nonspecialists is associated with drug use, then we would have artificially inflated estimates of comorbidity, because drug use is an independent risk factor for HIV infection.
Our results were similar to those of the study of New Jersey Medicaid claims by Walkup and colleagues (15). In that study, the estimated treated prevalence of serious mental illness among persons with HIV infection or serious mental illness was 12.5 percent, which is similar to the treated prevalence of 12.3 percent that we found, providing evidence of the robustness of the finding. Walkup and colleagues did not publish the percentage of diagnoses of HIV infection among persons with serious mental illness and did not present a denominator of all Medicaid-eligible individuals, so it is not possible to compare their rates directly with ours.
There are several possible explanations for the strong associations between HIV infection and serious mental illness, and they are not mutually exclusive. Mental illness may be causally related to HIV infection. As we have already suggested, persons with serious mental illness may be more likely to engage in behaviors that place them at high risk of becoming infected with HIV, primarily substance use and high-risk sexual behavior (4). It is also possible that the social marginalization and stigma associated with serious mental illness places persons who have these disorders in proximity to others who engage in high-risk behaviors. Thus, even if the behaviors of persons with serious mental illness are no riskier per se than the behaviors of others, these individuals could be engaging in those behaviors in the company of a group of individuals who have a higher rate of seropositivity.
It is also possible that HIV infection causes serious mental illness. There is evidence that seropositive status, while related to recurrence of previously existing major affective disorders, can also be related to the onset of those disorders (18). There is also some evidence that HIV infection may trigger a psychotic episode and can contribute to first-onset schizophrenia (19). However, these effects are small and could not account for the magnitude of the associations we observed in this study.
Estimates of the large number of undiagnosed cases of HIV infection notwithstanding, two sets of limitations to our prevalence estimates must be considered. The first set relates to the validity of calculating rates of treated disease and infection from Medicaid claims. There are at least four reasons why estimates of true prevalence based on estimates of treated period prevalence gleaned from Medicaid claims are lower-bound estimates.
First, it is likely that some Medicaid-eligible individuals with either serious mental illness or HIV infection did not receive any treatment and thus were not correctly represented. Second, Medicaid-eligible individuals may have received medical services through community clinics that were not billed to Medicaid. Thus some patients in our sample may have received psychiatric or HIV-related treatment or both without those claims appearing in the Medicaid data set. Third, individuals may have received treatment that was paid for by Medicaid before or after the study period without receiving treatment during the study.
Fourth, claims data were available only for individuals who were enrolled in a fee-for-service plan. A proportion of persons who were eligible for Medicaid in Philadelphia were enrolled in health maintenance organizations for at least part of the study period and may have received treatment for a target condition during that time. These individuals were all included in the denominator as not having received treatment for a target condition, because many individuals move back and forth from fee-for-service plans to health maintenance organizations, and no tenable statistical models are currently available to account for this movement in and out of the risk group. However, it is likely that this fourth threat to validity is smaller than the other three, because there is an incentive for individuals who have potentially higher treatment costs to remain in or return to the fee-for-service plan.
On the other hand, a second set of limitations could positively bias the estimates of risk of co-occurrence of HIV infection and serious mental illness. It may be that individuals with both diagnoses are more likely to come into contact with the health system as a function of their co-occurring disorders. It is also possible that persons who have serious mental illness are more likely to be tested for HIV infection, or vice versa, as a function of their contact with providers. This form of bias is often referred to as hospital bias or Berkson's bias (20).
Berkson described this bias as arising from the fact that individuals with two conditions may seek treatment for either one, thus increasing the probability that they will come into contact with the health care system and be diagnosed as having the other condition. Therefore, prevalence estimates of a second condition that are gleaned from a treated sample are likely to overrepresent both the second condition and the co-occurrence of the two conditions in the general population. A number of studies have found higher rates of comorbidity in treated populations than in untreated populations for both psychiatric disorders (21,22,23) and physical health conditions (24,25,26).
For this bias to have had a significant impact on our estimates, persons with a serious mental illness as well as HIV infection would have to have been more likely to seek treatment as well as more likely to be diagnosed as having the other condition once they were receiving treatment for the first condition. Although we are aware of no studies that have examined the impact of either HIV infection or serious mental illness on help seeking, one study found that persons with alcoholism were more likely to seek treatment if they had co-occurring physical conditions (23). However, the presence of the physical condition did not increase the likelihood that the patient would receive an alcohol-related diagnosis.
Certainly, other studies have suggested that the sensitivity of general health professionals to psychiatric disorders is limited (27,28), and confidentiality constraints between physical and mental health settings as well as limits on the availability of resources in mental health settings may preclude HIV testing in psychiatric treatment. Therefore, although these biases may have been present in our study, it is unlikely that they were of sufficient magnitude to account for the robust association between HIV infection and serious mental illness that we found.
The limitations we have discussed relate primarily to problems inherent in any study that uses claims data. Despite these limitations, useful epidemiologic studies can be accomplished by using claims. Welfare recipient data and Medicaid claims data provide large samples and specific information about relatively understudied populations and questions. Claims data probably provide more accurate and unbiased information than self-reports, especially in the case of sensitive topics such as HIV infection and serious mental illness in marginalized populations. Despite the inherent limitations, our findings have important clinical and policy implications.
The treated period prevalence of HIV infection is much higher among Medicaid enrollees with a serious mental illness than in the general Medicaid population. It is likely that persons with serious mental illness engage in behaviors that put them at greater risk of HIV infection. It is also possible that as a result of cognitive and perceptual limitations and distortions caused by the disorder, persons with serious mental illness require different primary prevention strategies to reduce their risk of contracting HIV.
Other issues bear exploration as well. If providers think that persons with serious mental illness are less likely to adhere to treatment, they may be less likely to prescribe a state-of-the-art treatment regimen—such as highly active antiretroviral therapy—for these individuals than for patients who do not have serious mental illness. At least one study has shown that persons with psychiatric disorders are less likely to receive state-of-the-art treatment for physical health problems such as myocardial infarction (29). It is important to explore this issue in relation to HIV infection.
There is no evidence that adherence to treatment for HIV infection is poorer among persons with serious mental illness than in the general population. In fact, in a comprehensive review, Cramer and Rosenheck (30) argued that observed differences in treatment adherence between persons with serious mental illness and other persons are small and may be due to measurement error. They concluded that improvements in methods for measuring treatment adherence in psychiatric populations are needed to determine whether true differences exist. No studies have compared adherence in psychiatric populations of persons who have co-occurring physical health conditions with nonpsychiatric populations of persons who have the same physical health problems.
Conversely, poorer treatment adherence among persons with serious mental illness could lead to poorer outcomes and the development of treatment-resistant strains of HIV in this population.
Of special note is the fact that more than 12 percent of persons who had a diagnosis of HIV infection also had a diagnosis of schizophrenia or a major affective disorder. This large proportion suggests that programs to help persons with HIV infection manage the disease should contain components that address both psychiatric and physical concerns. It is especially important to establish open channels of communication between specialty mental health and general health care sectors to meet the joint needs of this population.
Finally, persons with both serious mental illness and HIV infection require special consideration because of the nature of the two conditions. Case managers must be trained to address the often competing needs of HIV infection and serious mental illness and especially in the management of two complex drug regimens. Research should be conducted into potential interactions of these therapies.
Further studies are needed to determine the modes of transmission and the potentially unique needs of this population in reducing risk and improving treatment.
Acknowledgments
This research was partly supported by grant P30-AI-45008 from the National Institutes of Health and the Developmental Core of the Penn Center for AIDS Research as well as by grant P30-NR-05043 from the Center for Nursing Outcomes Research. The authors thank Barbara J. Turner, M.D., for her helpful comments on an earlier draft.
Dr. Blank Dr. Mandell, and Dr. Hadley are affiliated with the Center for Menta Health Policy and Services Research in the department of psychiatry of the School of Medicine at the University of Pennsylvania, 3535 Market Street, Suite 3020, Philadelphia, Pennsylvania 19104-2641 (e-mail, [email protected]). Dr. Aiken is affiliated with the School of Nursing and the Center for AIDS Research at the University of Pennsylvania, with which Dr. Blank is also affiliated. Dr. Hadley is also with the Center for AIDS Research. This paper is one of several in this issue focusing on the health and health care of persons with severe mental illness.
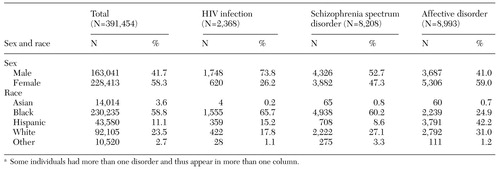 |
Table 1. Demographic and diagnostic characteristics of a Medicaid populationa
a Some individuals had more than one disorder and thus appear in more than one column.
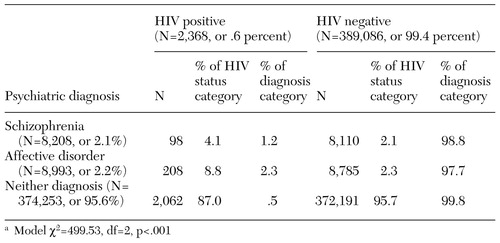 |
Table 2. Co-occurrence of HIV infection and serious mental illness in a Medicaid population (N=391,454)
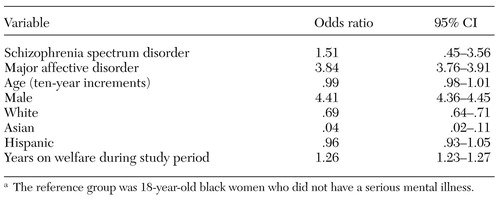 |
Table 3. Results of logistic regression with diagnosis of HIV infection as the dependent variablea
a The reference group was 18-year-old black women who did not have a serious mental illness.
1. Centers for Disease Control and Prevention: New Cases of HIV Infection in the United States. Available at www.cdc.gov/hiv/surveillance.htmGoogle Scholar
2. Karon J, Rosenberg P, McQuillan G, et al: Prevalence of HIV infection in the United States, 1984-1992. JAMA 276:126-131, 1996Crossref, Medline, Google Scholar
3. Sullivan G, Koegel P, Kanouse D, et al: HIV and people with serious mental illness: the public sector's role in reducing HIV risk and improving care. Psychiatric Services 50:648-652, 1999Link, Google Scholar
4. Gottesman I, Groome C: HIV/AIDS risks as a consequence of schizophrenia. Schizophrenia Bulletin 23:675-684, 1997Crossref, Medline, Google Scholar
5. Cournos F, Horwath E, Guido J, et al: HIV-1 infection at two public psychiatric hospitals in New York City. AIDS Care 6:443-452, 1994Crossref, Medline, Google Scholar
6. Silberstein C, Galanter M, Marmor M, et al: HIV-1 among inner city dually diagnosed patients. American Journal of Drug and Alcohol Abuse 20:101-103, 1994Crossref, Medline, Google Scholar
7. Susser E, Valencia E, Conover S: Prevalence of HIV infection among psychiatric patients in a New York City men's shelter. American Journal of Public Health 83:568-570, 1993Crossref, Medline, Google Scholar
8. Cournos F, Empfield M, Horwath E: HIV seroprevalence among patients admitted to two psychiatric hospitals. American Journal of Psychiatry 148:1225-1230, 1991Link, Google Scholar
9. Lyketsos C, Storch D, Lann H, et al: HIV infection in Maryland public psychiatric facilities: results of an informal survey. Maryland Medical Journal 42:571-573, 1993Medline, Google Scholar
10. Sacks M, Dernmatis H, Looser-Ott S, et al: Seroprevalence of HIV and risk factors for AIDS virus in psychiatric inpatients. Hospital and Community Psychiatry 43:736-737, 1992Abstract, Google Scholar
11. Schwarz-Watts D, Montgomery L, Morgan D: Seroprevalence of human immunodeficiency virus among inpatient pretrial detainees. Bulletin of the American Academy of Psychiatry and the Law 23:285-288, 1995Medline, Google Scholar
12. Stewart D, Zuckerman C, Ingle J: HIV seroprevalence in a chronically mentally ill population. Journal of the National Medical Association 86:519-523, 1994Medline, Google Scholar
13. Ellis D, Collis I, King M: A controlled comparison of HIV and general medical referrals to a liaison psychiatry service. AIDS Care 6:69-76, 1994Crossref, Medline, Google Scholar
14. Meyers M: Gain Family Life and Child Care Study. Berkeley, Calif, University of California, Family Welfare Research Group, 1992Google Scholar
15. Walkup J, Crystal S, Sambamoorthri U: Schizophrenia and major affective disorder among Medicaid recipients with HIV/ AIDS in New Jersey. American Journal of Public Health 89:1101-1103, 1999Crossref, Medline, Google Scholar
16. Kessler R, McGonagle K, Zhao S: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
17. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69-71, 1992Abstract, Google Scholar
18. Rosenberger P, Bornstein R, Nasrallah H: Psychopathology in human immunovirus infection: lifetime and current assessment. Comprehensive Psychiatry 34:150-158, 1993Crossref, Medline, Google Scholar
19. Sewell D: Schizophrenia and HIV. Schizophrenia Bulletin 22:465-473, 1996Crossref, Medline, Google Scholar
20. Berkson J: Limitation of the application of fourfold table analysis to hospital data. Biomedical Bulletin 2:47-53, 1946Crossref, Google Scholar
21. Bushnell J, Wells J, Oakley-Browne M: Impulsivity in disordered eating, affective disorder, and substance abuse. British Journal of Psychiatry 169:329-333, 1996Crossref, Medline, Google Scholar
22. Galbaud du Fort G, Newman S, Bland R: Psychiatric comorbidity and treatment seeking: sources of selection bias in the study of clinical populations. Journal of Nervous and Mental Disease 467-474, 1993Google Scholar
23. Helzer J, Pryzbeck T: The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol 49:219-224, 1998Google Scholar
24. Conn H, Snyder N, Atterbury C: The Berkson bias in action. Yale Journal of Biology and Medicine 52:141-147, 1979Medline, Google Scholar
25. Morabia A, Stellman S, Wynder E: Smoking prevalence in neighborhood and hospital controls: implications for hospital-based case-control studies. Journal of Clinical Epidemiology 49:885-889, 1996Crossref, Medline, Google Scholar
26. Roberts R, Spitzer W, Delmore T: An empirical demonstration of Berkson's bias. Journal of Chronic Diseases 31:119-128, 1978Crossref, Medline, Google Scholar
27. Coyne J, Fechnerbates S, Schwenk T: Prevalence, nature, and comorbidity of depressive disorders in primary care. General Hospital Psychiatry 16:267-276, 1994Crossref, Medline, Google Scholar
28. Linzer M, Spitzer R, Kroenke K, et al: Gender, quality of life, and mental disorders in primary care: results from the PRIME-MD 1000 study. American Journal of Medicine 101:526-533, 1996Crossref, Medline, Google Scholar
29. Druss B, Bradford D, Rosenheck R, et al: Mental disorders and use of cardiovascular procedures after myocardial infarction. International Journal of Psychiatry in Medicine 29:361-362, 1999Google Scholar
30. Cramer J, Rosenheck R: Compliance with medication regimens for mental and physical disorders. Psychiatric Services 49:196-201, 1998Link, Google Scholar



