Adherence to Medication Regimens and Participation in Dual-Focus Self-Help Groups
Abstract
OBJECTIVE: The authors examined the associations between attendance at self-help meetings, adherence to psychiatric medication regimens, and mental health outcomes among members of a 12-step self-help organization specifically designed for persons with both chronic mental illness and a substance use disorder. METHODS: A sample of members of Double Trouble in Recovery (DTR) was interviewed at baseline and one year later. Correlates of adherence to psychiatric medication regimens at the follow-up interview were identified for 240 attendees who had received a prescription for a psychiatric medication. RESULTS: Consistent attendance at DTR meetings was associated with better adherence to medication regimens after baseline variables that were independently associated with adherence were controlled for. Three baseline variables were associated with adherence: living in supported housing, having fewer stressful life events, and having a lower severity of psychiatric symptoms. In addition, better adherence was associated with a lower severity of symptoms at one year and no psychiatric hospitalization during the follow-up period. CONCLUSIONS: Treatment programs and clinicians should encourage patients who have both mental illness and a substance use disorder to participate in dual-focus self-help groups that encourage the responsible use of effective psychiatric medication, particularly after discharge to community living. Clinicians also should be sensitive to stressful life events and discuss with patients how such events might affect their motivation or ability to continue taking medication.
Poor adherence to psychiatric medication regimens is a major obstacle to the effective care of persons who have chronic mental illness. A recent review reported that patients who were receiving antipsychotics or antidepressants took an average of 58 percent and 65 percent, respectively, of the prescribed dosages (1). Persons who have both a mental illness and a substance use disorder appear to have the highest risk of poor adherence; studies have usually shown a strong association between substance use and nonadherence (2,3,4,5,6,7,8), although some studies have shown no relationship (9,10).
Substance use may affect medication compliance both directly and indirectly. Active substance use or association with substance users leads to a disorganized lifestyle that can make adherence to a medication regimen difficult. Substance misuse can directly impair judgment about health behaviors (11,12). Substance abuse may function as self-medication, supplanting the use of psychiatric medications that may be perceived as less effective, slow to act, or having more side effects (13). Recovering persons who have dual diagnoses may be influenced by 12-step-oriented treatment staff or self-help groups to avoid taking their medication (14). Substance users may decline medication because of denial of illness, preferring to ascribe their symptoms solely to substance misuse rather than to mental illness because the latter is more stigmatizing; medication, even if accepted initially, is used only temporarily (13,15).
Self-help groups, often based on the 12-step philosophy, have played an important role in furthering the recovery of persons who have addictive disorders as well as persons with mental illness (16,17,18,19,20,21,22). However, some members of 12-step groups who have dual diagnoses report receiving misguided advice about psychiatric illness and the use of psychiatric medications, which are seen as "drugs" (23), although this is not the official view of Alcoholics Anonymous or Narcotics Anonymous (24,25).
Alcoholics Anonymous neither endorses nor prohibits the use of psychiatric medications by its members, and the Alcoholics Anonymous World Service has been open about the organization's limitations—and, by extension, those of other single-purpose mutual-aid groups. A pamphlet about members and medication states: "Because of the difficulties that many alcoholics have with drugs, some members have taken the position that no one in AA should take any medication. While this position has undoubtedly prevented relapses for some, it has meant disaster for others." Also: "No AA member plays doctor," and "Be completely honest with yourself and your physician regarding use of medication" (24). However, there is still aversion to the use of medication in local 12-step chapters, whose members view the use of any psychoactive medications as unacceptable because of the potential for abuse.
Virtually no research has been conducted on the relationship between medication adherence and participation in self-help groups that support the responsible use of psychiatric medications. An exception is a survey of patients and family members who were affiliated with the Depressive and Manic-Depressive Association of Chicago, which found that a belief in the efficacy of medications and adherence to medication regimens improved after participation in this self-help group (26). The study concluded that a patient-run self-help organization can usefully support physicians' recommendations.
In this study we examined the association between the frequency of attendance at self-help group meetings and adherence to psychiatric medication regimens among members of Double Trouble in Recovery (DTR), a 12-step self-help program specifically designed for persons who have chronic mental illness and a substance use disorder. DTR seeks to create "a safe environment where clients can discuss the issues of mental disorders, medication, medication side effects, psychiatric hospitalizations, and experiences with the mental health system openly, without shame or stigma" (27). DTR is a mutual-aid fellowship adapted from the 12-step Alcoholics Anonymous program of recovery. It specifically embraces persons who have a dual diagnosis of a mental and substance use disorder.
DTR was started in New York State in 1989 and currently has more than 200 groups meeting in the United States. Currently the states with the largest numbers of groups are New York, Georgia, Colorado, and New Mexico. New DTR groups are being started continually. Some groups are initiated by consumers, and others are started by professionals who believe that mutual-help fellowships are a useful complement to formal treatment. Groups meet in community-based organizations; psychosocial clubs; day treatment programs for mental health, substance abuse, and dual diagnosis; and hospital inpatient units. All DTR groups, including those started by professionals, are led by persons who are in recovery (28).
We hypothesized that greater attendance at DTR group meetings would be associated with better adherence to psychiatric medication regimens after key factors previously shown to affect adherence among psychiatric patients residing in the community—side effects, recent substance misuse, lack of outpatient contact, and current stress—were controlled for. Furthermore, we hypothesized that better adherence would be associated with improved mental health outcomes after one year.
Methods
Subject recruitment and follow-up
A prospective longitudinal study design was used. Study participants were recruited at 24 DTR meetings—each including ten to 20 members—held in community-based organizations and day treatment programs throughout New York City. Study staff went to the various meetings, explained the study to the DTR members, and invited all members to participate in the study. The only requirement was that participants had to have been attending DTR for at least one month.
Of the 360 attendees who were counted at these meetings, 16 were ineligible because they had less than one month of attendance, and 34 declined to participate either immediately or when they were later contacted for an interview. Thus 310 DTR attendees (86 percent, or about six out of seven attendees) participated in the study. The main reasons for declining to participate were concerns about confidentiality, especially among attendees of meetings held in treatment facilities; the length of the interview; and scheduling conflicts for some individuals who were attending intensive day treatment programs.
Participation was based on the provision of informed consent, and the study was approved by the institutional review board of National Development and Research Institutes, Inc. Recruitment and interviewing were performed by three long-term DTR members—an African-American man and two white women—ranging in age from 30 to 39 years. These individuals had been trained in interviewing techniques by senior research staff. The interviews lasted about two and a half hours. Participants received $35 at baseline and $40 at the follow-up interview for their time.
The baseline interviews of the 310 attendees were conducted between January and December 1998. The one-year follow-up interviews of 277 attendees were conducted between January and December 1999, for a follow-up rate of 90.5 percent of the 306 attendees who were still alive at the end of the follow-up period (four had died). Reasons for nonparticipation in the follow-up interview were that we were unable to locate or contact the attendee (19 attendees), that the attendee refused to participate (six attendees), that the attendee received residential treatment out of state (three attendees), and that the attendee was incarcerated (one attendee).
Study measures
The baseline and follow-up interviews were conducted as part of a broader prospective longitudinal study of the effectiveness of self-help for persons with dual diagnoses. The interview was based on a mix of standardized instruments and both fixed-response and open-ended questions tailored to the study. The variables measured were those that previous theory or research has linked to medication adherence.
In addition to sociodemographic characteristics, the baseline measures included several indexes using either a Likert scale—for example, ranging from 1, strongly agree, to 4, strongly disagree—or dichotomous response items, such as 1, yes, and 0, no; Cronbach's alphas were computed for the data set.
Psychiatric symptoms in the past year were measured with 13 items from the Colorado Symptom Index (CSI) (29), such as "felt depressed," "heard voices," and "forgot important things" (alpha=.85). Perceived coping was measured with 16 items from the Mental Health Confidence Scale (30), such as "How confident are you that you can deal with symptoms of your illness?" and "How confident are you that you can deal with feeling lonely?" Items are ranked on a scale ranging from 1, not at all confident, to 4, very confident (alpha=.89).
Internal motivation to change was measured with 11 items from the Treatment Motivation Questionnaire (TMQ) (31) that were adapted to the DTR context, such as "I came to DTR because it is important to me" and "I accept the fact that I need help and support" (alpha=.86). External motivation to change was measured with four items, also adapted from the TMQ, such as "I came to DTR because of a court order" and "I came to DTR because my counselor said I had to come" (alpha=.71). Social support was measured with 13 items specifically developed for this study, such as "My friends and relatives don't bother with me" and "The people in my life are no help at all" (28) (alpha=.74). The presence of a steady relationship with a spouse or partner was coded as yes or no. The presence of stressful life events in the past year was assessed with 15 items, such as "victim of violent crime" and "close friend or relative died," developed for a previous study of substance users (32).
Drug or alcohol use in the past year and in the past month was assessed with 11 items adapted from the Addiction Severity Index (ASI) (33), such as alcohol use, marijuana use, and crack use, coded as any use or no use. Finally, consequences of drug or alcohol use were assessed with four items—"Did you ever overdose on drugs?"; "Do you ever have blackouts from drugs or alcohol?"; "Do you ever have delirium tremens from alcohol?"; and "Do you have health problems from drugs or alcohol?" Alphas were not computed for drug or alcohol use, stressful life events, or consequences of drug or alcohol use, because these are inventories rather than unidimensional constructs.
Follow-up measures, representing behaviors and circumstances during the past year, were adherence to psychiatric medication regimens, with adherence defined as always taking the medications as prescribed; weekly DTR attendance, coded as yes or no; index of attendance frequency at conventional 12-step groups; type and number of psychiatric medications prescribed; a medication side effects index, consisting of 12 items, such as dry mouth and sleeping problems, rated from 1, not at all, to 4, very much; any psychiatric inpatient stay; living in supported housing; and psychiatric symptoms.
Statistical analysis
The primary goal of the analysis was to test the hypothesis that DTR attendance would be associated with adherence to psychiatric medication regimens. The secondary goal was to identify and control for other correlates of adherence and to determine whether adherence was associated with psychiatric outcomes, such as less mental distress and a lower rate of psychiatric hospitalization.
The analysis was performed with SPSS, version 6.14, using the crosstabs, means, regression, and logistic regression procedures (34). Bivariate statistics—chi square or t tests—were used to compare respondents who were adherent with those who were not on sociodemographic variables and the variables listed above as being potentially relevant to medication adherence. Variables that were significant at less than .1 (two-tailed test) in the bivariate analysis were simultaneously entered into a multiple logistic regression equation with medication adherence as the dependent variable. We used this level of significance to avoid a type II error in the multivariate analysis.
We also used multivariate analysis to examine two mental health outcome measures at follow-up—severity of psychiatric symptoms and presence of a psychiatric inpatient episode—which might be affected by medication adherence. The independent variables in these two analyses were medication adherence and variables that were significantly associated with the given mental health outcome measure. Ordinary least-squares multiple regression was used for severity of psychiatric symptoms, and multiple logistic regression was used for presence of an inpatient episode, both with simultaneous entry. To maintain a sample size of 240 in the multivariate analyses, we used mean substitution to impute missing values for variables; the lowest valid sample size was 228. All regressions exceeded the recommended guideline for the minimum number of cases per variable, which was ten (35).
Results
Among the 277 attendees who participated in the follow-up interview, 240 (87 percent) reported that they had received a prescription for a psychiatric medication during the one-year follow-up period; this constituted the sample for our analyses. The sample comprised 173 men (73 percent) and 67 women (27 percent); 140 participants (59 percent) were black, 58 (24 percent) were white, 30 (13 percent) were Hispanic, and six (3 percent) were from other racial groups. A total of 144 (61 percent) were single; 79 (33 percent) were separated, divorced, or widowed; and 15 (6 percent) were married or considered married under common law. A total of 129 (54 percent) were housed in a community residence or apartment program, 51 (21 percent) lived in their own apartment or house, 25 (10 percent) lived with friends or relatives, 22 (9 percent) lived in a single-room-occupancy residence, and 11 (5 percent) lived in a homeless shelter.
The mean±SD age of the participants was 40±8 years, with a range of 20 to 58 years. The psychiatric diagnoses reported by the participants—not mutually exclusive—were schizophrenia (116 participants, or 48 percent), major depression (55 participants, or 23 percent), bipolar disorder (53 participants, or 22 percent), other (30 participants, or 11 percent), and unknown (48 participants, or 20 percent). Sixty-two participants (26 percent) reported multiple diagnoses. The primary substance of past or current abuse was cocaine or crack (reported by 92 participants, or 39 percent), alcohol (84 participants, or 35 percent), heroin (26 participants, or 11 percent), marijuana (27 participants, or 12 percent), and other (seven participants, or 3 percent).
Attendees who participated in the follow-up interview and those who were lost to follow-up were compared on age, sex, race, marital status, primary substance of abuse, and all independent variables that were found to be significantly associated with medication adherence at follow-up. Attendees who participated in the follow-up had higher mean scores only for perceived coping (r=.15, p<.01).
Medications and adherence
Participants reported 59 separate trade names of psychiatric medications. The mean±SD number of prescribed medications per person was 2.4±.7. The major categories and frequencies of each were conventional antipsychotics, 53 patients (22 percent); atypical antipsychotics, 107 patients (45 percent); selective serotonin reuptake inhibitors, 85 patients (35 percent); tricyclic antidepressants, 13 patients (5 percent); "newer" antidepressants, 51 patients (21 percent); antianxiety medications, 35 patients (15 percent); antimanic or anticonvulsive medications, 81 patients (34 percent); and miscellaneous palliative medications, 103 patients (43 percent).
Of the 240 participants who received a prescription for a medication, 189 (79 percent) were adherent, and 51 (21 percent) were nonadherent. Reasons given by participants for nonadherence—not mutually exclusive—were a belief that he or she no longer needed medication (18 patients, or 35 percent), failure to remember to take the medication (15 patients, or 29 percent), side effects (nine patients, or 18 percent), self-adjustment of the dosage (eight patients, or 16 percent), a dislike of medications (three patients, or 6 percent), drug substitution (three patients, or 6 percent), and other reasons (three patients, or 6 percent).
Correlates of adherence
As can be seen in Table 1, several variables were associated with better adherence to psychiatric medication regimens. They were continuous attendance at DTR meetings, supported housing, fewer side effects of medications, more attendance at other 12-step programs, fewer stressful life events, fewer psychiatric symptoms, no alcohol or drug use in the past year, more external motivation for change, better coping, diagnosis of schizophrenia, multiple diagnoses, other diagnoses, receipt of atypical antipsychotics, and nonreceipt of "newer" antidepressants.
When these variables were entered into a multiple logistic regression on adherence, the variables that were significantly (p<.05) and independently associated with adherence were fewer stressful life events (unstandardized partial regression coefficient B=−.23), less severe psychiatric symptoms (B=−.15), more DTR attendance (B=1.45), and supported housing (B=1.41).
Sixty-seven participants (28 percent) reported some use of alcohol or drugs during the follow-up period, and those who had used substances during the follow-up period were somewhat less likely to be adherent (r=−.13, p<.05). However, we chose to use baseline rather than follow-up measures of substance use in the multivariate analysis because we wanted to establish a time sequence for the purpose of examining substance use versus abstinence as a potential precursor of medication adherence.
Adherence and mental health outcomes
Multiple logistic regression analysis showed that better adherence to medication regimens was significantly associated with absence of an inpatient episode during the follow-up period (B=−1.04). None of the correlates of adherence—more stressful life events at baseline, greater severity of symptoms at baseline, and supported housing—were significantly associated with presence of an inpatient episode in the logistic regression. DTR attendance was excluded from this analysis, because an inpatient hospital stay would logically represent a hiatus in continuous attendance; thus any association between attendance and presence of an inpatient episode could have been artifactual.
The correlates of severity of symptoms at one year as the dependent variable were examined with multiple regression. Three measures were significantly and independently associated with the severity of psychiatric symptoms at follow-up: severity at baseline (B=.40), stressful life events at baseline (B=.23), and adherence (B=−1.33).
Discussion
Although the potential benefit of self-help for persons with mental illness and those who have dual diagnoses is considerable, 12-step groups have not traditionally reinforced adherence to psychiatric medication regimens. This observation is in accord with our finding that participation in traditional 12-step programs such as Alcoholics Anonymous and Narcotics Anonymous was not associated with adherence. However, we found that consistent participation in a 12-step program for persons with dual diagnoses—Double Trouble in Recovery, which supports the responsible use of medication—was associated with better adherence. Moreover, this association could not be explained by other variables often associated with medication adherence among persons who have mental illness.
The overall rate of adherence—79 percent—reported for the one-year study period is at the upper end of the range of rates reported for patients treated with antipsychotic or antidepressant medications (1). Several characteristics of the sample might have contributed to this apparently high adherence rate. For example, only persons who had already been attending DTR meetings for at least a month were included in the study, which suggests a somewhat more adherent group at baseline. In addition, most of the participants remained actively engaged with DTR during the study period, and many were attending outpatient programs or living in supported housing that provided structure and stability.
However, adherence may have been overestimated, because it could be ascertained only by self-report, arguably the least accurate way to measure adherence (1). Thus a cautious interpretation of the data would be to consider the group termed "adherent" as adhering relatively well but probably not perfectly. The adherence rate may also have been overestimated because persons who participated in the follow-up interview were more likely to have had slightly but significantly better coping skills and social support—two characteristics associated with higher adherence in bivariate analysis—at baseline.
The American Psychiatric Association has advised that persons for whom psychoactive medications are prescribed for comorbid psychiatric disorders should be referred to groups in which such therapy is recognized and supported as useful rather than labeled as another form of substance abuse (36). Our study is the first to provide empirical evidence of the effectiveness of this recommendation. The study also showed that the 12-step philosophy is not inherently incompatible with the use of appropriate medication. As the DTR manual states, "DTR can help you overcome secrecy and be more comfortable about having a mental disorder and taking prescription medications" (27). The fact that all members are struggling with the same issues of serious mental illness and substance misuse and their consequences makes it less difficult to discuss and identify the boundaries between the use of medications and the misuse of psychoactive drugs.
Certain factors that might have been expected to be associated with medication adherence were significant in the bivariate analysis but dropped out in the multivariate analysis—for example, side effects and substance abuse. Some previous research has found that side effects are influential (2,37,38), but some has found that they are not (3,39). The participants in our study were mostly long-term users of psychiatric medication, and side effects occurred commonly, possibly to the point that participants had "learned to live with them"; side effects were not mentioned often as a reason for poor adherence. Substance use during the past month was reported infrequently (9 percent of subjects), as might be expected for these regular attendees at 12-step programs, so the data may not have been amenable to the adequate testing of this hypothesis. Participants who had used alcohol or drugs during the follow-up period were slightly but significantly less likely to have been adherent, but the time sequence of substance use and adherence behaviors during the follow-up period is not known.
Lower severity of symptoms at baseline was associated with better adherence to medication regimens during the follow-up period. This finding is similar to those of several previous studies, which found that better adherence was associated with perceptions of symptom relief (40,41), and fewer symptoms were associated with more positive attitudes toward adherence (42). These findings suggest that a perception of benefits from adherence encourages adherence, which is consistent with social learning models of health behavior, such as the health belief model (43).
We included a measure of recent stressful life events in the study because of previous findings that such events were frequent in this population. The degree of recent stress was related to adherence, suggesting that clinicians should be sensitive to such events and should discuss with patients how stress might affect their motivation or ability to continue taking their medication. The higher adherence rate among participants who were in supported housing indicates the value of structured and supportive living arrangements in maintaining adherence.
Medication adherence appears to have consequences that are pertinent to mental health and service use. Respondents who were less adherent reported more severe symptoms of mental illness at the one-year follow-up interview, even after severity of symptoms at baseline was controlled for, and were more likely to have been hospitalized during the follow-up period. These findings indicate that the current generation of psychiatric medications helps alleviate symptoms and the need for expensive interventions, such as hospitalization. Several previous studies have shown associations between better adherence and less severe symptoms (3,5,44), but this study is the first to suggest a relationship with less psychiatric hospitalization as well.
Additional limitations of our study were the use of nonstandardized measures for some of the constructs, as a result of the need to tailor the interview to the study population and to specific topics, and the nonexperimental design, which means that caution is required in making any causal inferences from the results.
Conclusions
Treatment programs and clinicians should encourage patients who have both mental illness and a substance use disorder to participate in dual-focus self-help groups that encourage the responsible use of effective psychiatric medication, particularly after discharge to community living. In that respect, structured, supportive living arrangements appear to be valuable for maintaining adherence to medication regimens. Clinicians also should be sensitive to stressful life events and should discuss with patients how such events might affect their motivation or ability to continue taking their medication.
Increased efforts to facilitate adherence among patients who live in the community are beneficial, because better adherence is associated with less severe psychiatric symptoms and less need for expensive interventions, such as hospitalization. Persons who are in recovery should also encourage their peers who have dual diagnoses to participate in dual-focus groups in addition to more traditional self-help groups.
Acknowledgment
This study was supported by grant R01-DA-11240 from the National Institute on Drug Abuse.
Dr. Magura, Dr. Laudet, Dr. Mahmood, and Dr. Rosenblum are affiliated with the Institute for Treatment and Services Research at National Development and Research Institutes, Inc., 71 West 23rd Street, New York, New York 10010 (e-mail, [email protected]). Dr. Knight is with the Mental Health Empowerment Project in Albany, New York.
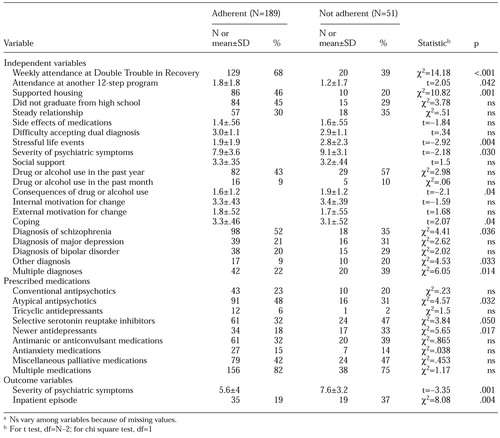 |
Table 1. Characteristics of and outcomes for 240 participants in a dual-focus 12-step self-help program who were adherent to psychiatric medication regimens and those who were not adherenta
a Ns vary among variables because of missing values
1. Cramer JA, Rosenheck R: Compliance with medication regimens for mental and physical disorders. Psychiatric Services 49:196-201, 1998Link, Google Scholar
2. Weiss RD, Greenfield SF, Najavits LM, et al: Medication compliance among patients with bipolar disorder and substance use disorder. Journal of Clinical Psychiatry 59:172-174, 1988Crossref, Google Scholar
3. Olfson M, Mechanic D, Hansell S, et al: Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatric Services 51:216-222, 2000Link, Google Scholar
4. Kampman O, Lehtinen K: Compliance in psychoses. Acta Psychiatrica Scandinavica 100:167-175, 1999Crossref, Medline, Google Scholar
5. Owen RR, Fisher EP, Booth EM, et al: Medication noncompliance and substance abuse among patients with schizophrenia. Psychiatric Services 47:853-858, 1996Link, Google Scholar
6. Kashner TM, Rader LE, Rodell DE, et al: Family characteristics, substance abuse, and hospitalization patterns of patients with schizophrenia. Hospital and Community Psychiatry 42:195-197, 1991Abstract, Google Scholar
7. Drake, RE, Other FC, Wallace MA: Alcohol use and abuse in schizophrenia. Journal of Nervous and Mental Disease 177:408-414, 1989Crossref, Medline, Google Scholar
8. Bergen J, Glenn H, Armitage P, et al: Six-month outcome following a relapse of schizophrenia. Australian and New Zealand Journal of Psychiatry 32:815-822, 1998Crossref, Medline, Google Scholar
9. Warner R, Taylor D, Wright J, et al: Substance use among the mentally ill: prevalence, reasons for use, and effects on illness. American Journal of Orthopsychiatry 64:30-39, 1994Crossref, Medline, Google Scholar
10. Kovasznay B, Fleischer J, Tanenberg-Karant M, et al: Substance use disorder and the early course of illness in schizophrenia and affective psychosis. Schizophrenia Bulletin 23:195-201, 1997Crossref, Medline, Google Scholar
11. Sowers W: Treatment of persons with severe mental illness and substance use disorders in addiction programs. Drug and Alcohol Forum 191:15-21, 1997Google Scholar
12. Walker R: Substance abuse and B-cluster disorders: I. understanding the dual diagnosis patient. Journal of Psychoactive Drugs 24:223-241, 1992Crossref, Medline, Google Scholar
13. Sowers W, Golden S: Psychotropic medication management in persons with co-occurring psychiatric and substance abuse disorders. Journal of Psychoactive Drugs 31:59-70, 1999Crossref, Medline, Google Scholar
14. Zweben JE, Smith DE: Considerations in using psychotropic medication with dual diagnosis patients in recovery. Journal of Psychoactive Drugs 21:221-228, 1989Crossref, Medline, Google Scholar
15. Salloum IM, Moss HB, Daley DC, et al: Drug use problem awareness and treatment readiness in dual-diagnosis patients. American Journal on Addictions 7:35-42, 1998Crossref, Medline, Google Scholar
16. Devine J, Brody C, Wright J: Evaluating an alcohol and drug program for the homeless: an econometric approach. Evaluation and Program Planning 20:205-215, 1997Crossref, Google Scholar
17. Humphreys K, Huebsch P, Finney J, et al: A comparative evaluation of substance abuse treatment: V. substance abuse treatment can enhance the effectiveness of self-help groups. Alcoholism: Clinical and Experimental Research 23:558-563, 1999Crossref, Medline, Google Scholar
18. McCrady BS, Miller WR: Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, NJ, Rutgers Center of Alcohol Studies, 1993Google Scholar
19. Timko C, Moos RH: Outcomes of the treatment climate in psychiatric and substance abuse program. Journal of Clinical Psychology 54:1137-1150, 1998Crossref, Medline, Google Scholar
20. Galanter M: Zealous self-help groups as adjuncts to psychiatric treatment: a study of Recovery, Inc. American Journal of Psychiatry 145:1248-1272, 1988Link, Google Scholar
21. Markowitz F, DeMasi M, Carpinello S, et al: The Role of Self-Help in the Recovery Process. Presented at the annual national conference on state mental health agency services research and program evaluation, held Feb 11-13, 1996, in Arlington, VaGoogle Scholar
22. Commissioner's Report. Albany, NY, New York State Office of Mental Health, 1993Google Scholar
23. The Dual Diagnosis Recovery Book. Minneapolis, Hazelden Foundation, 1993Google Scholar
24. Alcoholics Anonymous: The AA Member: Medications and Other Drugs. New York, AA World Services, 1984Google Scholar
25. Narcotics Anonymous World Services: Bulletin 17. Van Nuys, Calif, 1999Google Scholar
26. Kurtz LF: Use of lithium and other medications by members of a self-help group. Lithium 1:125-126, 1990Google Scholar
27. DTR Inc: Double Trouble in Recovery: How to Start and Run a Double Trouble in Recovery Group. Albany, NY, Mental Health Empowerment Project, 1998Google Scholar
28. Laudet A, Magura S, Vogel H, et al: Support, mutual aid, and recovery from dual diagnosis. Community Mental Health Journal 36:457-476, 2000Crossref, Medline, Google Scholar
29. Shern DL, Wilson NZ, Coen AS: Client outcomes: II. longitudinal client data from the Colorado Treatment Outcome Study. Milbank Quarterly 72:123-148, 1994Crossref, Medline, Google Scholar
30. Carpinello SE, Knight EL, Markowitz FE, et al: The development of the Mental Health Confidence Scale: a measure of self-efficacy in individuals diagnosed with mental disorders. Psychiatric Rehabilitation Journal 23:236-243, 2000Crossref, Google Scholar
31. Ryan RM, Plant R, O'Malley S: Initial motivations for alcohol treatment: relations with patient characteristics, treatment involvement, and dropout. Addictive Behaviors 20:279-297, 1995Crossref, Medline, Google Scholar
32. Magura S, Laudet A, Kang SY, et al: Effectiveness of intensive services for crack-dependent women with newborns and young children. Journal of Psychoactive Drugs 31:321-338, 1999Crossref, Medline, Google Scholar
33. McLellan AT, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:19-21, 1992Crossref, Google Scholar
34. Norusis MJ: SPPS for Windows: Advanced Statistics, Release 6.0. Chicago, SPSS, Inc, 1993Google Scholar
35. Harrell FE: Regression modeling strategies for improved prognostic prediction. Statistics in Medicine 3:143-152, 1984Crossref, Medline, Google Scholar
36. American Psychiatric Association: Practice guidelines for the treatment of patients with substance abuse disorders: alcohol, cocaine, opioids. American Journal of Psychiatry 152(Nov suppl):1-59, 1995Google Scholar
37. Ruscher SM, de Wit R, Mazmanian D: Psychiatric patients' attitudes about medication and factors affecting noncompliance. Psychiatric Services 48:82-85, 1997Link, Google Scholar
38. Hoge SK, Appelbaum PS, Lawlor T, et al: A prospective multicenter study of patients' refusal of antipsychotic medication. Archives of General Psychiatry 47:949-956, 1990Crossref, Medline, Google Scholar
39. Fleischhacker WW, Meise U, Gunther V, et al: Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatrica Scandinavica 382(suppl):11-15, 1994Google Scholar
40. Adams SG, Howe JT: Predicting medication compliance in a psychotic population. Journal of Nervous and Mental Disease 181:558-560, 1993Crossref, Medline, Google Scholar
41. Smith JA, Hughes ICT, Budd RJ: Non-compliance with anti-psychotic depot medication: users' views on advantages and disadvantages. Journal of Mental Health (UK) 8:287-296, 1999Crossref, Google Scholar
42. Draine J, Solomon P: Explaining attitudes toward medication compliance among a seriously mentally ill population. Journal of Nervous and Mental Disease 182:50-54, 1994Crossref, Medline, Google Scholar
43. Rosenstock IM, Strecher VJ, Becker MH: Social learning theory and the health belief model. Health Education Quarterly 15:175-183, 1988Crossref, Medline, Google Scholar
44. Dixon L, Weiden P, Torres M, et al: Assertive community treatment and medication compliance in the homeless mentally ill. American Journal of Psychiatry 154:1302-1304, 1997Link, Google Scholar



