Lifetime Use of Mental Health and Substance Abuse Treatment Services by Incarcerated Women Felons
Abstract
OBJECTIVE: This study examined the lifetime use of alcohol, drug, and mental health treatment services by recently incarcerated women prison inmates. METHODS: A total of 805 women entering a North Carolina prison for new felony charges in 1991 and 1992 were interviewed in person shortly after incarceration. The women were assessed for psychiatric disorders and lifetime use of substance abuse and mental health treatment services. Rates of service use were analyzed by inmate characteristics and were compared with rates for a sample of women in the community in North Carolina. RESULTS: The majority of women inmates reported a history of using substance abuse services or mental health services or both. Those with psychiatric disorders and prison recidivists were the most likely to have used such services. Rates of service use were substantially higher for the inmates than for the women in the community, even when the effects of having a psychiatric or substance use disorder were controlled for. CONCLUSIONS: Many of the incarcerated women in the study met lifetime criteria for alcohol, drug, and mental health disorders that were significantly related to their use of substance abuse and mental health treatment services. The majority of the inmates met criteria for a current disorder despite past treatment. Further research is needed to help in developing programs to reduce women inmates' alcohol, drug, and mental health problems.
The number of women in jail, in prison, on probation, or on parole in the United States has increased dramatically over the past 20 years and now exceeds 950,000 (1). The number of female prison inmates increased from 7,389 in 1974 to 82,594 in 1999 (2). Despite these increases, few studies have described the characteristics of female criminal offenders. We know that most have been arrested for a drug or property crime, have substance use problems, and are mothers (3,4,5,6,7). Female criminal offenders also have a high rate of HIV infection (8,9,10). Although studies with small samples or convenience samples have suggested that female criminal offenders have a variety of psychosocial problems (11,12,13), research is needed to document the extent of these problems.
In 1996 we reported prevalence estimates for specific psychiatric disorders from a large-scale study of women prison inmates, the Women Inmates' Health Study (14). The majority of the sample met diagnostic criteria for a lifetime substance use disorder, and rates for some other psychiatric disorders were higher than those in the general population. Almost half of the inmates met criteria for a current disorder. Teplin and colleagues (15) found similarly high rates of psychiatric and substance use disorders among female jail inmates.
Despite the high prevalence of psychiatric disorders in this population, we are aware of no systematic examinations of the mental health and substance abuse treatment patterns of female criminal offenders. However, two studies developed estimates of the proportion of incarcerated women who have received substance abuse treatment. In a 1994 study of women entering prison in Texas, 56 percent reported having previously received substance abuse treatment (16). Also, in a 1987 national survey of incarcerated adolescent and adult females, 68 percent of the adults indicated that they had participated in a substance abuse treatment program (17).
The purpose of this study was to deepen our understanding of the use of mental health and substance abuse treatment by incarcerated female felons. The study used data from the survey sample in the Women Inmates' Health Study to address the following research questions. First, among women recently imprisoned in North Carolina and assessed soon after incarceration, what are the bivariate relationships between the women's demographic and clinical characteristics and their lifetime use of mental health and substance abuse treatment services? For example, are white inmates more or less likely than nonwhite inmates to use such services? What proportion of women with a mood disorder have received mental health and substance abuse treatment, and how does this utilization rate compare with the rate for women without a disorder or with a different disorder? Second, in multivariate analyses in which the dependent variable is use of services versus no use of services, what characteristics or disorders are significantly related to the use of specific types of services, when the effects of all other independent variables are controlled for? Third, how do the utilization rates for mental health and substance abuse treatment services among female felons compare with rates for women from a community sample, if the effects of psychiatric and substance use disorders are controlled for?
Methods
The Women Inmates' Health Study
Data for the study were collected between 1991 and 1992 at the only prison to which newly sentenced female felons in North Carolina were admitted. (A felony is an offense for which the minimum sentence is one year or longer.) Study subjects included all women entering prison for a new felony charge during that period, except for a few months during which there was a large number of intakes, from which a random sample was selected. For the high-intake months, sampling weights were used to adjust for the probability of selection (18). For example, if one of every three women was randomly selected in a month, the weighting for these subjects would be the inverse of the selection probability, which is three. Only 6 percent of the entire sample consisted of women who entered prison during the high-intake months. The subjects were interviewed shortly after intake. The study was approved by the Research Triangle Institute's institutional review board.
The survey interviewers for the Women Inmates' Health Study conducted 805 in-depth, face-to-face interviews in private. The mean duration of the interviews was 2.5 hours. Emphasis was placed on assuring participants that responses would not be shared with prison authorities or staff. Written informed consent was obtained, and a package of toiletries was the honorarium. The response rate was 95 percent; the remaining 5 percent were lost to follow-up, primarily as a result of transfer to another facility or release.
Assessment of psychiatric disorders
A detailed discussion of the instruments used for psychiatric assessment has been published elsewhere (14). DSM-III-R (19) diagnostic criteria were used. Most specific psychiatric disorders were assessed with the Composite International Diagnostic Interview (CIDI) (20,21). Because the CIDI does not have a module that identifies antisocial personality disorder, the Diagnostic Interview Schedule (22) was used to assess participants for that disorder. Because neither of the two instruments assesses borderline personality disorder, we used a modification of the borderline personality disorder module of the Diagnostic Interview for Personality Disorder, Revised (23).
Rates of service use for North Carolina women inmates grouped by disorder were compared with rates for a sample of North Carolina women of comparable age from the Duke site of the Epidemiologic Catchment Area (ECA) survey (24). More than 90 percent of the women in the ECA sample were community residents, and we refer to them here as the community sample. The ECA used the Diagnostic Interview Schedule and DSM-III (25) criteria. The CIDI was developed from the Diagnostic Interview Schedule, and rates of disorders found by using the two instruments should be similar.
The specific alcohol, drug, and mental health disorders considered in this analysis included mood disorders (major depressive episode and dysthymia), anxiety disorders (generalized anxiety disorder and panic disorder), and substance use disorders (alcohol abuse and dependence and drug abuse and dependence), as well as antisocial personality disorder and borderline personality disorder. We chose not to assess psychotic disorders. The assessment of such disorders is time-consuming, and the prevalence estimates were expected to be low (1 to 2 percent) and thus possibly unreliable. In addition, the number of cases would have been too small to distinguish any significant effects for this group in multivariate analyses. The prevalence estimates reported here are lifetime estimates, that is, the disorder may have occurred at any time in the subject's life. We also assessed exposure to extreme or traumatic events (that is, criterion A for posttraumatic stress disorder) by using a modification of the instrument used by Resnick and colleagues (26) in their national study of rape.
Service use
Treatment included both inpatient and outpatient services. Substance abuse treatment also included self-help groups, such as Alcoholics Anonymous, and detoxification.
For the comparisons between the inmates and the women in the community, services were classified as self-help groups targeting substance use problems, discussions about drug or alcohol problems when visiting a health care provider for a physical health problem, use of any substance abuse treatment services, use of mental health treatment or substance abuse treatment, and use of outpatient services for a physical health problem in the previous six months. Besides allowing a comparison of the overall use of medical services between the two groups, the latter category of services was used as an indicator of overreporting. If inmates tended to overreport service use, their rates of reporting physical health services would have been higher than those of the community women.
Because the inmates were interviewed within days after their admission to prison, the services they reported were virtually all received before their current incarceration. We did not know whether any of the reported services were received during a previous incarceration.
Other variables
The demographic variables included age, race, education, and marital status. A dichotomous variable was used to identify women who indicated that public assistance was their primary income source at the time of the arrest. Another variable specified whether participants had been incarcerated for a drug-related crime or a non-drug-related crime. The two categories were mutually exclusive, and women who were incarcerated for both types of crime were included in the drug-related crime category. A recidivism variable identified women who had previously served time in jail or prison.
Statistical analysis
Analyses were weighted to account for the probability of selection and, for the ECA data, for design effects. Therefore, all reported statistics, including prevalence estimates, are weighted estimates. Sample sizes, however, are given as actual (unweighted) numbers. For the bivariate analyses, chi square tests were used to determine whether rates of service use varied by the levels of the independent variables.
In the bivariate analyses, the variables indicating use of any substance abuse treatment and use of any mental health treatment were coded independently of one another—that is, whether or not the woman used the other type of treatment. Thus the treatment groups overlapped, and the sum of the sample sizes across the groups is greater than 805.
Next, a multivariate analysis was conducted to determine the relationship of the independent variables to different types of service use, with the effects of the other independent variables controlled for. For these analyses, a four-level variable was created in which the substance abuse treatment and mental health treatment groups were mutually exclusive—that is, the sample was divided into those who received only mental health treatment, only substance abuse treatment, both mental health and substance abuse treatment, and no treatment (the contrast group). Therefore, in the regression analyses, we used a multinomial (four-level) logit model that could accommodate nominal dependent variables (27). The multinomial logit model was analogous to the use of three separate binary logistic regression models comparing mental health treatment only versus no service, substance abuse treatment only versus no service, and both mental health and substance abuse treatment versus no service. For each independent variable, such as recidivism, three sets of odds ratios were calculated: one for mental health treatment only, one for substance abuse treatment only, and one for mental health treatment plus substance abuse treatment—all three relative to no service use. For example, for recidivists the odds ratio for mental health treatment only was 1.9. Thus, recidivists were 1.9 times as likely as nonrecidivists to have received only mental health treatment than to have received no treatment.
With samples this large, the expected values of the estimates would be the same for the four-level model as for four separate binary regression models. The multinomial model had the advantage of lower variances.
In the final analytic step, which compared women inmates and community women, prevalence estimates and their associated standard errors were generated by using standard analysis weights for the ECA study. These analyses were conducted with the Crosstab procedure from the Survey Data Analysis (SUDAAN) statistical package to account for the complex sampling design of the ECA (28).
Results
Demographic characteristics
Detailed sociodemographic characteristics of the sample have been reported elsewhere (14). Drug-related offenses were the most common type of offense for which the women were admitted to prison. Fifty-four percent of the sample had been previously incarcerated.
Prevalence of service use
Rates of service use for inmates grouped by demographic and other characteristics are listed in Table 1. A slight majority of women (53.5 percent) reported that they had received mental health or substance abuse treatment or both in their lifetime. Thus almost half of the sample (46.5 percent) had received no mental health or substance abuse treatment. A substantial minority (42.7 percent) had received substance abuse treatment. About a quarter (25.7 percent) had received mental health treatment; 15.7 percent had received inpatient mental health services and 20.1 percent outpatient services (data not shown). The rate of substance abuse treatment for recidivists was significantly higher than the rate for women who were incarcerated for the first time. Overall, rates of service use tended to be higher among white women, those who had been married, recidivists, and women convicted of a non-drug-related crime.
Table 2 shows the lifetime rates of service use among women who had a psychiatric or substance use disorder and those who did not. The general pattern is the same across the different disorders and the different service categories—significantly more women with each disorder had received services than women without that disorder. In addition, those with mood disorders, anxiety disorders, borderline personality disorder, or antisocial personality disorder were more likely than those with a substance use disorder to use mental health treatment. Those who had experienced a traumatic event also had higher rates of both types of service use than those who had not experienced a traumatic event.
Psychiatric disorder, trauma, and service use
Table 3 presents the results of the final regression analysis examining the predictors of service use. Antisocial personality disorder was the only disorder that was not significantly associated with service use; therefore, it was excluded from the model. Although experience of trauma was not significantly associated with service use, it was retained in the model so that we could examine the effect of trauma on service use when the analysis controlled for the effects of psychiatric and substance use disorders. Race, education, marital status, public assistance, drug-related crime, and recidivist status were retained in the model irrespective of their significance because of their potential roles as intervening variables.
Table 3 presents the odds ratios and associated chi square and p values for the relationship between each of the independent variables and use of the three types of services. For all three dependent variables—that is, specific types of services use—the comparison group consisted of participants who had received neither mental health treatment nor substance abuse treatment.
The only demographic or other characteristic consistently associated with service use was recidivism; marital status and type of crime were the only other characteristics significantly associated with any level of service use for mental health treatment or substance abuse treatment. After the analysis controlled for the effects of demographic characteristics and psychiatric disorders, experience of trauma was not significantly associated with service use.
For those who reported receiving only mental health services, mood disorder was the only disorder significantly associated with receipt of services. After demographic and other characteristics as well as other psychiatric and substance use disorders were controlled for, women with a mood disorder were 6.8 times more likely to have received only mental health services than those without a mood disorder. For those receiving only substance abuse treatment services, borderline personality disorder, drug abuse or dependence, and alcohol abuse or dependence were all significantly associated with service use. A significant interaction between alcohol and drug abuse or dependence was also found. In addition, women who had a drug use disorder, with or without an alcohol use disorder, were more likely to have received substance abuse treatment than those who had no substance use disorder or only an alcohol use disorder.
The final category was use of both mental health and substance abuse services. All disorders, except antisocial personality disorder, were positively related to having received a combination of mental health and substance abuse treatment. Women with both an alcohol use disorder and a drug use disorder were the most likely to have received combined treatment (odds ratio=34.87).
The logit model results reported in Table 3 differ from the bivariate findings listed in Table 1 and Table 2. Possible reasons for the differences include the lack of control in the bivariate analyses for the effects of other psychiatric disorders, substance use disorders, and subject characteristics. Also, the definitions of service use in the two types of analysis were slightly different—the bivariate analyses did not exclude from the mental health treatment group those who had also used substance abuse treatment services, but the treatment groups were mutually exclusive in the multivariate analyses. The generalized logit model enabled us to examine the results for those who received only mental health treatment separately from the results for those who received both mental health and substance abuse treatment. The findings suggest that women who received both mental health and substance abuse treatment—that is, the majority of those who received mental health treatment—account for the majority of the significant differences in both the bivariate and the logistic regression analyses.
In summary, the multivariate analyses found a significant relationship between lifetime prevalence of all psychiatric disorders assessed, except antisocial personality disorder, and lifetime use of both mental health and substance abuse treatment services. Having met lifetime criteria for a mood disorder was associated with having received mental health treatment but not substance abuse treatment, and both substance use disorders and borderline personality disorder were related to having received substance abuse treatment services but not mental health treatment.
Comparison with community sample
Table 4 compares rates of service use for inmates and a community sample of women in North Carolina. Use of outpatient medical services for a physical health problem in the previous six months was only slightly higher among the inmates. In both samples, rates of physical health service use tended to be somewhat higher for women with a diagnosable disorder. In the entire sample, however, the proportion of study participants who used mental health and substance abuse treatment services was between two and 20 times higher for the inmates than for the community women. Even among those with a disorder, the rates of service use for inmates were substantially higher than the rates for community women.
Discussion and conclusions
In the bivariate analyses, we found that women with certain characteristics were more likely to use services than their counterparts. These characteristics were being white, married, or incarcerated for a non-drug-related crime, having previously served time in jail or prison, or having met lifetime criteria for a mental health or substance use disorder. For example, white women were more likely to use services than nonwhite women, and married women were more likely than unmarried women. When the effects of all other independent variables were controlled for, the multivariate analyses revealed that only the following attributes were significantly related to having received either substance abuse or mental health treatment or both: having previously served time in jail or prison, being married, being incarcerated for a non-drug-related crime, and meeting lifetime criteria for a substance use, mood, or anxiety disorder or borderline personality disorder.
One striking finding is that more than half of the women entering prison for a felony charge in North Carolina had received mental health or substance abuse treatment services at some time in their lives, and almost half of those who had received mental health services had received inpatient services. To put this in perspective, it is important to remember that the majority of these women had had a lifetime psychiatric or substance use disorder, and, despite high rates of previous treatment, almost half had a current disorder. The rate of mental health or substance abuse treatment for community women of similar age was about 13 percent.
Furthermore, at least three-quarters of the women inmates with a psychiatric or substance use disorder had received services for their disorder, compared with 28 to 37 percent of the community women with a disorder. Because the rates of use of physical health services among the inmates and the community women were similar, the differences between the groups do not appear to be explained by overreporting of service use by inmates. The differences between the groups may have been due to greater severity of illness among the inmates, whose symptoms may have been so severe that they may have engaged in illegal behaviors such as violent assault or stealing to get money for drugs.
Alternatively, the inmates, who tended to have low incomes, may have received public treatment that was unavailable to many community women with higher incomes. Or, because many inmates with a disorder had already spent time in jail or prison, they may have received assessment and treatment during previous incarcerations, as mandated by law. However, Teplin and colleagues (15) and others have found that most individuals with psychiatric disorders who are incarcerated usually do not receive treatment. Furthermore, other findings suggest that the differences between the inmates and the North Carolina women in the ECA sample were not primarily the result of treatment during previous incarcerations: the rate of mental health and substance abuse treatment among first-time inmates was high; at the women's prison where the study was conducted, very few mental health treatment services were available; some studies have reported elevated rates of prior arrest and incarceration among community clients in substance abuse treatment and among psychiatric hospital patients (29,30).
Although the bivariate analysis found that trauma was related to lifetime service use, this relationship seems to have been mediated by the presence of a lifetime disorder, and the relationship was not found when the analysis controlled for the effects of disorder. Recidivism was the most robust predictor of service use among inmates.
These findings suggest that there is a subgroup of troubled women whose impairments result not only in their receiving mental health or substance abuse treatment services, or both, but also in their being repeatedly incarcerated. These women reported a high rate of substance use as well as impulsive and reckless behaviors, such as driving drunk or physically attacking others (data not presented). Their arrest and incarceration may have been related to behaviors associated with their psychiatric or substance use disorders.
Because we have no detailed information about the characteristics of the mental health and substance abuse services the women used, we do not know why, despite having been in treatment, they continued to exhibit fairly serious mental health problems and to engage in activities that led to arrest and incarceration. One hypothesis suggested by the high prevalence of exposure to trauma among the inmates is that their disorders may be trauma related, and previous treatment may not have addressed traumatic experiences.
An alternative explanation is that, in addition to having mental health and substance use problems, many of these women live in chaotic environments and have poor interpersonal, job, problem-solving, and other skills. Thus mental health or substance abuse treatment services without wraparound services may be of limited benefit, especially if the women return to the environment in which their problems developed. Moreover, we have no data on the amount and quality of treatment. Thus treatment may have been of limited duration or of poor quality, the women may not have adhered to treatment or may have dropped out, or they may have been unable to afford medications that were prescribed. Finally, research suggests that persons with severe drug or alcohol problems may require multiple treatment episodes.
One caveat that must be considered in interpreting the study findings is that the data were collected almost ten years ago. During that interval, the treatment histories of incarcerated women offenders may have changed. The demographic characteristics and proportions of women committing different categories of crime have not changed substantially in that time, which suggests that the characteristics of women inmates have not changed substantially. However, in North Carolina, as in many states, access to and availability of services have decreased in the past ten years (31). Thus rates of use may have decreased somewhat. Nevertheless, nearly half of the inmates in our study who received mental health services had used inpatient services, which suggests the presence of severe symptoms. Thus many would likely have received some treatment even if services were less available overall.
The high rates of psychiatric disorders found at the time of entrance to prison suggest a need for additional treatment resources for incarcerated women. The law mandates the right to treatment for serious mental health problems (15). Unfortunately, few services are available to these women at a time when they may be most amenable to change. For example, among women entering prison in Texas, 56.4 percent responded positively when asked if they would be interested in participating in a drug or alcohol treatment program "at this time" (16). The rapidly increasing rate of incarceration among women—and among men—often means that prison dollars are spent on beds and buildings and not on treatment and other services.
More research is needed to determine how best to address the alcohol, drug, and mental health problems of women inmates. One option might be to provide in-prison treatment that addresses inmates' specific problems and circumstances, including postrelease services. Another option would be to incarcerate fewer women—most are not violent offenders—and use the money saved to provide intensive outpatient treatment services, including wraparound services, that focus on the multiple needs of these women.
Previous studies have demonstrated that substance abuse treatment can reduce rates of criminal offenses and rearrest (32,33), and some research has suggested that treatment can also reduce recidivism for some offenders with mental disorders (34,35,36). However, providing services to offenders has generally not been seen as a worthwhile expenditure of public funds, even though such services may have a cost-offset benefit by reducing recidivism and the need for other costly services, such as social and child welfare services, and even though such services may reduce the impact these women's problems have on their lives, their children, and their communities.
Acknowledgments
This work was funded by grants DA-06387 and DA-10178 from the National Institute on Drug Abuse. Preparation of the report was partly supported by research funds from the Department of Veterans Affairs Health Services Research and Development Service.
Dr. Jordan, Dr. Schlenger, and Dr. Caddell are affiliated with Research Triangle Institute, 3040 Cornwallis Road, P.O. Box 12194, Research Triangle Park, North Carolina 27709-2194 (e-mail, [email protected]). Dr. Burns and Dr. Fairbank are with the department of psychiatry and behavioral sciences at Duke University Medical Center in Durham, North Carolina. Dr. Federman is with the department of biostatistics and informatics at the University of Wisconsin in Madison.
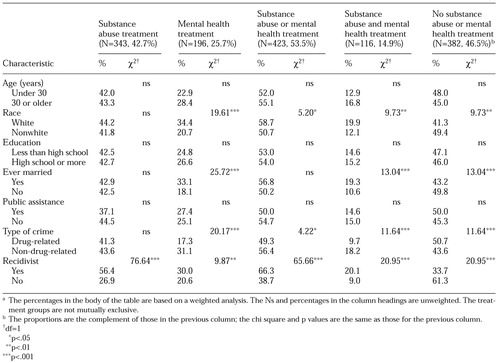 |
Table 1. Lifetime use of substance abuse and mental health treatment services among 805 recently incarcerated women prison inmates in North Carolina, by demographic and criminal justice characteristicsa
a The percentages in the body of the table are based on a weighted analysisThe Ns and percentages in the column headings are unweighted. The treatment groups are not mutually exclusive.
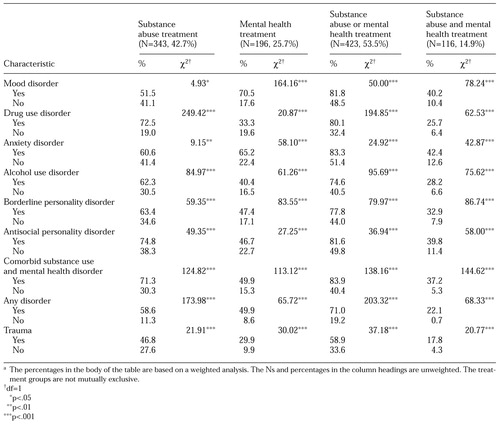 |
Table 2. Lifetime use of substance abuse and mental health treatment services among 805 recently incarcerated women prison inmates in North Carolina, by diagnostic and clinical characteristicsa
a The percentages in the body of the table are based on a weighted analysisThe Ns and percentages in the column headings are unweighted. The treatment groups are not mutually exclusive.
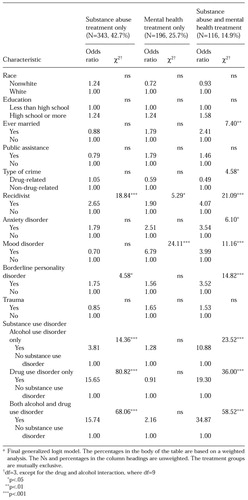 |
Table 3. Characteristics predicting lifetime substance abuse treatment or mental health treatment or both among 805 recently incarcerated women prison inmates in North Carolinaa
a Final generalized logit modelThe percentages in the body of the table are based on a weighted analysis. The Ns and percentages in the column headings are unweighted. The treatment groups are mutually exclusive.
 |
Table 4. Lifetime use of substance abuse and mental health treatment services among 805 recently incarcerated women prison inmates in North Carolina and 4,123 comparably aged women in the community, by diagnostic characteristics (in percentages)a
a The percentages in the body of the table are based on a weighted analysisThe Ns and percentages in the column headings are unweighted. The treatment groups are not mutually exclusive.
1. Criminal Offender Statistics, Women Offenders. Bureau of Justice Statistics and Activities at the National Archive of Criminal Justice Data Web site, accessed April 23, 2001. Available at www.icpsr.umich.edu/NACJD/bjs.html#csfacfGoogle Scholar
2. Bureau of Justice Statistics: Sourcebook of Criminal Justice Statistics Online, Nov 2000, accessed April 23, 2001. Available at www.albany.edu/sourcebookGoogle Scholar
3. National Institute of Justice: Drug Use Forecasting:1993 Annual Report. Washington, DC, US Department of Justice, 1993Google Scholar
4. Wellisch J, Prendergast ML, Anglin MD: Drug-Abusing Women Offenders: Results of a National Survey, Research in Brief. Washington, DC, National Institute of Justice, 1994Google Scholar
5. Snell TL: Survey of State Prison Inmates, 1991: Women in Prison, Bureau of Justice Statistics Special Report, NCJ-145321. Washington, DC, US Department of Justice, 1994Google Scholar
6. Research Advisory Services: Tabulation of a Nationwide Survey of Female Inmates, Prepared for the Task Force on the Female Offenders, Female Offender Survey Project. College Park, Md, American Correctional Association, May 1988Google Scholar
7. Friedman KO: Governor's Committee to Study Sentencing and Correctional Alternatives for Women Convicted of Crime: State of Maryland: Final Report. Annapolis, Md, General Assembly of Maryland, June 1988Google Scholar
8. Vlahov D, Brewer TF, Castro KG, et al: Prevalence of antibody to HIV-1 among entrants to US correctional facilities. JAMA 265:1129-1132, 1991Crossref, Medline, Google Scholar
9. Hankins CA, Gendron S, Handley MA, et al: HIV infection among women in prison: an assessment of risk factors using a nonnominal methodology. American Journal of Public Health 84:1637-1640, 1994Crossref, Medline, Google Scholar
10. Maruschak L: HIV in Prison and Jails, 1995. Bureau of Justice Statistics Bulletin NCJ-164260. Washington, DC, US Department of Justice, 1997Google Scholar
11. Owen B, Bloom B: Profiling women prisoners. Prison Journal 75:165-185, 1995Crossref, Google Scholar
12. Owen B: In the Mix. Albany, NY, State University of New York Press, 1998Google Scholar
13. Lord E: A prison superintendent's perspective on women in prison. Prison Journal 75:257-269, 1995Crossref, Google Scholar
14. Jordan BK, Schlenger WE, Fairbank JA, et al: Prevalence of psychiatric disorders among incarcerated women: II. convicted women felons entering prison. Archives of General Psychiatry 53:513-519, 1996Crossref, Medline, Google Scholar
15. Teplin LA, Abram KM, McClelland GM: Mentally disordered women in jail: who receives services? American Journal of Public Health 87:604-609, 1997Google Scholar
16. Farabee D: Substance Use Among Female Inmates Entering the Texas Department of Criminal Justice-Institutional Division:1994. Austin, Texas Commission on Alcohol and Drug Abuse, 1995Google Scholar
17. American Correctional Association Task Force on the Female Offender: The Female Offender: What Does the Future Hold? Laurel, Md, American Correctional Association, 1990Google Scholar
18. Little R, Rubin D: Statistical Analysis With Missing Data. New York, Wiley, 1987Google Scholar
19. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, rev. Washington, DC, American Psychiatric Association, 1987Google Scholar
20. World Health Organization: Composite International Diagnostic Interview (CIDI), Version 1.0. Geneva, World Health Organization, 1990Google Scholar
21. Robins LN, Wing J, Wittchen H-U, et al: The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry 45:1069-1077, 1988Crossref, Medline, Google Scholar
22. Robins LN, Helzer JE, Croughan J, et al: National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry 38:381-389, 1981Crossref, Medline, Google Scholar
23. Zanarini MC, Frankenburg FR, Chauncey DL, et al: The Diagnostic Interview for Personality Disorders: interrater and test-retest reliability. Comprehensive Psychiatry 28:467-480, 1987Crossref, Medline, Google Scholar
24. Robins LN, Regier DA (eds): Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, Free Press, 1991Google Scholar
25. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC, American Psychiatric Association, 1980Google Scholar
26. Resnick H, Falsetti S, Kilpatrick D, et al: Assessment of rape and other civilian trauma-related post-traumatic stress disorder, in Theory and Assessment of Stressful Life Events, 2nd ed. Edited by Miller TW. New York. International Universities Press, 1996Google Scholar
27. Agresti A: Categorical Data Analysis. New York, Wiley, 1990Google Scholar
28. Shah BV, Barnwell BG, Bieler GS: SUDAAN User's Manual: Release 7.0. Research Triangle Park, NC, Research Triangle Institute, 1996Google Scholar
29. Hodgins S, Lapalme M, Toupin J: Criminal activities and substance use of patients with major affective disorders and schizophrenia: a 2-year follow-up. Journal of Affective Disorders 55:187-202, 1999Crossref, Medline, Google Scholar
30. Gerstein DR, Datta AR, Ingels JS, et al: The national treatment improvement evaluation survey final report. Rockville, Md, Center for Substance Abuse Treatment, 1997Google Scholar
31. Estroff S: Now what? An analysis of recent reports on North Carolina's mental health services. Journal of Common Sense, Winter 2000/2001. Available at www.common-sense.org/pubications/journalGoogle Scholar
32. Gerstein DR, Johnson R: Prospective and retrospective studies of substance abuse treatment outcomes: methods and results of four large-scale follow-up studies. Rockville, Md, Center for Substance Abuse Treatment, 1999Google Scholar
33. Hubbard RL, Marsden ME, Rachal JV, et al: Drug Abuse Treatment: A National Study of Effectiveness. Chapel Hill, NC, University of North Carolina Press, 1989Google Scholar
34. Hoff RA, Baranosky MV, Buchanan BA, et al: The effects of a jail diversion program on incarceration: a retrospective cohort study. Journal of the American Academy of Psychiatry and the Law 27:377-386, 1999Medline, Google Scholar
35. Luettgen J, Chrapko WE, Reddon JR: Preventing violent re-offending in not criminally responsible patients: an evaluation of a continuity of treatment program. International Journal of Law and Psychiatry 21:89-98, 1998Crossref, Medline, Google Scholar
36. Harris GT, Rice ME: Mentally disordered offenders: what research says about effective service, in Impulsivity: Theory, Assessment, and Treatment. Edited by Webster CD, Jackson MA. New York, Guilford, 1997Google Scholar



