Converting Day Treatment Centers to Supported Employment Programs in Rhode Island
Abstract
>OBJECTIVE: The purpose of the study was to compare vocational and nonvocational outcomes of clients of two community mental health centers that underwent conversion from day treatment programs to supported employment programs with outcomes of clients of a center that delayed conversion until after the study was completed. METHODS: As part of a statewide effort in Rhode Island to convert day treatment programs to supported employment programs, the authors assessed 127 day treatment clients with severe mental illness in three community mental health centers. Two of the centers converted to supported employment, and one continued its rehabilitative day program. Participants were assessed prospectively for 30 to 36 months, with special attention to vocational and social outcomes. RESULTS: Former day treatment clients in the converted centers attained higher rates of competitive employment than those in the comparison group (44.2 percent and 56.7 percent versus 19.5 percent). Other employment outcomes also improved, and hospitalization rates and overall social functioning were unchanged. CONCLUSIONS: This study supports findings of previous studies suggesting that replacing rehabilitative day treatment programs with supported employment programs yields improvements in employment outcomes without adverse effects.
Historically, community mental health center services for clients with severe mental illness have been organized around the central structure of day treatment programs (1). The term "day treatment" has been used interchangeably with "partial hospitalization," which has been defined as "an ambulatory treatment program that includes the major diagnostic, medical, psychiatric, and prevocational treatment modalities designed for patients with serious mental disorders who require coordinated, intensive, comprehensive, and multidisciplinary treatment not provided in an outpatient clinic setting" (2).
Because partial hospitalization was mandated as an essential service in the Community Mental Health Center Act of 1963 (3), the number of such programs grew to exceed 1,000 nationwide by the 1980s (2). Originally developed as a cost-effective alternative to inpatient hospitalization (4,5,6), day treatment programs rapidly began to provide rehabilitative services rather than hospital diversion (3,7). In much of the United States, Medicaid reimbursement systems created incentives to provide day treatment services and to keep clients in them for long-term rehabilitative care. However, the research evidence indicates that day treatment does not rehabilitate clients in terms of helping them obtain jobs in the community (8). Furthermore, with the advent of managed care, the sizable costs of day treatment programs are coming under closer scrutiny (9,10).
Since the development of the community support program model in the 1970s (11), progressive state mental health systems throughout the United States have sought to increase the integration of persons with severe mental illness into the community. One factor that has facilitated the achievement of this goal has been the emergence of supported employment as an evidence-based practice and as a potential alternative to day treatment.
Supported employment refers to employment at prevailing wages in regular, integrated work settings with the provision of ongoing support services (12). Clients in supported employment typically work part-time in normal work settings with the same supervision, responsibilities, and wages as nondisabled workers. Thus supported employment is an alternative daytime activity that can replace day treatment. It can help fulfill consumers' desire to work, and it supports the goal of community integration. Results of early controlled studies of supported employment for persons with severe mental illness were promising, on average showing a threefold increase in rates of competitive employment (13). Recently these findings were reinforced by results from a multisite initiative (14). Managed care organizations, state departments of mental health, federal agencies, and advocacy groups are paying more attention to supported employment as an evidence-based practice for persons with severe mental illness (15,16,17).
A majority of persons with severe mental illness express the goal of participating in competitive employment (18). They prefer competitive employment to sheltered workshops (19), day treatment programs (20), and psychosocial rehabilitation programs (21). Unfortunately, vocational services are given low priority in most mental health systems. Both clients and family members identify employment as the highest-ranking unmet need (22,23). Less than 25 percent of clients with severe mental illness receive any form of vocational assistance (24,25,26), and community mental health centers devote only about 6 percent of their total budgets on average to vocational services (24). A recent five-state study found that a mere 2 percent of clients with severe mental illness were participating in supported employment programs (27).
Several studies have demonstrated the feasibility of converting day treatment programs to supported employment programs. In the first published study of such conversions (28), a New Hampshire community mental health center that eliminated its day treatment program because of budget cuts and replaced it with a small supported employment program was compared with a second site that continued its day treatment program along with traditional brokered vocational services. In the program that was converted to supported employment, clients' rate of competitive employment increased from 33 percent to 56 percent, whereas no change was seen for clients in the comparison program. Adverse outcomes—hospitalization, incarceration, homelessness, suicide attempts, or dropouts—did not increase among clients in the program that underwent conversion. Clients, their families, and mental health staff expressed high levels of satisfaction with the conversion (29). Subsequent studies of programs undergoing such conversions have reported similar results (30,31,32).
What remains to be shown is whether phasing out day treatment centers in favor of supported employment programs and other activities that involve community integration can be implemented systemwide. Several states are moving in this direction. Perhaps the best-planned demonstration is under way in Rhode Island, where a series of federal grants have been used to encourage the conversion of day treatment programs to supported employment (33). The Rhode Island effort involves collaboration among the Department of Mental Health, Retardation, and Hospitals, the Office of Rehabilitation Services, and the state Medicaid office to address organizational and financing issues. The effort is supported by meetings of stakeholders, including consumers and families, across the state to build consensus, and it includes state-funded supported employment training and economic incentives to replace lost Medicaid funds.
In this report we present data from the first step of the Rhode Island conversion process. We compared two community mental health center programs undergoing conversion with a third program that delayed conversion until after the study was completed. We hypothesized that competitive employment rates would increase among clients in the two programs undergoing conversion to supported employment, that adverse outcomes among these clients would not increase, and that their social activities would shift to contacts outside of the community mental health centers, whereas these measures would remain largely unchanged for clients in the comparison group.
Methods
We used a quasi-experimental design with two experimental programs that converted to supported employment and a comparison program that maintained day treatment with a stepped approach to vocational services. Participants were assessed at baseline and again at follow-up 30 to 36 months later; follow-up for clients in the converted programs took place 18 months after the conversion was completed. An independent research team conducted the interviews and evaluation.
Participants
Clients eligible for the study were those 18 to 65 years of age who had a severe mental disorder with prolonged disability, who had attended day treatment in one of three Rhode Island community mental health centers for at least eight days in the past six months, who were currently unemployed, who did not have any severe medical or cognitive impairment that would preclude employment and participation in the evaluation, and who provided informed consent.
Informational meetings with clients, families, and mental health providers were used to recruit participants for the study. Eligible clients gave informed consent before completing interviews. From the three centers, 127 of 170 eligible clients (74.7 percent) volunteered to participate in the evaluation. The participation rate did not differ across the three centers.
Complete vocational follow-up data were obtained for 114 of the 127 participants (89.8 percent). Their mean± SD age was 44.4±10.3 years; 58 (50.9 percent) were female, 93 (81.6 percent) were non-Hispanic white, and 48 (45.3 percent) had less than a high school education. Only one of the 114 was married. The majority had diagnoses of schizophrenia spectrum disorders (73, or 64 percent) or mood disorders (27, or 23.9 percent). Only a third (N=37) had worked in a competitive job at any time during the previous five years. Participants from the three community mental health center programs were similar in demographic, clinical, and vocational characteristics, with the exceptions of race and diagnosis. Program A, one of those undergoing conversion, had a larger proportion of nonwhite participants, mostly Hispanic (32.6 percent versus 20 percent and 2.4 percent; χ2=12.74, df=2), p<.01). Program B, the other conversion program, had a larger proportion of participants with schizophrenia spectrum disorders (83.3 percent versus 55.8 percent and 58.5 percent; χ2=11.90, df=2, p<.02).
Attrition was similar in the three programs. Of the 13 clients who were missing at follow-up, five had moved out of the area, four had died, two had been placed in nursing homes, one had been discharged, and one had been hospitalized soon after baseline and remained hospitalized throughout the follow-up period.
Programs
Three Rhode Island community mental health centers of similar size participated in the evaluation. Leaders of all three centers agreed to discontinue their day treatment programs and establish supported employment services, and administrators in center C agreed to delay their conversion and to serve as a comparison site for the initial evaluation. Thus center C continued its day treatment program three days a week and continued to offer vocational assistance that included supported employment as well as help in obtaining volunteer and sheltered workshop jobs. Center A provides services for persons in small mill cities and serves the largest Hispanic population in the state, and center B serves a suburban setting with the most affluent population of the three centers. Center C, the comparison site, is situated in the most rural of the study sites.
The conversion programs adopted a standardized approach to supported employment called individual placement and support (34). In this model, employment specialists join existing clinical teams to help interested clients find competitive jobs that match their interests and to coordinate long-term job support services offered by the team for clients who are working. The individual placement and support approach has been standardized by a manual (35), specific training procedures (36), and a fidelity scale (37). In studies in a variety of settings the model has produced consistently positive vocational outcomes (38).
The program conversions to supported employment followed a lengthy consensus-building process. After several months of discussions with staff, clients, and families about the principles and practices of supported employment, day treatment counselor positions were converted to employment specialist positions. The employment specialists and their supervisors received two days of supported employment training that included visits to mature programs. A vocational trainer provided weekly training sessions and supervision until the on-site supervisors were ready to take over. Fidelity ratings (37) were used to monitor implementation and to provide regular feedback to the teams and their supervisors about progress and areas for improvement. Both programs achieved ratings of good fidelity within 12 months.
Measures
Participants were assessed at baseline during the fall of 1995 and again 30 to 36 months later—18 months after complete conversion for the supported employment sites—by independent research interviewers using an interview that incorporated sections of several standardized instruments. Participants' demographic characteristics, clinical history, and housing situation were assessed with standardized questions from well-validated research interviews. The Employment and Income Review (39) was used to assess their work history, entitlements, and finances. The Global Assessment Scale (40) was used to rate participants' overall functional status, the expanded Brief Psychiatric Rating Scale (41) to assess symptoms, and the Rosenberg Self-Esteem Scale (42) to assess self-esteem.
To detect changes in social supports, we used the Quality of Life Interview (43), which assesses the number of and satisfaction with social contacts, in person or by telephone, and satisfaction with social relationships. We expanded the instrument to cover relationships with other consumers, with friends outside of the mental health system, with family, and with mental health staff, and we incorporated an overall rating, which was the total number of social contacts.
Participants' clinical diagnoses were obtained from community mental health center records. Center staff collected data weekly on hours and wages of competitive employment, which is defined by federal standards as work in the competitive job market at prevailing wages and supervised by personnel employed by the business.
Statistical analyses
We used one-way analysis of variance for continuous variables and chi square tests for discrete variables to examine the equivalence of the participants from the three programs at the baseline assessment point. Vocational outcomes during the postconversion period were analyzed with two-way analyses of variance with group (program A, B, or C) and work history, which was a dichotomous variable indicating whether the participant had been engaged in any work in the past five years, defined as between-subjects factors.
Because our primary hypothesis was that clients in the two programs that underwent conversion to supported employment would have better vocational outcomes than clients in the program that did not convert, we used a planned comparison to test the difference between programs A and B on the one hand and program C on the other. We also investigated group differences for nonvocational outcomes, which were assessed by interview at baseline and at follow-up 30 to 36 months later. We used repeated-measures multivariate analysis of variance, with group as the between-subjects factor and time—baseline versus follow-up—as the repeated measure, so that the interaction indicated program differences in change over time. We tested the planned comparison of programs A and B versus program C on the change scores derived from subtracting baseline from follow-up scores. The dichotomous outcome variable, employment versus no employment, was analyzed with a generalized linear mixed model using the SAS GLIMMIX macro (44).
Results
Vocational outcomes
Employment rates among clients in program C, the comparison program, held constant at about 5 percent each month, whereas rates among clients in the two programs that underwent conversion to supported employment climbed to rates between 15 percent and 35 percent per month after conversion. These monthly differences led to an overall difference in employment rates across the three centers during the study period, with higher rates for programs A (44.2 percent) and B (56.7 percent) than for program C (19.5 percent).
Table 1 presents the results for vocational outcomes. The main effects for both program and work history were significant for all employment outcomes, indicating that there were differences between programs and that persons who had worked during the previous five years had greater success than those who had not. Significant interactions for total hours and number of weeks of work are due to stronger effects of supported employment for clients who had not worked during the previous five years. That is, both groups improved, but clients who did not have a work history improved more than those who had. The planned comparisons were significant for the overall employment rate, total hours of work, and number of weeks of work and were nearly significant for total wages. Effect sizes for the planned comparisons varied from .23 to .61, with large effects for work history and weeks of work (45).
Nonvocational outcomes
As Table 2 shows, most of the tests of nonvocational outcomes were not statistically significant. No program differences, temporal changes, or interactions for symptoms, self-esteem, and hospitalization rates were detected. No program differences or time differences were detected for overall number of social contacts, but the interaction was significant. The mean number of social contacts increased for clients in program A, decreased for clients in program B, and stayed about the same for clients in program C. The planned comparison of programs A and B versus program C was not significant.
Examining social support with specific groups of other consumers, nonconsumer friends, family, and mental health staff (data not shown) revealed similar findings. The increase in mean number of social contacts for clients in program A, from 11.4 to 13.8 contacts per week, reflected increases in contacts with nonconsumer friends, family, and mental health staff. The decrease in overall contacts for clients in program B, from 15.5 to 11.2 contacts per week, was based on decreases in contacts with all four groups—consumers, nonconsumers, family, and staff. Nevertheless, no changes in satisfaction occurred with any of these changes in number of social contacts. The planned comparisons also were not statistically significant in any of these analyses.
Discussion
This study provides further evidence that day treatment programs in mental health settings can be converted to supported employment programs, providing strong benefits and carrying little risk. As in previous studies (28,29,30,31,32), clients in two routine mental health settings in Rhode Island were able to make the transition without untoward effects and, for many of the clients, with the benefit of vocational experiences in community work settings. The notable improvements in competitive employment outcomes in these conversions are all the more remarkable for the studies' inclusion of all day treatment clients, not just those who expressed interest in working or who signed up for employment services. In Rhode Island, as elsewhere, staff and clients noted the postconversion differences in terms of higher expectations and hopes for the future.
Although in our study no group changes were noted in symptoms, self-esteem, or quality of life, other research has shown that clients who are working in competitive employment or who become good workers benefit in nonvocational areas (46,47). These changes typically are not seen at the program level because many clients do not work at all or do not become consistent workers over time.
There is little evidence that rehabilitative day treatment—an expensive service—either promotes rehabilitation or protects clients from poor outcomes. Furthermore, it seems clear from interviews (19,20,21) and ethnographic studies (48,49,50) that clients experience day treatment as demeaning and would prefer competitive employment as an alternative. It may be that keeping people in segregated, low-expectation settings such as day treatment centers has the unintended effect of socializing them into disability, just as long-term hospitalization did earlier this century.
Findings on social outcomes from the Rhode Island project are less clear. Clients in both programs that underwent conversion to supported employment were encouraged to participate in existing social programs in the community to replace the social support offered previously by day treatment programs. Clients in program A reported more social contacts after the conversion, but clients in program B reported fewer.
The differences between the two programs could not be readily explained, even in follow-up interviews with staff and clients, who were unaware of any changes. One possibility is that the differences were not meaningful, particularly as clients in both conversion programs as well as in the comparison program did not become isolated and reported no change in satisfaction with their social supports. Other possibilities include measurement problems or factors the participants were unaware of. Social functioning should be explored further, because isolation and loneliness in the community are concerns often expressed by persons with severe mental illness and their families.
One caveat concerning the recent studies of day treatment closures is that they have all been in New England states known for having relatively well-funded and effective mental health programs. Closing day treatment programs in settings that lack a bedrock of competent clinical services may be considerably more difficult, just as closing hospitals has been problematic in states that lack adequate community-based services. This study was also limited by the particular characteristics of the community mental health centers involved, including small population size, high client motivation, and lack of racial diversity.
Conclusions
This study contributes to the literature showing that rehabilitative day treatment programs can be converted to supported employment programs with positive employment outcomes and without negative outcomes. Although clients generally appeared to be able to transfer social participation and maintain social satisfaction, this aspect requires further study.
Acknowledgments
This study was supported by National Institute of Disability and Rehabilitation Research grant 8133-G-50032 and National Institute of Mental Health grants MH-00839 and MH-00842; by the Rhode Island Department of Mental Health, Retardation, and Hospitals; by the Rhode Island Office of Rehabilitation Services; and by Community Counseling Center, East Bay Mental Health Center, and Mental Health Services. The authors thank Mike Braet, B.A., Kat Burrell, M.A., Bob Crossley, M.A., Ellen Heath, M.A., Carol Moser, R.N., M.S., Sandra Perez, B.A., Susan Ricketts, B.S., and Richard Toscano, M.Ed., for their help in conducting the research.
Ms. Becker, Dr. Xie, Dr. McHugo, and Dr. Drake are affiliated with the New Hampshire-Dartmouth Psychiatric Research Center, 2 Whipple Place, Lebanon, New Hampshire 03766 (e-mail, [email protected]). Dr. Bond is affiliated with the department of psychology at Indiana University-Purdue University Indianapolis. Mr. McCarthy and Mr. Thompson are affiliated with the Rhode Island Department of Mental Health, Retardation, and Hospitals.
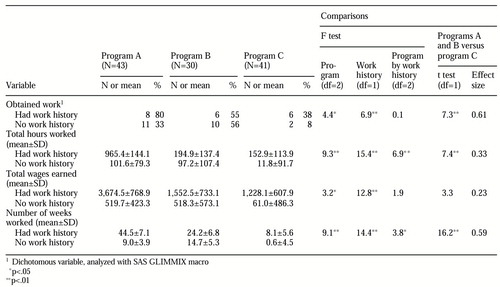 |
Table 1. Competitive employment outcomes among 114 participants during the two-year study period, by program and work history
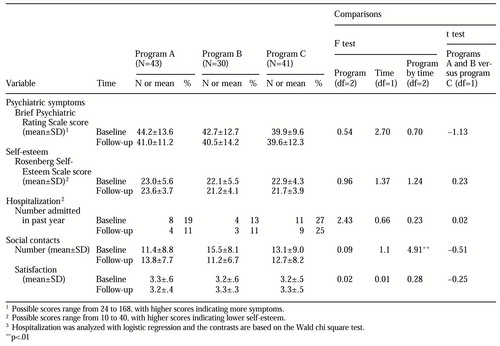 |
Table 2. Nonvocational outcomes among 114 participants during the two-year study period, by program and time
1. Krizay J: Partial hospitalization: facilities, cost, and utilization. Washington, DC, American Psychiatric Association, Office of Economic Affairs, 1989Google Scholar
2. Parker S, Knoll JL: Partial hospitalization: an update. American Journal of Psychiatry 147:156-160, 1990Link, Google Scholar
3. Rosie JS: Partial hospitalization: a review of recent literature. Hospital and Community Psychiatry 38:1291-1299, 1987Abstract, Google Scholar
4. Dick P, Cameron L, Cohen D, et al: Day and full-time psychiatric treatment: a controlled comparison. British Journal of Psychiatry 147:246-250, 1985Crossref, Medline, Google Scholar
5. Endicott J, Hertz MI, Gibbon M: Brief versus standard hospitalization: the differential costs. American Journal of Psychiatry 135:707-712, 1978Link, Google Scholar
6. Herz MI: Research overview in day treatment. International Journal of Partial Hospitalization 1:33-44, 1982Medline, Google Scholar
7. Casarino JP, Wilner M, Maxey JT: American Association for Partial Hospitalization (AAPH) standards and guidelines for partial hospitalization. International Journal of Partial Hospitalization 1:5-21, 1982Medline, Google Scholar
8. Hoge MA, Davidson L, Hill WL, et al: The promise of partial hospitalization: a reassessment. Hospital and Community Psychiatry 43:345-354, 1992Abstract, Google Scholar
9. Riggs RT: HMOs and the seriously mentally ill: a view from the trenches. Community Mental Health Journal 32:213-218, 1996Crossref, Medline, Google Scholar
10. McFarland BH: Ending the millennium: commentary on "HMOs and the seriously mentally ill: a view from the trenches." Community Mental Health Journal 32:219-222, 1996Crossref, Medline, Google Scholar
11. Turner JC, TenHoor WJ: The NIMH community support program: pilot approach to a needed social reform. Schizophrenia Bulletin 4:319-348, 1978Crossref, Google Scholar
12. Wehman P: Supported employment: toward zero exclusion of persons with severe disabilities, in Vocational Rehabilitation and Supported Employment. Edited by Wehman P, Moon MS. Baltimore, Brookes, 1988Google Scholar
13. Bond GR, Drake RE, Mueser KT, et al: An update on supported employment for people with severe mental illness. Psychiatric Services 48:335-346, 1997Link, Google Scholar
14. Carey MA: The continuing need for research on vocational rehabilitation programs. Psychosocial Rehabilitation Journal 18:163-164, 1995Crossref, Google Scholar
15. Manderscheid RW, Henderson MJ: Federal and state legislative and program directions for managed care, in Outcome Measurement in the Human Services: Cross-Cutting Issues and Methods. Edited by Mullen EJ, Magnabosco JL. Washington DC, NASW Press, 1997Google Scholar
16. National Advisory Mental Health Council, Clinical Treatment and Services Research Workgroup: Bridging Science and Service. Rockville, Md, National Institute of Mental Health, 1999Google Scholar
17. Flynn LM: Commentary. Schizophrenia Bulletin 24:30-32, 1998Google Scholar
18. Rogers ES, Walsh D, Masotta L, et al: Massachusetts Survey of Client Preferences for Community Support Services (final report). Boston, Boston University, Center for Psychiatric Rehabilitation, 1991Google Scholar
19. Bedell JR, Draving D, Parrish A, et al: A description and comparison of experiences of people with mental disorders in supported employment and paid prevocational training. Psychiatric Rehabilitation Journal 21:279-283, 1998Crossref, Google Scholar
20. Bond GR, Dietzen LL, McGrew JH, et al: Accelerating entry into supported employment for persons with severe psychiatric disabilities. Rehabilitation Psychology 40:91-111, 1995Crossref, Google Scholar
21. Hatfield AB: Serving the unserved in community rehabilitation programs. Psychosocial Rehabilitation Journal 13:71-82, 1989Google Scholar
22. Crane-Ross D, Roth D, Lauber BG: Consumers' and case managers' perceptions of mental health and community support service needs. Community Mental Health Journal 36:161-178, 2000Crossref, Medline, Google Scholar
23. Steinwachs DM, Kasper JD, Skinner EA: Family Perspectives on Meeting the Needs for Care of Severely Mentally Ill Relatives: A National Survey (final report). Baltimore, Johns Hopkins University, Center on the Organization and Financing of Care for the Severely Mentally Ill, 1990Google Scholar
24. Hollingsworth EJ, Sweeney JK: Mental health expenditures for services for people with severe mental illness. Psychiatric Services 48:485-490, 1997Link, Google Scholar
25. Leff HS, Wise M: Measuring service system implementation in a public mental health system through provider descriptions of employment service need and use. Psychosocial Rehabilitation Journal 18:51-64, 1995Crossref, Google Scholar
26. Lehman AF, Steinwachs DM: Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
27. Five State Feasibility Study on State Mental Health Agency Performance Measures. Prepared for the US Center for Mental Health Services. Alexandria, Va, National Association of State Mental Health Program Directors Research Institute, Inc, 1998.Google Scholar
28. Drake RE, Becker DR, Biesanz JC, et al: Rehabilitation day treatment vs supported employment: I. vocational outcomes. Community Mental Health Journal 30:519-532, 1994Crossref, Medline, Google Scholar
29. Torrey WC, Becker DR, Drake RE: Rehabilitative day treatment versus supported employment: II. consumer, family, and staff reactions to a program change. Psychosocial Rehabilitation Journal 18:67-75, 1995Crossref, Google Scholar
30. Drake RE, Becker DR, Biesanz JC, et al: Day treatment versus supported employment for persons with severe mental illness: a replication study. Psychiatric Services 47:1125-1127, 1996Link, Google Scholar
31. Bailey E, Ricketts SK, Becker DR, et al: Do long-term day treatment clients benefit from supported employment? Psychiatric Rehabilitation Journal 22:24-29, 1998Google Scholar
32. Gold M, Marrone J: Mass Bay Employment Services (a service of Bay Cove Human Services, Inc): a story of leadership, vision and action resulting in employment for people with mental illness, in Roses and Thorns From the Grassroots (spring). Boston, Institute of Community Action, 1998Google Scholar
33. McCarthy DD, Thompson D, Olson S: Planning a statewide project to convert day treatment to supported employment. Psychiatric Rehabilitation Journal 22:30-33, 1998Crossref, Google Scholar
34. Becker DR, Drake RE: Individual placement and support: a community mental health center approach to vocational rehabilitation. Community Mental Health Journal 45:487-489, 1994Google Scholar
35. Becker DR, Drake RE: A Working Life: The Individual Placement and Support (IPS) Program. Concord, NH, New Hampshire-Dartmouth Psychiatric Research Center, 1993Google Scholar
36. Becker DR, Torrey WC, Toscano R, et al: Building recovery-oriented services: lessons from implementing IPS in community mental health centers. Psychiatric Rehabilitation Journal 22:51-54, 1998Crossref, Google Scholar
37. Bond GR, Becker DR, Drake RE, et al: A fidelity scale for the individual placement and support model of supported employment. Rehabilitation Counseling Bulletin 40:265-284, 1997Google Scholar
38. Drake RE, Becker DR, Clark RE, et al: Research on the individual placement and support model of supported employment. Psychiatric Quarterly 70:289-301, 1999Crossref, Medline, Google Scholar
39. Improved Rehabilitation of Psychiatrically Disabled Individuals. NIDRR G0087-C0223-88. Boston, Boston University, Center for Psychiatric Rehabilitation, 1989Google Scholar
40. Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 33:766-771, 1976Crossref, Medline, Google Scholar
41. Lukoff D, Nuechterlein KH, Ventura J: Appendix A: manual for expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594-602, 1986Google Scholar
42. Rosenberg M: Society and the Adolescent Self-Image. Princeton, NJ, Princeton University Press, 1969Google Scholar
43. Lehman AF: The well-being of chronic mental patients. Archives of General Psychiatry 40:369-373, 1983Crossref, Medline, Google Scholar
44. Little R, Milliken G, Stroup W, et al: SAS System for Mixed Models. Cary, NC, SAS Institute, Inc, 1996Google Scholar
45. Lipsey MW: Design Sensitivity. Newbury Park, Calif, Sage, 1990Google Scholar
46. Bond GR, Resnick SG, Drake RE, et al: Does competitive employment improve nonvocational outcomes for people with severe mental illness? Journal of Consulting and Clinical Psychology, in pressGoogle Scholar
47. Mueser KT, Becker DR, Torrey WC, et al: Work and nonvocational domains of functioning in persons with severe mental illness: a longitudinal analysis. Journal of Nervous and Mental Disease 185:419-426, 1997Crossref, Medline, Google Scholar
48. Estroff S: Making It Crazy: An Ethnography of Psychiatric Clients in an American Community. Berkeley, University of California Press, 1981Google Scholar
49. Alverson M, Becker DR, Drake RE: An ethnographic study of coping strategies used by people with severe mental illness participating in supported employment. Psychosocial Rehabilitation Journal 18:115-128, 1995Crossref, Google Scholar
50. Quimby E, Drake RE, Becker DR: Ethnographic findings from the Washington, DC, vocational services study. Psychiatric Rehabilitation Journal, in pressGoogle Scholar



