Association Between Interruptions in Medicaid Coverage and Use of Inpatient Psychiatric Services
Abstract
OBJECTIVES: Persons with schizophrenia are heavy and persistent users of Medicaid services. Interruptions in their Medicaid coverage may have serious consequences for the mental health of these individuals and their subsequent use of mental health services. This study sought to determine the impact of interruptions in Medicaid coverage on the use of Medicaid-reimbursed inpatient psychiatric services over a four-year period. METHODS: Inpatient Medicaid claims and eligibility files for 1,830 Medicaid beneficiaries with schizophrenia in Utah from December 1990 to December 1994 were used to identify differences in hospital admissions and total number of days in a hospital associated with interrupted Medicaid coverage. Of the 1,830 Medicaid beneficiaries identified, 1,463 experienced continuous Medicaid eligibility, and 367 had interruptions in their eligibility. RESULTS: Interruptions in Medicaid coverage were associated with an average of .63 more psychiatric hospitalizations per beneficiary over the four-year period, representing an 86 percent higher hospital admission rate. This increase appeared to be largely due to a subset of persons who have much higher hospitalization rates after an interruption in Medicaid coverage. Interruptions in Medicaid coverage were associated with a mean of 8.3 more days of psychiatric hospitalization over the four-year period, representing 61 percent more hospital days. CONCLUSIONS: Medicaid beneficiaries who experience interruptions in coverage have, on average, a significantly greater use of inpatient psychiatric services while participating in Medicaid than beneficiaries with continuous Medicaid coverage. These findings suggest potential benefits of maintaining continuous Medicaid eligibility for beneficiaries with a severe mental illness.
Schizophrenia is a severe and chronic disease that afflicts about 1 percent of the population. The disease is characterized by episodes of acute psychosis followed by periods of remission recurring throughout an individual's lifetime (1). Because of the chronic nature of schizophrenia, continuous maintenance treatment is necessary (2,3,4,5,6,7). The ability of persons with schizophrenia to maintain continuous care is in part related to their ability to pay for services.
The Medicaid program is the largest source of federal support for the care of persons with severe mental illness (8), and it is typically the primary source of funding for care for such persons. Some individuals may also have Medicare coverage because of their disability, but coverage for outpatient mental health services under Medicare is limited and is subject to a 50 percent rate of coinsurance. In addition, Medicare does not cover prescription drugs. State funding for mental health care is usually available to this population, but the services are often limited. Thus if a person with severe mental illness experiences an interruption in Medicaid coverage, access to mental health care will likely be affected during this period, leading to discontinuity in treatment. Discontinuity in treatment during periods of interrupted coverage may adversely affect the person's mental health status and increase the probability that expensive psychiatric hospitalizations will be necessary. Such hospitalizations in turn often trigger the renewal of Medicaid coverage to cover the cost of inpatient care.
Although the causes of interrupted Medicaid coverage are not known, two scenarios are likely. One is that the person's mental health status improves, permitting the person to secure employment. Because of the additional income, the person may no longer qualify for Medicaid. Under this scenario, the employed individual may receive no health insurance benefits or may have private insurance that is less comprehensive than Medicaid, especially for coverage of expensive psychotropic medications. Interruptions in Medicaid coverage could also be the result of worsening mental health status. Under this scenario, the beneficiary becomes too ill to complete the paperwork required to maintain Medicaid coverage. Such individuals may lose contact with the mental health care system precisely because of their worsening mental health status.
To our knowledge, no published studies have examined the effects of interruptions in Medicaid coverage in either the general health or the mental health sector. In a study of the effect of gaps in health insurance in general on continuity of care for young children, Kogan and associates (9) found that children with gaps in insurance were less likely to receive preventive care and were more likely to delay care and require hospitalization if they were seen in an emergency department. Several studies have examined the effect of loss of Medicaid coverage on access to and use of health care and on health status. These studies showed that loss of Medicaid coverage results in decreased access to care and worse general health (10,11,12).
In the study reported here, we used data from Medicaid claims to assess whether interruptions in Medicaid coverage for beneficiaries with schizophrenia were associated with differences in admission rates for Medicaid-reimbursed psychiatric hospitalizations and in the number of days patients were hospitalized.
Methods
Sample
The data were collected as part of an evaluation of the Utah Prepaid Mental Health Plan. This study was approved by the institutional review board of the University of Minnesota. Under the Utah Prepaid Mental Health Plan, community mental health centers provided mental health services to all Medicaid beneficiaries in a given catchment area in exchange for a capitated payment. Medicaid beneficiaries who were not served by community mental health centers under contract with the Utah Prepaid Mental Health Plan received usual care. Descriptions of the Utah Prepaid Mental Health Plan and of the evaluation are published elsewhere (13,14,15,16,17,18,19). Receiving services at community mental health centers that were contract sites of the Utah Prepaid Mental Health Plan was associated with more use of case management services (19) and fewer expenditures for inpatient psychiatric services (18) compared with receiving services at a noncontract site.
For the analyses reported here, we used data from Utah Medicaid beneficiaries with schizophrenia who were identified by using an algorithm based on diagnostic codes in Medicaid claims covering the period from July 1988 through November 1990 (20). A total of 1,915 Medicaid beneficiaries who had either one inpatient admission or two outpatient claims with a primary diagnosis of schizophrenia were selected.
Individuals were identified as having had an interruption in Medicaid if they experienced two or more continuous months without coverage, followed by renewed coverage, during the period from December 1990 through December 1994. Any periods without Medicaid coverage that were experienced at the end of the study period were excluded from the analyses, because no utilization data were available for these periods.
Of the 1,915 persons identified as having schizophrenia from July 1988 through November 1990, a total of 367 experienced interruptions in Medicaid coverage of at least two months during the 49-month study period from December 1990 through December 1994, a total of 1,463 experienced continuous coverage, and 85 were not covered at any time during the study period. Of those with continuous coverage, 1,125 (78 percent) were covered for the entire 49-month study period and 338 (22 percent) were not covered for at least one month at the end of the study period. Data for persons with a noncovered episode at the end of the study period were included in the analysis, but their utilization was modeled only for the period of continuous coverage, with exposure time—that is, the number of months of Medicaid coverage—controlled for.
In the group of persons with continuous coverage, the mean±SD number of months of continuous coverage was 43.5±12.1. For the 367 individuals with interruptions in Medicaid, the average number of interruptions was 1.3. The average duration of each period of coverage was 15.8 months, and the average duration of each interruption was 9.9 months. Of the 367 individuals with interruptions, 290 had one interruption, 65 had two interruptions, eight had three interruptions, three had four interruptions, and one had five interruptions.
Variables
The number of hospitalization episodes and the number of days in the hospital were determined by using beginning dates and ending dates of the episodes in the Medicaid claims data. The number of psychiatric hospitalizations was obtained by summing the number of unique hospitalization episodes for each individual over the 49-month study period. The distribution of the total number of hospitalizations in the study sample is presented in Table 1. For comparison purposes, the number of hospitalizations that occurred before an interruption in Medicaid coverage and the number of hospitalizations that occurred after an interruption were calculated.
The total number of days of psychiatric hospitalization was computed by summing the length of stay for each episode of inpatient psychiatric care for an individual patient during the study period. The distribution of the number of days of psychiatric hospitalization in the study sample is presented in Table 2. For comparison purposes, the number of days before an interruption in Medicaid coverage and the number of days after an interruption were calculated as well.
Statistical methods
The main purpose of the statistical analysis was to answer the following question: What would the use of Medicaid-reimbursed inpatient psychiatric services for persons with interruptions in coverage have been if they had instead experienced continuous Medicaid coverage over the same period?
Number of psychiatric hospitalizations. The association of interruptions in Medicaid coverage with the number of psychiatric hospitalizations over the 49-month study period was analyzed by using negative binomial regression (21,22,23). By using this method, the total number of Medicaid-reimbursed psychiatric hospitalizations was modeled as a function of the duration of the interruption in Medicaid coverage, sex, race, urban residence, participation in the Utah Prepaid Mental Health Plan, age, calendar year of eligibility, and total months of Medicaid coverage.
The effect of interruptions in Medicaid coverage was analyzed by comparing the mean number of psychiatric hospitalizations for individuals with interruptions in coverage, adjusted for the covariates, including the total number of months of Medicaid coverage, with the estimated mean number of psychiatric hospitalizations that would have occurred if those same individuals had instead experienced continuous coverage. The adjusted mean of the total number of hospitalizations for the 367 beneficiaries with interruptions in coverage was determined by using the regression model. Then the total number of hospitalizations that would have occurred if the 367 beneficiaries had experienced continuous Medicaid coverage was estimated by resetting the length-of-interruption variable to zero and redoing the regression analysis with the new time at risk. The new time at risk was equal to the original time at risk for these beneficiaries plus the number of months that Medicaid coverage was interrupted.
This model did not distinguish between hospitalizations that took place before or after an interruption in coverage. If a majority of hospitalizations took place before an interruption in coverage or if individuals with interruptions in coverage were more likely to have a history of psychiatric hospitalizations, the results could be biased because an effect on psychiatric hospitalizations could be attributed to interruptions in Medicaid coverage. To examine this possible source of bias, we compared the rate of hospitalizations before and after an interruption in coverage. Ideally, we would have presented the results of a sensitivity analysis based on a negative binomial regression model, but the sample was too small for this type of analysis.
Number of days of psychiatric hospitalization. The association of interruptions in Medicaid with the total number of hospital days was examined by using an exponential regression model (24,25). We assumed that the log of the mean number of hospital days was a function of the patients' characteristics, including whether they had an interruption in Medicaid coverage.
The effect of interrupted Medicaid coverage on the number of hospital days was determined by comparing the mean length of stay for persons with interruptions in Medicaid coverage, adjusted for age, sex, race, the number of months of Medicaid eligibility, and other factors, to the mean length of stay assuming continuous Medicaid coverage, as described above. We examined the total number of days in the hospital per month before and after an interruption in Medicaid coverage to see whether the rate increased after a period of interrupted coverage. The sample was not large enough for a regression model to be estimated to determine the statistical significance of any difference in hospital days after an interruption in Medicaid coverage.
Results
The unadjusted means for all variables for the group with continuous coverage and the group with interrupted coverage are presented in Table 3.
Number of psychiatric hospitalizations
The results of the regression analysis are presented in Table 4. The duration of the interruption in Medicaid coverage, age, race, participation in the Utah Prepaid Mental Health Plan, and the year of eligibility were significant predictors of the number of hospitalizations. With adjustment for the covariates, 51.5 percent of the 367 individuals with interrupted coverage had at least one hospitalization, but only 38.3 percent of those same 367 individuals were predicted to have had at least one hospitalization if they had instead experienced continuous coverage, a 35 percent difference (z=6.9, p<.001). The adjusted mean number of hospitalizations for persons with interruptions in Medicaid coverage was 1.36, and the adjusted mean number of hospitalizations assuming continuous Medicaid coverage was .73, a difference of .63 hospitalizations (z=8.4, p<.001), or 86 percent.
These findings were supported when the hospitalization rate—that is, the mean number of hospitalizations per month—before an interruption in coverage was compared with the rate after an interruption in coverage. Before an individual's first interruption in coverage, the unadjusted rate was .035 hospitalizations per month, compared with .045 hospitalizations per month after the interruption in coverage, a 28 percent difference. Also, approximately 30 percent of all hospitalizations occurred in the two-month period after an interruption in Medicaid coverage. However, more individuals had a lower hospitalization rate after the interruption (85 individuals) than had a higher hospitalization rate after the interruption (52 individuals), but the 52 individuals with the higher rates accounted for a higher total number of hospitalizations after the interruption than the individuals with the lower rate. Thus the mean increase in hospitalizations associated with having an interruption in Medicaid coverage appeared to be due to the occurrence of a large effect in a subset of the population who experienced interruptions in coverage.
Number of days of psychiatric hospitalization
The results of the regression analysis for the total number of hospital days are presented in Table 4. The duration of the interruption in Medicaid coverage, age, race, urban residence, participation in the Utah Prepaid Mental Health Plan, and the year of eligibility were significant predictors of total hospital days. Individuals with an interruption in coverage spent a mean of 21.9 days in the hospital during the 49-month study period, but those same individuals would have spent a mean of only 13.6 days in the hospital if they had had continuous coverage, a difference of 8.3 days (z=7.1, p<.001), or 61 percent.
These findings were supported when the number of hospital days per month before an interruption in coverage was compared with the number of days per month after an interruption. Before the first interruption in coverage, individuals spent a mean of .56 days in the hospital per month, compared with .64 days per month after an interruption in coverage, a 14 percent difference. A total of 83 individuals had more hospital days per month after an interruption in coverage, and 58 had fewer hospital days after an interruption in coverage.
Overall, the analysis suggested that use of inpatient psychiatric services was greater for patients with interruptions in Medicaid coverage than for those without interruptions. Although the analyses that incorporated the timing of hospitalizations did not show an overwhelming effect, the numbers of hospitalizations and hospital days per month before and after an interruption in Medicaid coverage clearly showed that a majority of hospitalizations did not take place before an interruption in Medicaid coverage. The results of additional analyses of the timing of outpatient services and pharmacy claims and an analysis of data from a subset of the sample that accounted for baseline mental health status are available from the first author on request.
Discussions and conclusions
The results of this study, summarized in Table 5, suggest that interruptions in Medicaid coverage are associated with greater use of inpatient psychiatric services. On average, each individual beneficiary with schizophrenia who experiences interruptions in Medicaid coverage may spend up to eight extra days in an inpatient psychiatric facility over a four-year period. This increase appears to be due to a large effect in a subset of the population. Although Medicaid programs may attempt to save money by restricting coverage, this strategy may not result in cost savings in this population, because loss of coverage may lead to expensive psychiatric hospitalizations that result in reinstatement of coverage to cover the cost of the hospitalization.
A logical solution to the problem created by interruptions in Medicaid coverage would be a reexamination of Medicaid eligibility policies for persons with chronic disabilities (including schizophrenia), a history of hospitalization, or both. Changes in such policies could help address the cases of persons who lose eligibility because their mental health improves, allowing them to obtain employment and an income that exceeds the limits for Medicaid eligibility. Assuming that universal health insurance with a prescription drug benefit is not politically likely, continuing Medicaid eligibility through a Medicaid buy-in program might enable such individuals to remain in the workforce while also maintaining their access to mental health care and avoiding clinical decompensation.
To address interruptions in coverage that are the result of worsening mental health status, state Medicaid programs might consider steps to enable individuals to more easily maintain their Medicaid coverage, such as instituting annual renewal of Medicaid coverage instead of monthly renewal, which was required in Utah at the time of the study. Such steps might reduce the frequency of interruptions and the cost of administering Medicaid benefits. However, this approach assumes that simply maintaining Medicaid coverage will ensure that individuals will seek out care from mental health providers, which may not be the case.
The type of Medicaid eligibility may also play a role in the likelihood of experiencing an interruption in coverage. For example, persons who are eligible for Medicaid because they receive Supplemental Security Income may be less likely to experience an interruption in coverage than those who are eligible through the Aid to Families With Dependent Children or Temporary Assistance for Needy Families programs. Unfortunately, with the available data, we could not determine the causes of interruptions in coverage or the eligibility categories of the beneficiaries in the study.
The effect of interruptions in Medicaid coverage may be confounded by unmeasured characteristics. For example, persons with interruptions may be more likely to be noncompliant with their medication regimen or more likely to have substance use problems, both of which have been shown to be associated with higher rates of relapse and higher rates of inpatient service use. Persons who experienced interruptions in coverage had a significant drop in both outpatient visits and pharmacy claims in the two months preceding the interruption (data available from the first author), which suggests that persons who are noncompliant with treatment may be more likely to experience interruptions in coverage. If these individuals are more likely to experience interruptions in coverage, policies that provide ongoing case management to these at-risk populations might help stabilize their coverage and might still save states money in the long run.
The total number of hospitalizations and total number of days in the hospital were significantly less for persons who received services through the Utah Prepaid Mental Health Plan. If Medicaid programs are seeking to decrease costs, reducing the use of inpatient services through mechanisms such as the Utah Prepaid Mental Health Plan and additional case management may be a better solution than trying to reduce service use by limiting Medicaid coverage. However, we found no difference in the probability of having an interruption in Medicaid coverage between beneficiaries who received services through the Utah Prepaid Mental Health Plan and those who did not, which suggests that capitation alone does not decrease the frequency of interruptions in Medicaid coverage.
Beneficiaries also may experience an interruption in coverage if they are hospitalized in a state psychiatric hospital for an extended period, but this occurrence was relatively rare. Regardless of the reason for the interruptions in coverage, the results of this study suggest that individuals whose coverage is interrupted may use more inpatient mental health services than they would have used if their coverage had been continuous. Additional research is needed to validate these findings and to explore the causes of interruptions in Medicaid coverage so that potential solutions to this problem can be developed.
A few other limitations of this study should be noted. This research examined the association of interruptions in Medicaid coverage with the use of Medicaid-reimbursed inpatient psychiatric services and did not test whether interruptions in Medicaid led directly to the inpatient episode. Sensitivity analyses that incorporated the timing of hospitalization could not be conducted, because the sample was too small, but the data suggested that findings from the main set of analyses were not due to high rates of hospitalization before interruptions in Medicaid coverage. Other limitations include the lack of data on the use of services during the interruption periods and on use of services that were not paid for by Medicaid, lack of measures of mental health status and other potential confounding factors for all beneficiaries, and lack of information on the causes of interruptions in coverage. Nevertheless, the results of this study serve as a starting point for further investigation of the causes and effects of interruptions in Medicaid among persons with severe mental illness.
Acknowledgments
This work was supported by grant MH-58025 from the National Institute of Mental Health. The authors thank the staff of the health care financing division of the Utah Department of Health and the staff of the community mental health centers in Utah.
Dr. Harman is affiliated with the department of health services administration at the University of Florida in Gainesville and with Western Psychiatric Institute and Clinic in Pittsburgh. Dr. Manning is with the department of health studies at the University of Chicago. Dr. Lurie is with the RAND Corporation in Arlington, Virginia. Dr. Christianson is with the department of healthcare management at the University of Minnesota in Minneapolis. Address correspondence to Dr. Harman at the Department of Health Services Administration, University of Florida, P.O. Box 100195, Gainesville, Florida 32611-0195 (e-mail, [email protected]). An earlier version of this paper was presented at the annual meeting of the Association for Health Services Research held June 15 to 17, 1998, in Chicago.
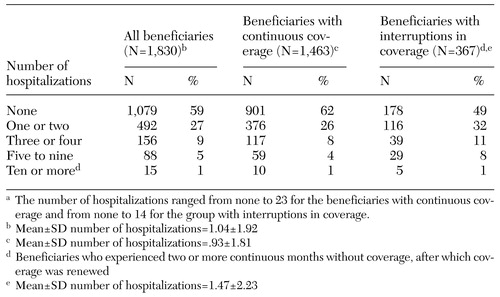 |
Table 1. Total number of inpatient psychiatric hospitalizations of Utah Medicaid beneficiaries with schizophrenia with continuous or interrupted Medicaid coverage over a 49-month period (December 1990 through December 1994)a
a The number of hospitalizations ranged from none to 23 for the beneficiaries with continuous coverage and from none to 14 for the group with interruptions in coverage.
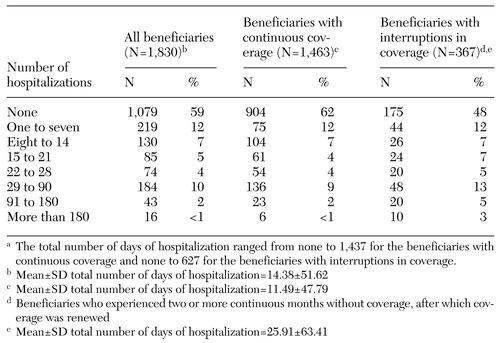 |
Table 2. Total number of days of inpatient psychiatric hospitalization of Utah Medicaid beneficiaries with schizophrenia with continuous or interrupted Medicaid coverage over a 49-month period (December 1990 through December 1994) a
a The total number of days of hospitalization ranged from none to 1,437 for the beneficiaries with continuous coverage and none to 627 for the beneficiaries with interruptions in coverage.
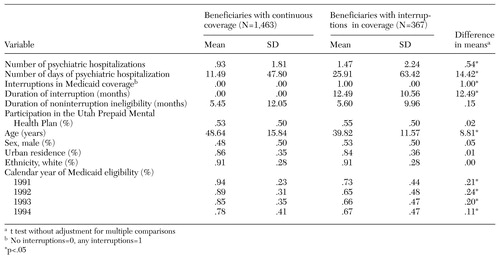 |
Table 3. Mean values for variables assessed in a study of effects of interruptions in Medicaid coverage among Utah Medicaid beneficiaries with schizophrenia over a 49-month period (December 1990 through December 1994)
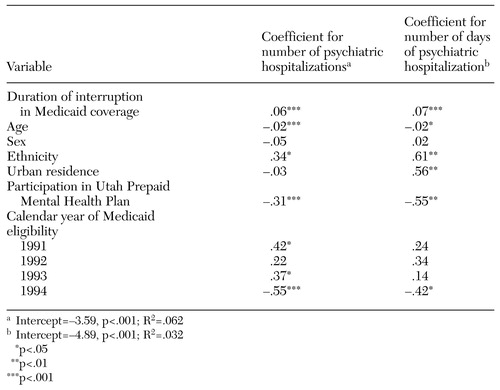 |
Table 4. Regression analysis of variables assessed in a study of effects of interruptions in Medicaid coverage among 1,830 Utah Medicaid beneficiaries with schizophrenia over a 49-month period (December 1990 through December 1994)
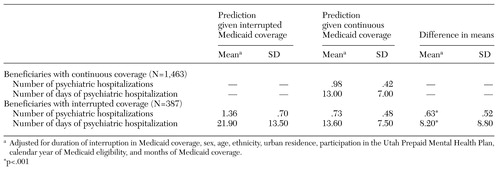 |
Table 5. Predicted number of psychiatric hospitalizations and number of days of psychiatric hospitalization associated with interrupted and continuous Medicaid coverage among 1,830 Utah Medicaid beneficiaries with schizophrenia over a 49-month period (December 1990 through December 1994)
1. Carpenter WT Jr, Buchanan RW: Schizophrenia. New England Journal of Medicine. 330:681–690, 1994Google Scholar
2. Stein LI: A system approach to reducing relapse in schizophrenia. Journal of Clinical Psychiatry 54(suppl):7–12, 1993Medline, Google Scholar
3. Bellack AS, Mueser KT: Psychosocial treatment for schizophrenia. Schizophrenia Bulletin 19:317–336, 1993Crossref, Medline, Google Scholar
4. Bellack AS, Mueser KT: A comprehensive treatment program for schizophrenia and chronic mental illness. Community Mental Health Journal 22:175–189, 1986Crossref, Medline, Google Scholar
5. Vaccaro JV, Young AS, Glynn S: Community-based care of individuals with schizophrenia: combining psychosocial and pharmacologic therapies. Psychiatric Clinics of North America 16:387–399, 1993Crossref, Medline, Google Scholar
6. Dworkin RJ, Adams GL, Telschow RL: Cues of disability and treatment continuation of chronic schizophrenics. Social Science and Medicine 22:521–526, 1986Crossref, Medline, Google Scholar
7. Bachrach LL: Continuity of care for chronic mental patients: a conceptual analysis. American Journal of Psychiatry 138:1449–1456, 1981Link, Google Scholar
8. Steinwachs DM, Cullum HM, Dorwart RA, et al: Service systems research. Schizophrenia Bulletin 18:627–668, 1992Crossref, Medline, Google Scholar
9. Kogan MD, Alexander GR, Teitelbaum MA, et al: The effect of gaps in health insurance on continuity of a regular source of care among preschool-aged children in the United States. JAMA 274:1429–1435, 1995Crossref, Medline, Google Scholar
10. Lurie N, Ward NB, Shapiro MF, et al: Termination from Medi-Cal: does it affect health? New England Journal of Medicine 311:480–484, 1984Google Scholar
11. Lurie N, Ward NB, Shapiro MF, et al: Termination of Medi-Cal benefits: a follow-up study one year later. New England Journal of Medicine 314:1266–1268, 1986Crossref, Medline, Google Scholar
12. Brown ER, Cousineau MR: Loss of Medicaid and access to health services. Health Care Financing Review 12(4):17–26, 1991Google Scholar
13. Christianson JB, Gray DZ, Kihlstrom LC, et al: Development of the Utah Prepaid Mental Health Plan. Advances in Health Economics and Health Services Research 15:117–135, 1995Medline, Google Scholar
14. Christianson JB, Gray DZ: What CMHCs can learn from two states' efforts to capitate Medicaid benefits. Hospital and Community Psychiatry 45:777–781, 1994Abstract, Google Scholar
15. Christianson JB, Manning W, Lurie N, et al: Utah's prepaid mental health plan: the first year. Health Affairs 14(3):160–172, 1995Google Scholar
16. Manning WG, Liu CF, Stoner T, et al: Outcomes for Medicaid beneficiaries with schizophrenia under a prepaid mental health carve-out. Journal of Behavioral Health Services Research 26:442–450, 1999Crossref, Medline, Google Scholar
17. Liu CF, Manning WG, Christianson JB, et al: Patterns of outpatient use of mental health services for Medicaid beneficiaries under a prepaid mental health carve-out. Administration and Policy in Mental Health 26:401–415, 1999Crossref, Medline, Google Scholar
18. Stoner T, Manning W, Christianson J, et al: Expenditures for mental health services in the Utah Prepaid Mental Health Plan. Health Care Financing Review 18(3):73–93, 1997Google Scholar
19. Popkin MK, Lurie N, Manning W, et al: Changes in the process of care for Medicaid patients with schizophrenia in Utah's Prepaid Mental Health Plan. Psychiatric Services 49:518–523, 1998Link, Google Scholar
20. Lurie N, Moscovice I, Popkin M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69–71, 1992Abstract, Google Scholar
21. Lawless JF: Negative binomial and mixed Poisson regression. Canadian Journal of Statistics 15:209–225, 1987Crossref, Google Scholar
22. Gardner W, Mulvey EP, Shaw EC: Regression analysis of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological Bulletin 118:392–404, 1995Crossref, Medline, Google Scholar
23. Cameron AC, Trivedi PK: Econometric models based on count data: comparisons and applications of some estimators and tests. Journal of Applied Econometrics 1:29–53, 1986Crossref, Google Scholar
24. McCullagh P, Nelder JA: Generalized Linear Models, 2nd ed. New York, Chapman and Hall, 1989Google Scholar
25. Blough DK, Madden CW, Hornbrook MC: Modeling risk using generalized linear models. Journal of Health Economics 18:153–171, 1999Crossref, Medline, Google Scholar



