Disparities in Use of Mental Health and Substance Abuse Services by Persons With Co-occurring Disorders
A pervasive concern about treating persons with co-occurring mental and substance use disorders is whether they receive treatment for both disorders. This is a significant problem in that persons with co-occurring disorders represent from 49% to over 60% of persons in treatment settings. ( 1 , 2 , 3 ). Several important population-based surveys ( 2 , 3 , 4 , 5 , 6 , 7 ) have found that most persons in need of mental health care or substance abuse treatment services or both do not get specialty treatment for these disorders. Lack of treatment seems to be worse for persons with co-occurring mental and substance use disorders. The 2005 National Survey on Drug Abuse and Health ( 8 ) found that more than half of the adults with co-occurring disorders did not receive specialty mental health care or substance abuse treatment during the prior 12 months.
In many locales, one problem in obtaining services is that the mental health and substance abuse treatment systems are segregated and have separate funding streams ( 9 , 10 , 11 ). Persons with co-occurring disorders frequently need to navigate two systems of care to obtain treatment, and those who receive treatment in one sector may not receive adequate treatment in the other sector ( 9 , 12 ).
Despite population-based and organizational studies concerning use of mental health and substance abuse treatment systems, there is a dearth of empirical information about whether persons with co-occurring disorders navigate between the two systems to obtain care ( 9 ). Also, it is not known whether one system of care is more advantageous than the other in terms of facilitating treatment for both disorders. Typically, clinical studies of persons with co-occurring disorders focus on one system of care only, which may provide an incomplete perspective on treatment utilization ( 13 ).
The primary study objective was to address these gaps in knowledge by examining differences in the likelihood and amount of services received in the mental health care and substance abuse treatment systems by persons with co-occurring disorders during the 24-month period after entering treatment. Participants were recruited concomitantly from either mental health crisis residential programs or substance abuse crisis residential detoxification programs in San Francisco. We found no other investigations in the literature that used this methodology.
In our earlier descriptive work ( 14 ), we found that participants with co-occurring disorders recruited from the two systems had many similarities, including DSM-IV diagnoses. On the basis of these similarities, we anticipated that there would be minimal differences in service use patterns between groups after controlling for demographic and clinical factors found to be predictors of service use.
Methods
Recruitment procedures
Recruitment sites were three mental health crisis residential programs in the public-sector mental health system and four substance abuse residential detoxification programs. These programs represented all of the programs of these types in San Francisco during the recruitment period (1999–2001). The programs were primary points of entry into treatment and were expected to provide short-term care to stabilize clients and then to refer them to longer-term treatments.
Participants
Clinic staff at the recruitment locations informed the research assistants about new entrants. Recruitment at each of the programs was conducted on one randomly selected day per week to avoid potential bias from weekly variation in program entry. On each recruitment day, research assistants approached entrants admitted in the previous 24 hours and attempted to recruit those clients. The study was explained to interested clients. Clients who could not be approached and recruited within 72 hours of treatment entry were no longer considered for study participation. Research assistants read and reviewed the consent form with interested potential participants. Those who agreed to participate provided written informed consent. All procedures were approved by the University of California, San Francisco, Institutional Review Board.
Inclusion criteria
Clients who were 18 to 50 years of age, who spoke English or Spanish, who had public insurance (Medi-Cal, Medicare, or both) ( 15 ) or no health insurance, who were not HIV positive, who had verifiable contact information to assist with follow-up, and who were able to provide informed consent were eligible to participate. Clients with private insurance were excluded because of their greater access to care than those without. Documented HIV-positive clients were not enrolled in the study because they had access to specialized services. Clients who could not provide at least one verifiable contact for follow-up and those planning to leave San Francisco within the year were also excluded because of the anticipated loss of follow-up information. Intake interviews, including a comprehensive diagnostic assessment, were conducted within 72 hours of admission.
A total of 1,484 clients were identified as new entrants and potentially eligible for the study. Of this group, 537 (36%) were found to be ineligible, 377 (25%) refused participation, and 570 (38%) provided informed consent. Of those providing informed consent, 476 participants (84% of 570) completed the intake assessment battery and 420 (74%) provided useable diagnostic data. Of these 420, a total of 226 participants had co-occurring diagnoses, and of them, 224 had utilization data from the billing-information systems. The 224 composed the study sample: 118 participants from substance abuse and 106 from mental health settings. A total of 54 clients who did not provide usable data consisted of 21 persons who had no diagnoses assigned because of incomplete diagnostic data and 33 persons whose diagnoses were deemed unreliable because they did not endorse symptoms consistent with their treatment setting (for example, clients from the detoxification programs who did not endorse substance use). The excluded group of 54 persons did not differ from the included group in terms of age, gender, ethnicity, or education.
Measures and data collection
Demographic data. Demographic data were collected directly from participants during the study intake interview and consisted of age, gender, race and ethnicity, and homelessness in the 30 days before treatment entry.
Clinical data. Diagnostic data were obtained during the study intake interview by research assistants who were trained to administer the Diagnostic Interview Schedule for DSM-IV (DIS-IV) ( 16 ) by a senior clinician who was trained on the instrument. With this measure, current 12-month psychiatric and substance use diagnoses were identified. For all disorders assessed, the DIS-IV includes questions about whether symptoms occurred only when the individual was under the influence of alcohol, illicit drugs, or prescription medications or were the result of a medical condition. For schizophrenia spectrum disorders, individuals were asked whether each endorsed type of delusion or hallucination was experienced only while under the influence of substances.
Current psychiatric diagnoses were grouped into four binary (yes-no) variables: schizophrenia spectrum disorders (schizophrenia, schizoaffective, and schizophreniform disorders), bipolar disorders (bipolar I and II), depressive disorders (major depression and dysthymia), and anxiety disorders (specific phobia and social phobia and panic, generalized anxiety, obsessive-compulsive, and posttraumatic stress disorders). These categories were not mutually exclusive; participants with more than one diagnosis were counted in each diagnostic category. Current substance use disorders comprised five binary variables and included use of alcohol, cocaine, amphetamines, opiates, and marijuana. Abuse and dependence diagnoses were collapsed into a single category because of paucity of participants meeting only abuse diagnoses. Co-occurring disorders were defined as having both a current mental disorder and a current substance use disorder.
Indicators of problem severity were collected during the intake interview. For analytic purposes, we operationalized psychiatric problem severity as "ever" being hospitalized for psychiatric problems, and we operationalized drug use severity as the number of current substance use diagnoses.
Utilization data. Electronic utilization data were obtained from the billing-information systems of the county mental health and substance abuse treatment systems. All county-run or county-contracted services report into these billing-information systems. Utilization data for the 24-month periods before and after study entry were downloaded, verified, and coded in consultation with county data system managers.
Two aggregate binary utilization variables were constructed: use of any mental health services and use of any substance abuse treatment services in the 24 months after treatment entry. Frequently used treatment services (subscribed to by 10% or more of the participants) were examined individually and transformed into binary variables as well. These included acute psychiatric hospitalization, mental health crisis residential treatment, mental health day treatment, psychiatric emergency services, mental health transitional residential services, mental health case management and (other) mental health outpatient services, crisis residential detoxification, residential drug-free treatment, and non-methadone-related outpatient services.
Continuous and count variables were created to reflect amount of services received over the 24 months. Amount of services was recorded as days or hours, depending on the units reported to the billing-information system.
Data analyses
Covariates. Variables included as covariates for the logistic and linear regressions were ones that either had significantly differentiated between the two treatment groups or that were supported in the literature. Covariates included gender ( 17 , 18 ), age ( 3 , 17 ), race-ethnicity ( 19 ), homelessness ( 20 , 21 ), a diagnosis of schizophrenia spectrum disorders versus all other disorders ( 22 ), severity of disorders, and prior service use (mental health treatment, substance abuse treatment, or both) ( 12 ). In analyses predicting mental health service use, any use of mental health services in the 24 months before study entry was included in the model; in analyses predicting substance abuse treatment use, any substance abuse treatment in the 24 months before study entry was included in the model.
Analyses. We implemented a two-part model ( 23 , 24 , 25 ), first using simultaneous logistic regressions to determine whether treatment system (mental health or substance abuse treatment) was a significant predictor of utilization. We then conducted zero-truncated negative binomial regressions ( 26 ) to determine whether treatment system was a significant predictor of amounts of services received that were measured in number of days (counts). For amounts of services measured in hours, we used ordinary least-squares regression, but because the distribution of these variables was highly skewed, we transformed the variables into their natural log. All tests of statistical significance were two-tailed. When appropriate, we applied Rom ( 27 ) corrections (a modified Bonferroni adjustment found in the literature) to all tests of significance to preserve the alpha level in multiple tests. The Rom adjustment controls the familywise error rate at the alpha designated as the significance level.
Results
Demographic and clinical characteristics
Demographic and clinical characteristics are listed in Tables 1 and 2 . The mean±SD ages for participants from substance abuse treatment (37.1±7.3) and those from mental health treatment (35.7±7.0) were not significantly different. Years of education were the same for both groups (substance abuse treatment participants, 12.4±2.3 years; mental health participants, 12.4±2.5 years). There were no differences between groups on frequency and type of mental disorders and substance use diagnoses.
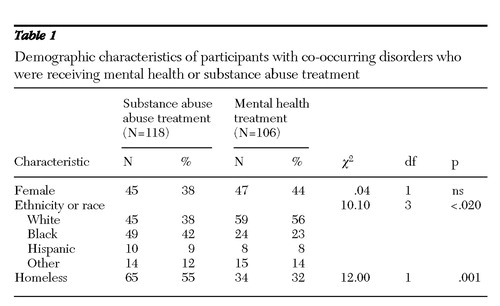 |
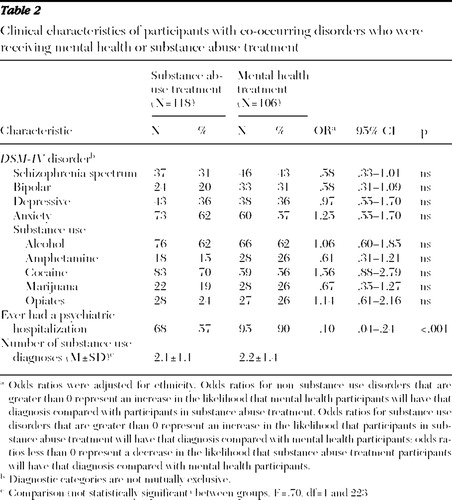 |
Utilization of services
Results of logistic regressions examining the effect of treatment system on service use variables are shown in Table 3 . After applying the Rom adjustment, we found that participants from substance abuse treatment were significantly less likely to use any mental health services, day treatment, transitional residential services, case management services, and non-case management mental health outpatient services. Substance abuse treatment participants were significantly more likely than mental health care participants to receive crisis residential detoxification.
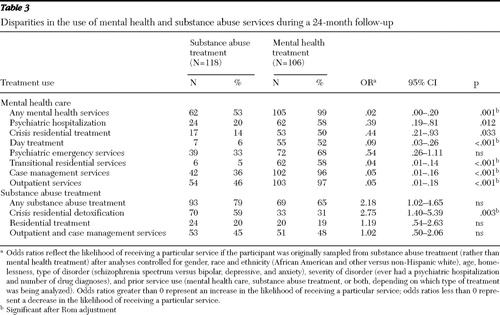 |
Amounts of services
Only participants who had some utilization of the given service were included in the analyses. The "amount" variables were difficult to analyze because of their non-normal distributions. We first examined the raw distributions and found some median differences between groups. Substance abuse treatment participants received a median of 8.6 hours of mental health case management, compared with a median of 21.1 hours received by mental health treatment participants. Substance abuse treatment participants received a median of 34.2 hours of other services (non-case management), compared with a median of 60.1 hours by mental health treatment participants. Participants from substance abuse treatment received more days of crisis residential detoxification (median of 10.0 days, versus a median of 7.5 days for mental health treatment participants).
Second, the distributions of services utilized were examined with zero-truncated negative binomial regression and linear regression with log transformations ( 26 ). Results of these analyses are shown in Table 4 . After Rom adjustments were made, the significant differences between groups that remained were in mental health outpatient hours and substance abuse residential treatment days.
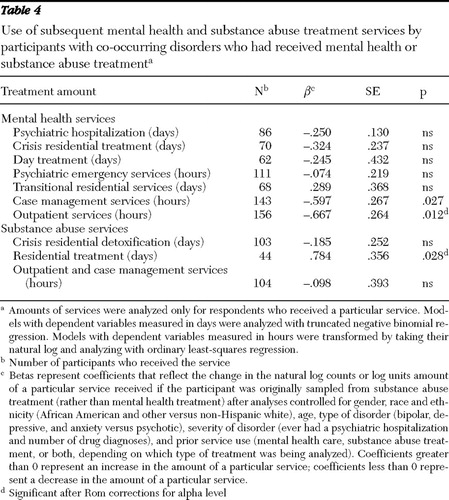 |
Discussion
Our objective was to investigate prospectively whether there were disparities in mental health and substance abuse treatment services obtained between two groups of individuals with co-occurring disorders. In comparison with participants recruited from mental health care, those in substance abuse treatment were significantly less likely to obtain community-based mental health services, specifically day treatment, transitional residential, case management, and outpatient services. Mental health treatment participants were significantly less likely than substance abuse treatment participants to obtain crisis residential detoxification services. There were few distinctions between the two treatment groups in amounts of services received. Mental health care participants received more hours of mental health outpatient services, and substance abuse treatment participants received more hours of drug residential treatment.
These differences are notable because on the basis of diagnostic similarities between groups, we had expected a level of parity between groups in obtaining mental health care and substance abuse treatment.
In part, differences between the groups may be attributable to linkage or referral arrangements between service units (such as between residential services and case management). The two treatment systems may have had different linkage arrangements, with some more effective than others. The literature indicates that linkage arrangements can affect utilization of medical and psychosocial services. One study found an increase in use of mental health services over a six-month period when services were available on site at drug treatment programs compared with off-site community programs that necessitated travel ( 28 ). Another study corroborated these results ( 29 ). Of the linkage mechanisms examined, on-site delivery and transportation assistance were associated with higher levels of utilization of medical and psychosocial services. On-site case management was associated with greater use of routine medical care and housing assistance. Referral agreements and off-site case management were not correlated with most services.
Participants' preferences and perceptions of treatment services also may have contributed to the utilization patterns ( 30 , 31 , 32 ). A qualitative study we conducted ( 30 , 31 ) included open-ended interviews of 24 adults with serious mental illness and co-occurring substance use problems. Perceived client-level barriers to receiving services were explored. Most of the respondents (71%) identified drug use as a serious problem in their lives. They believed that drug treatment was helpful for those committed to abstinence, but many did not think that abstinence was possible or desirable. Perceived barriers to care included discomfort with participating in 12-step groups, overemphasis on abstinence, insufficient attention to mental health issues, and drug treatment services' not being tailored to meet needs of persons with co-occurring disorders.
The patterns of disparities we obtained led us to reflect on the role that crisis residential detoxification treatment may play in facilitating entry into longer-term mental health and substance abuse treatment services. In the 24-month period subsequent to study entry, participants with co-occurring disorders who were using mental health care were significantly less likely to find their way into detoxification programs. We expected that these participants would need crisis detoxification services because their current substance use disorders were not significantly different from those of participants using substance abuse treatment. Furthermore, the participants recruited from substance abuse treatment were less likely to obtain subsequent supportive mental health outpatient community services, although their mental disorders did not significantly differ from the participants using mental health care. We suggest that crisis residential detoxification should be modified to better meet needs of both substance abuse and mental health clients. Crisis residential detoxification programs should include improved access to detoxification services for mental health clients and to provide improved linkages from detoxification into mental health treatment for substance abuse clients. In this manner, crisis residential detoxification services could be an ideal gateway into longer-term mental health and substance abuse treatments for clients with co-occurring disorders.
Study strengths
Different from most utilization studies, this research examined service use of persons with co-occurring mental and substance use disorders who were recruited concomitantly from the mental health and substance abuse treatment systems. We obtained utilization data directly from the billing-information systems of the mental health and substance abuse treatment systems. Because the treatment systems rely on these billing-information systems for reimbursement, the utilization data in our analyses reflect the most accurate and objective utilization data available. The study also had the advantage of including all of the programs in San Francisco that were either crisis residential mental health programs or residential detoxification programs.
Study limitations
An important consideration is the degree to which the results may be generalized. For this study, one issue of concern is the loss of potential participants. The recruiting procedures were based on the operations of the treatment settings. Research staff were informed by treatment staff of new treatment entrants and attempted to recruit them. Aside from persons who did not want to be in the study, there were losses of potential participants because some were not stable enough to sign an informed consent form, did not ultimately enter treatment after participating in the intake process, or would not be available for follow-up. These circumstances were not unique to this study but bear mentioning.
Another concern about generalizability is the extent to which our sample and findings are similar to those of other studies. Although we found no studies sufficiently similar to ours to make meaningful comparisons, the clinical and demographic characteristics of our sample fall within the range of values from related studies ( 33 ). Furthermore, we found studies documenting the undertreatment of mental disorders among clients with co-occurring disorders who were using substance abuse treatment ( 1 , 10 , 26 , 27 ). On the basis of this information, we suggest that our findings have applicability beyond San Francisco. We anticipate that these findings are relevant to urban areas similar to San Francisco, in particular those with extensive public-sector treatment systems that are not integrated in terms of funding, staffing, or patient flow.
Last, the utilization data, although certainly reflecting most of the service use, did not include all services that participants may have received, such as substance abuse treatment provided in mental health programs and mental health services provided in substance abuse treatment programs and services provided by programs that do not report into the billing-information systems. The use and amount of these services may have differentially affected the two groups. However, we believe that significant receipt of such services is unlikely, because there are generally few alternative service options for the low-income clients served in the public sector.
Conclusions
Although there were no diagnostic differences between participants recruited from the two treatment systems, significantly fewer participants from substance abuse treatment obtained services from the mental health treatment system and significantly fewer mental health participants obtained crisis residential detoxification services from the substance abuse treatment system. Study results should be considered in efforts of system modification and development and, furthermore, in research about mechanisms underlying results. Replications of this study must be conducted to assess the robustness of our findings in other locales and to address gaps in the study.
Acknowledgments and disclosures
This study was supported by grant R01-DA010836 from the National Institute on Drug Abuse (NIDA) to Dr. Havassy, principal investigator, and by NIDA grants T32-DA07250 and P50-DA09253. The authors acknowledge the assistance provided by Kevin Delucchi, Ph.D., Joseph Guydish, Ph.D, William McConnell, Ph.D., and James Sorensen, Ph.D. The authors also thank the study participants for their willingness to provide personal information.
The authors report no competing interests.
1. Harris KM, Edlund M: Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services 56:954–959, 2005Google Scholar
2. Narrow WE, Regier DA, Rae DS, et al: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Archives of General Psychiatry 50:95–107, 1993Google Scholar
3. Narrow WE, Regier DA, Norquist G, et al: Mental health service use by Americans with severe mental illnesses. Social Psychiatry and Psychiatric Epidemiology 35:147–155, 2000Google Scholar
4. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:17–31, 1996Google Scholar
5. Watkins KE, Burnam A, Kung FY, et al: A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatric Services 52:1062–1068, 2001Google Scholar
6. Results From the 2003 National Survey of Drug Use and Health: National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Statistics, 2004Google Scholar
7. Overview of Findings From the 2004 NSDUH. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Statistics, 2005Google Scholar
8. Results From the 2005 National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Statistics, 2006Google Scholar
9. Ducharme L, Knudsen H, Roman P: Availability of integrated health care for co-occurring substance abuse and psychiatric conditions. Community Mental Health Journal 42:363–375, 2006Google Scholar
10. Burman M, Watkins KE: Substance abuse with mental disorders: specialized public systems and integrated care. Health Affairs 25:648–658, 2006Google Scholar
11. Ridgely SM, Goldman HH, Willenbring M: Barriers to the care of persons with dual diagnoses: organizational and financing issues. Schizophrenia Bulletin 16:123–132, 1990Google Scholar
12. Ziedonis DM: Integrated treatment of co-occurring mental illness and addiction: clinical interventions, programs, and system perspectives. CNS Spectrums 9:892–904, 2004Google Scholar
13. Weisner C, Schmidt L: Expanding the frame of health services research in the drug abuse field. Health Services Research 30:707–726, 1995Google Scholar
14. Havassy BE, Alvidrez J, Owen KK: Comparisons of patients with comorbid psychiatric and substance abuse disorders: implications for treatment and service delivery. American Journal of Psychiatry 161:139–145, 2004Google Scholar
15. Matherlee K: Bridging silos: part II. DI, SSI, Medicare and Medicaid issues and initiatives. National Health Policy Forum, pp 1–18, 2003Google Scholar
16. Robins L, Cottler L, Bucholz K, et al: Diagnostic Interview Schedule for DSM-IV (DIS-IV). St Louis, Mo, Washington University School of Medicine, 1995Google Scholar
17. Hser YI, Maglione M, Polinsky ML, et al: Predicting drug treatment entry among treatment-seeking individuals. Journal of Substance Abuse Treatment 15:213–220, 1998Google Scholar
18. Grella CE: Effects of gender and diagnosis on addiction history, treatment utilization, and psychosocial functioning among a dually-diagnosed sample in drug treatment. Journal of Psychoactive Drugs 35(suppl 1): 169–179, 2003Google Scholar
19. Snowden LR: Barriers to effective mental health services for African Americans. Mental Health Services Research 3:181–187, 2001Google Scholar
20. Stein JA, Gelberg L: Homeless men and women: differential associations among substance abuse, psychosocial factors, and severity of homelessness. Experimental and Clinical Psychopharmacology 3:75–86, 1995Google Scholar
21. Gonzalez G, Rosenheck R: Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services 53:437–446, 2002Google Scholar
22. Wang P, Demler O, Kessler R: Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health 92:92–98, 2002Google Scholar
23. Duan N, Manning W, Morris C, et al: A comparison of alternative models for the demand for medical care. Journal of Business and Economic Statistics 1:115–126, 1983Google Scholar
24. Shrout PE, Newman SC: Design of two-phase prevalence surveys of rare disorders. Biometrics 45:549–555, 1989Google Scholar
25. Buntin M, Zaslavsky A: Too much ado about two-part models and transformations? Comparing methods of modeling Medicare expenditures. Journal of Health Economics 23:525–542, 2004Google Scholar
26. Long J, Freese J: Regression Models With Categorical Dependent Variables Using Stata. College Station, Tex, Stata Press, 2005Google Scholar
27. Rom DM: A sequentially rejective test procedure based on a modified Bonferroni inequality. Biometrika 77:663–665, 1990Google Scholar
28. Grella CE, Stein JA: Impact of program services on treatment outcomes of patients with comorbid mental and substance use disorders. Psychiatric Services 57:1007–1015, 2006Google Scholar
29. Friedmann PD, D'Aunno TA, Jin L, et al: Medical and psychosocial services in drug abuse treatment: do stronger linkages promote client utilization? Health Services Research 35:443–465, 2000Google Scholar
30. Alvidrez J, Kaiser D, Havassy BE: Perspectives of severely mentally ill clients on drug use and treatment. Presented at annual meeting of the American Public Health Association, San Francisco, Nov 2003Google Scholar
31. Alvidrez J, Kaiser D, Havassy BE: Severely mentally ill consumers' perspectives on drug use. Journal of Psychoactive Drugs 36:347–355, 2004Google Scholar
32. Appel PW, Ellison AA, Jansky HK, et al: Barriers to enrollment in drug abuse treatment and suggestions for reducing them: opinions of drug injecting street outreach clients and other system stakeholders. American Journal of Drug and Alcohol Abuse 30:129–153, 2004Google Scholar
33. Watkins KE, Hunter S, Wenzel S, et al: Prevalence and characteristics of clients with co-occurring disorders in outpatient substance abuse treatment. American Journal of Drug and Alcohol Abuse 30:749–764, 2004Google Scholar



