Use of Leverage to Improve Adherence to Psychiatric Treatment in the Community
Abstract
OBJECTIVES: A variety of tools are being used as leverage to improve adherence to psychiatric treatment in the community. This study is the first to obtain data on the frequency with which these tools are used in the public mental health system. Patients' lifetime experience of four specific forms of leverage—money (representative payee or money handler), housing, criminal justice, and outpatient commitment—was assessed. Logistic regression was used to examine associations between clinical and demographic characteristics and receipt of different types of leverage. METHODS: Ninety-minute interviews were conducted with approximately 200 adult outpatients at each of five sites in five states in different regions of the United States. RESULTS: The percentage of patients who experienced at least one form of leverage varied from 44 to 59 percent across sites. A fairly consistent picture emerged in which leverage was used significantly more frequently for younger patients and those with more severe, disabling, and longer lasting psychopathology; a pattern of multiple hospital readmissions; and intensive outpatient service use. Use of money as leverage ranged from 7 to 19 percent of patients; outpatient commitment, 12 to 20 percent; criminal sanction, 15 to 30 percent; and housing, 23 to 40 percent. CONCLUSIONS: Debates on current policy emphasize only one form of leverage, outpatient commitment, which is much too narrow a focus. Attempts to leverage treatment adherence are ubiquitous in serving traditional public-sector patients. Research on the outcomes associated with the use of leverage is critical to understanding the effectiveness of the psychiatric treatment system.
Treating people with mental disorders without their consent has always been the defining human rights issue in mental health law (1). For centuries compulsory treatment took place in inpatient settings, that is, mental hospitals. In recent years, the loci of involuntary treatment have shifted from institutions to the community. Much of the vigorous policy debate on outpatient commitment—a judicial civil order directing a person with a mental disorder to adhere to a prescribed community treatment plan—treats the topic as if it were simply an extension of inpatient commitment into the community. However, we have argued elsewhere that rather than viewing outpatient commitment as a diluted form of institutionalization, it should be seen in a broader legal and clinical context as one of several legal tools derived from the social welfare and judicial systems that are now being used to attempt to improve adherence to treatment (2,3).
People with mental disorders are often dependent on resources provided by welfare agencies. Their access to these goods and services may be tied to treatment participation. For example, because individuals with mental disorders sometimes have cognitive deficits that impair their ability to manage money, the Social Security Administration may appoint a representative payee to manage the individual's disability benefits (4,5). In addition, many people with mental disorders have their finances informally managed by family members. Some representative payees and informal money managers construe their role as supervisory and make access to funds contingent on treatment adherence (6,7).
Also, to help prevent homelessness, the government provides a number of housing options in the community for people with mental disorders that it does not provide for other citizens. Some landlords use the promise of obtaining or retaining subsidized housing as leverage to attempt to secure adherence to medication or psychosocial treatment, often in the belief that treatment adherence will make people with mental illness better tenants (8).
Many people with mental disorders also come into contact with the judicial system. Lenient disposition of their cases may be made conditional on accepting treatment for their disorder in the community. For example, making the receipt of mental health services a condition of probation has long been an accepted judicial practice (9,10). A new type of criminal court, a "mental health court," has recently been developed that makes even more transparent the link between criminal sanctioning and treatment in the community (11,12). Finally, outpatient commitment is meaningfully being implemented for the first time in an increasing number of states (13,14).
The study reported here is the first to obtain reliable data on how often various forms of leverage are applied to people with mental disorders in an attempt to secure their adherence to treatment in the community. Because the overall use of leverage and the distribution of the various types of leverage may differ greatly from site to site, we selected sites on the basis of regional diversity and variation in the size of the cities that the sites are located in. The survey sites included two smaller-population cities, Durham, North Carolina (population 187,035) and Worcester, Massachusetts (population 172,648), and three larger-population cities, Tampa, Florida (population 303,447), San Francisco (population 776,733), and Chicago (population 2,896,016). Finally, we determined which demographic and clinical characteristics were most associated with the use of leverage.
Methods
Participants
Approximately 200 outpatients (range, 200 to 205) from publicly funded mental health programs were sampled from each of five sites: Chicago; Durham, North Carolina; San Francisco; Tampa, Florida; and Worcester, Massachusetts. Although we specified that participants had to be treated for mental disorders (rather than for only a substance use disorder), we did not specify a diagnosis or a given level of acuity. The specific inclusion criteria for participation in our study were being aged 18 to 65 years, able to speak English or Spanish, and currently in outpatient treatment for a mental disorder with a publicly supported mental health service provider (operationally defined as at least one appointment or visit in the past six months) and having the first service contact as an adult at least six months ago.
Because of constraints that were imposed by the different institutional review boards that approved the study at each site, two recruitment strategies were used. At the Worcester, Tampa, and San Francisco sites, potential participants were recruited sequentially in the waiting rooms of outpatient clinics in community mental health centers. Outpatients were asked if they wanted to hear about a study on mental health treatment. Of those who expressed interest in hearing about the study, a mean of 12 percent did not meet inclusion criteria (Ns ranged from 15 to 24 across the three sites) and a mean of 7 percent refused to participate (Ns ranged from 7 to 34). In Durham a list of potentially eligible participants was created from management information system data, and these patients were randomly selected to be approached about the study. Of those who were told about the study in Durham, 3 percent (N=8) did not meet eligibility criteria and 13 percent (N=32) refused to participate. Finally, both recruitment strategies were used at the Chicago site. Half of this sample was obtained by using the waiting room approach and the other half by using the eligibility list approach. Rates of ineligibility and refusal at the Chicago site were 5 percent (N=13) and 2 percent (N=4), respectively.
After the study was completely described to the participants, written informed consent was obtained. Participants were interviewed in person by trained interviewers and paid $25 for an interview that lasted an average of 90 minutes. After interviews were conducted, research personnel obtained diagnostic information from participants' clinic charts. Data collection ran from October 2002 through December 2003, although on average data collection at each site was completed in four to six months.
Measures
Leverage. We assessed participants' lifetime experience of four specific tools derived from the social welfare system—money and housing as leverage—and the judicial system—criminal sanction and outpatient commitment as leverage, including related judicial orders, such as "Rogers orders" in Massachusetts. All patients were questioned about their experience with outpatient commitment and housing. For example, for housing, patients were asked, "Did you ever live somewhere where you felt you were required to stay in mental health or substance abuse treatment or required to continue taking your medication?" Only the relevant subsets of patients were questioned in greater detail about their experience with the criminal justice system and money. Persons for whom the use of money as leverage was considered relevant were those who had a formal representative payee or an informal money manager. Persons for whom leverage by the criminal justice system was considered relevant were those who had been arrested, convicted, or on probation and those who were on parole. For example, participants who had been involved with the criminal justice system were asked, "Sometimes a police officer or a prosecutor or a judge tells you or your lawyer that the charges would be dropped or reduced if you get treatment in the community for your mental health, alcohol, or drug problems. Did anyone ever tell you or your lawyer this?" Finally, a binary leverage summary variable was created. Participants who reported at least one of the four leverages were considered as having had experienced "any leverage"; those who did not were considered to have experienced "no leverage."
Clinical characteristics. Objective diagnostic information was obtained by chart review. In addition, the anchored version of the Brief Psychiatric Rating Scale (BPRS) was used to assess current psychiatric symptoms (15). The Global Assessment of Functioning was used to assess current functioning levels (16). Insight into mental illness was assessed with the Insight and Treatment Attitudes Questionnaire (17). Self-reported alcohol and drug use for the past 30 days was also obtained. If participants had taken any alcohol, nonprescribed drugs, or street drugs, follow-up questions were asked that had been adapted from the Michigan Alcoholism Screening Test and the Drug Abuse Screening Test (18,19). We combined alcohol and drug abuse symptoms and dichotomized them into "one or more substance abuse symptoms" (score of 1) and "no substance abuse symptoms" (score of 0).
Interviewers at each site were trained in reliable administration of the interview. For example, the proportion of agreement (within 10 points) between interviewers and an experienced psychiatrist for total scores on the BPRS ratings was 91 percent across the five sites (out of a total of 84 possible ratings).
Statistical analysis. We used logistic regression to examine the joint associations between participants' demographic and clinical characteristics and their receipt of different types of leverage. For the purpose of multivariate modeling, pooling the data across sites offered the advantage of greater statistical power, but it also posed two problems that required adjustment in the analyses.
First, we had to account for site effects and site-by-covariate interactions associated with leverage. To examine and control for these site effects, we used Zelen's test of the homogeneity of odds ratios (20,21). The Zelen statistic allowed us to test the null hypothesis that the relative risk of leverage did not differ across the five sites but instead represented a sampling distribution from a common population. If Zelen's test showed the sites' odds ratios for a given variable were homogeneous, we then pooled the data for that variable and calculated a common odds ratio across sites.
The second problem was that pooling the data could have distorted statistical inferences, insofar as the observations within each site were not independent. Without an adjustment for the clustered nature of the data, the standard errors around the pooled estimates would have been understated, leading to overly liberal tests of statistical significance. Accordingly, we used specialized statistical software, StatXact, to adjust significance tests and confidence intervals around the common (pooled) odds ratios (21). For multivariable analysis, we used a companion statistical package designed to conduct multivariate logistic regression with stratified data (Proc-LogXact) (22). These techniques provided the appropriate correction of variance estimates while taking into account within-site correlation of observations. Specifically, Proc-LogXact uses the Cochran-Armitage method, as adapted by Rao and Scott (23), to adjust the "effective sample size" for design effects that occur with a clustered sample (22).
Results
Table 1 lists the demographic and clinical characteristics of participants by site. Table 2 shows the site-specific lifetime usage rates of the four assessed forms of leverage. For the use of the criminal justice system and money as leverage, both the rates in the relevant subsample and in the total sample of people who experienced the leverages are reported. The number of people who were arrested or convicted ranged from 82 to 123 across the five sites, with a total of 512. The number of people who had a representative payee or an informal money manager ranged from 86 to 124, with a total of 519.
The percentage of patients who experienced at least one form of leverage varied within a fairly narrow range, from 44 percent in Durham to 59 percent in San Francisco. Somewhat more variation was seen across sites in the use of specific forms of leverage. Money was used as leverage for 7 to 19 percent of all patients (15 to 31 percent of patients who had either a representative payee or a money handler). Outpatient commitment was reported by 12 to 20 percent of all patients. The criminal justice system was used as leverage for 15 to 30 percent of all patients (38 to 49 percent of the patients who had been arrested or convicted). Housing was used as leverage for 23 to 40 percent of all patients.
We were also interested in studying the profile of demographic and clinical characteristics that were most associated with the use of leverage. We first examined bivariate associations between each type of leverage and a range of salient variables: age, gender, race, diagnosis, substance abuse, symptomatology, functioning, insight into illness, time in treatment, hospitalizations, and frequency of outpatient visits. Continuous variables were recoded into high and low categories (above and below the median) to better capture nonlinear associations and to allow a common, efficient test of whether the five sites differed in the relationship of each characteristic to the receipt of each type of leverage.
Table 3 displays the results of the bivariate analysis across the different types of leverage. Each of the four types of leverage was found to be significantly more common among participants with a history of multiple hospitalizations and among those with low global functioning. Psychotic disorders were significantly associated with money and housing leverages across all sites and with outpatient commitment and criminal justice leverage at some, but not all, sites. Participants with BPRS global symptom scores that were higher than the median were significantly more likely to receive housing leverage, criminal justice leverage, and, at three sites, outpatient commitment. Co-occurring substance abuse was significantly associated with receiving all types of leverage except for housing. An inconsistent pattern was found for the measure of insight, with lower insight being significantly associated with receiving money leverage and higher insight being significantly associated with receiving criminal justice and housing leverage.
Multivariate logistic regression analyses (22) for the four types of leverage are shown in Table 4. When the analyses controlled for clinical factors, respondents who were male were more likely to have received leverage related to housing and criminal justice. Younger respondents were more likely to have received leverage related to criminal justice and money. With respect to clinical and service-use characteristics, psychotic disorders were associated with receiving money leverage, whereas multiple hospitalizations were associated with all four types of leverage, and lower functioning was associated with outpatient commitment and housing. Substance abuse showed an inconsistent pattern of association across the leverage types—significantly increasing the likelihood of receiving outpatient commitment, criminal justice, and money leverage but significantly decreasing the likelihood of receiving housing leverage.
Table 5 presents bivariate and multivariate analyses of variables associated with the combined index of any leverage. These findings must be interpreted with caution, because some characteristics are significantly associated with only some types of leverage and not with others. These analyses showed that when all other variables were controlled for, receiving any type of leverage was significantly less common among individuals older than 44 years and significantly more common among those with lower functioning, multiple hospitalizations, higher-intensity outpatient service use, and longer total time in treatment. It must be noted that the association between substance abuse and receiving any leverage is diluted, because outpatient commitment, criminal justice, and money leverage tends to be applied to substance abusers but housing does not.
Discussion
Although the percentage of patients who reported that they experienced at least one form of leverage varied within a fairly narrow range (44 to 59 percent) across sites from different regions of the country and of differing degrees of urbanization, we found more substantial variation in the types of leverage used across sites. For example, Durham had a rate of outpatient commitment leverage (20 percent) that was almost twice as high as the rate found in Chicago (12 percent) but a rate of use of money as leverage (9 percent) that was barely more than half of that found in Chicago (19 percent). Among all the sites, San Francisco had the highest rate for using housing as leverage (40 percent) and the criminal justice system as leverage (30 percent) but the lowest rate for using money as leverage (7 percent). This suggests some fungibility across types of leverage, with the overall rate of leverage remaining fairly constant.
Part of this variation in the mix of leverages may relate to the fact that specialized programs have developed in a certain location. For example, Chicago has developed innovative representative payee programs (24), so it is not surprising that money would often be used as leverage there.
We caution that the site-specific prevalence estimates reported here cannot be combined or averaged across sites to produce national estimates for the U.S. population. Moreover, differences between the sites in the prevalence of leverage cannot be interpreted simply as regional differences. The five sites were not chosen at random, and they used variations on a common approach to sample selection. In their demographic and clinical characteristics, the samples differ significantly from each other on a number of variables associated with the use of leverage. The samples also differ from broader, nationally representative survey samples of individuals who receive specialty mental health services in the community. For example, compared with respondents from the National Institute of Mental Health's National Comorbidity Study (25) who were in active treatment for mental disorders, our samples included a significantly higher proportion of males, individuals with psychotic disorders, and outpatients who used services at a high frequency.
Because each of these three variables was found to be significantly associated with receiving one or more types of leverage, it is possible that our estimates of the frequency of our sample's receipt of leverage are somewhat higher than would have been obtained in a random national survey of persons in treatment for mental disorder. However, national survey samples may not adequately represent individuals with severe and persistent mental illness.
Nonetheless, the pattern of bivariate and multivariate associations reveals a fairly consistent picture of legal and other forms of leverage being used significantly more frequently for male patients; those younger than 45 years; those with more severe, disabling, and longer-lasting psychopathology; those with a pattern of multiple hospital readmissions; and those with intense outpatient service use. However, given the cross-sectional nature of the study, interpreting the causal ordering of some of these associations is difficult. For example, the higher rate of outpatient service use for those with a history of leverage could be a consequence of the use of leverage, or it could simply indicate greater need for treatment over time, resulting from greater severity and acuity of illness.
The association between participants' insight into their illness and receipt of leverage suggest that there may be at least some important differences in the populations who are recipients of different types of leverage. For example, although participants with less insight were more likely to receive money as leverage, those with relatively greater insight were more likely to receive criminal justice and housing leverage.
Consistent with the findings on the use of each type of leverage and on the combined index of the use of any type of leverage, the multivariate analysis showed that when all other variables were controlled for, leverage was significantly more likely to be received by individuals who were younger than 44 years, with lower functioning, and with a history of multiple hospitalizations, higher-intensity outpatient service use, and longer total time in treatment.
Conclusions
The study presented here is the first attempt to obtain systematic information on how often given forms of leverage are applied to people with mental disorders in an attempt to improve their adherence to treatment in the community. Broadly speaking, we found that approximately half the public-sector patients whom we surveyed at five sites had experienced at least one form of leverage at some point in their treatment history.
At each of the five sites, the most prevalent form of leverage—applied to between 23 and 40 percent of all patients—was the use of housing in an attempt to secure treatment adherence. The frequency with which housing is used as leverage is in stark contrast to the dearth of attention that, at least until recently, this topic has generated from researchers and advocates (26). Likewise, at every site except for Durham, avoidance of involvement in the criminal justice system was the second most prevalent form of leveraged treatment, used with between 15 and 30 percent of all patients and between 38 and 49 percent of patients who had been charged with a criminal offense. Only recently has this use of leverage begun to receive the empirical attention that it would seem from these data to merit (27).
In contrast to these understudied forms of leverage, at most sites outpatient commitment and related judicial orders—which are the subject of an extensive body of scholarly literature and much legal commentary—were the least prevalent form of leverage, applied to between only 12 and 20 percent of patients. Indeed, outpatient commitment is a separate and explicit section of the involuntary commitment statute in only two of the states studied (North Carolina and Illinois), and in the remaining states it is permitted under the general involuntary commitment statute.
The data reported here suggest that the focus of the current policy debate on one form of leverage—outpatient commitment—is much too narrow: leveraged treatment is ubiquitous in serving traditional public-sector patients. Opponents of outpatient commitment may believe that outpatient commitment still deserves a central role in debates on mental health policy, because outpatient commitment is more formally coercive and potentially stigmatizing than other forms of leverage. However, the leading case that upheld outpatient commitment did so precisely because the coercion involved was minimal: the court stated that "a violation of the [outpatient commitment] order, standing alone, ultimately carries no sanction" (28). In future analyses, we will examine the comparative effects of outpatient commitment and other forms of leverage on the amount of coercion and stigma perceived by patients and on their attitudes toward treatment engagement.
Given the widespread prevalence of the use of leverage, understanding how, or whether, leverage works is critical to understanding the effectiveness of the psychiatric treatment system. More specifically, our findings raise two crucial questions for further research: what types of patients are most amenable to the effective use of leverage, and what types of leverage are most effective in improving adherence among these patients to treatment in the community?
Acknowledgments
This research was supported by the MacArthur Research Network on Mandated Community Treatment. The authors thank Karen Albert, M.S., Annette Christy, Ph.D., Barbara Gormley, Ph.D., and Barbara McCauley, M.A.
Dr. Monahan is affiliated with the University of Virginia School of Law, 580 Massie Road, Charlottesville, Virginia 22903 (e-mail, [email protected]). Dr. Redlich, Dr. Steadman, and Ms. Robbins are with Policy Research Associates in Delmar, New York. Dr. Swanson and Dr. Swartz are with the department of psychiatry at Duke University Medical Center in Durham, North Carolina. Dr. Appelbaum is with the department of psychiatry at the University of Massachusetts Medical Center in Worcester. Mr. Petrila is with the department of mental health law and policy at the University of South Florida in Tampa. Dr. Angell is with the social services administration at the University of Chicago. Dr. McNiel is with the department of psychiatry at the University of California, San Francisco.
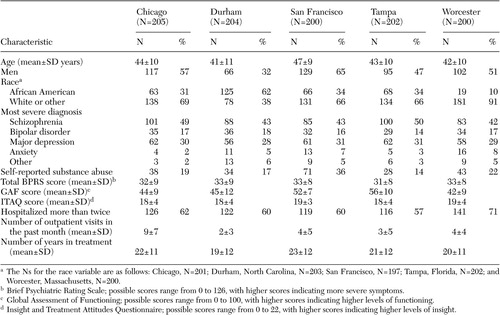 |
Table 1. Demographic and mental health characteristics of outpatients participating in a study on the use of leverage for treatment adherence, by site
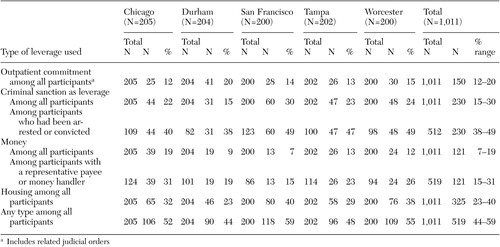 |
Table 2. Types of leverage received by outpatients over their lifetime, by site
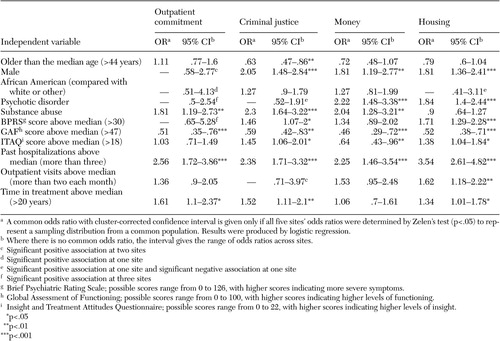 |
Table 3. Cross-site bivariate associations between characteristics and types of leverage received by outpatients at five sites
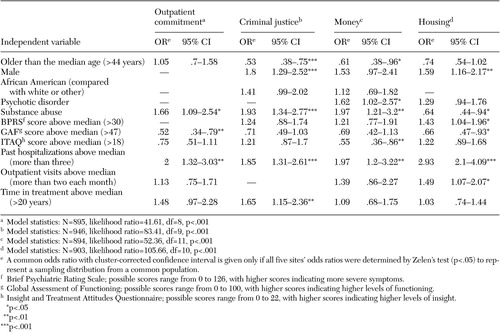 |
Table 4. Cross-site multivariate models of characteristics associated with types of leverage
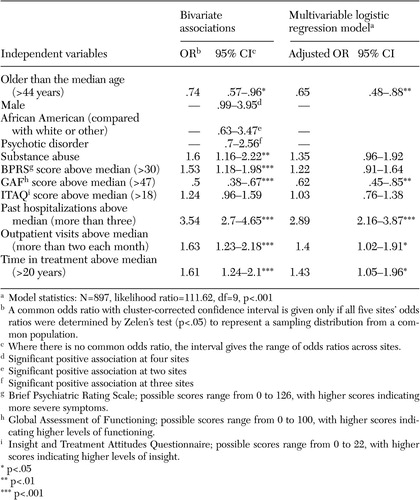 |
Table 5. Cross-site multivariate model and bivariate associations with receiving any type of leverage among outpatients at five sites
1. Appelbaum PS: Almost a Revolution: Mental Health Law and the Limits of Change. New York, Oxford University Press, 1994Google Scholar
2. Monahan J, Bonnie R, Appelbaum P, et al: Mandated community treatment: beyond outpatient commitment. Psychiatric Services 52:1198–1205, 2001Link, Google Scholar
3. Monahan J, Swartz M, Bonnie R: Mandated treatment in the community for people with mental disorders. Health Affairs 22(5):28–38, 2003Google Scholar
4. Grisso T, Appelbaum P: Assessing Competence to Consent to Treatment: A Guide for Physicians and Other Health Professionals. New York, Oxford University Press, 1998Google Scholar
5. Pescosolido B, Monahan J, Link B, et al: The public's view of the competence, dangerousness, and need for legal coercion among persons with mental illness. American Journal of Public Health 89:1339–1345, 1999Crossref, Medline, Google Scholar
6. Elbogen E, Swanson J, Swartz M: Psychiatric disability, the use of financial leverage, and perceived coercion in mental health services. International Journal of Forensic Mental Health 2:119–127, 2003Crossref, Google Scholar
7. Elbogen E, Swanson J, Swartz M, et al: Characteristics of third-party money management for persons with psychiatric disabilities. Psychiatric Services 54:1136–1141, 2003Link, Google Scholar
8. Allen M: Waking Rip Van Winkle: Why developments in the last 20 years should teach the mental health system not to use housing as a tool of coercion. Behavioral Sciences and the Law 21:503–521, 2003Crossref, Medline, Google Scholar
9. Skeem J, Encandela J, Louden J: Perspectives on probation and mandated mental health treatment in specialized and traditional probation departments. Behavioral Sciences and the Law 21:429–458, 2003Crossref, Medline, Google Scholar
10. Skeem J, Petrila J: Specialty probation for individuals with mental illnesses. Court Review 40:8–15, 2004Google Scholar
11. Griffin P, Steadman H, Petrila J: The use of criminal charges and sanctions in mental health courts. Psychiatric Services 53:1285–1289, 2002Link, Google Scholar
12. Redlich A, Steadman H, Monahan J, et al: The second generation of mental health courts. Psychology, Public Policy, and the Law, in pressGoogle Scholar
13. Swartz M, Swanson J, Hiday V, et al: A randomized controlled trial of outpatient commitment in North Carolina. Psychiatric Services 52:325–329, 2001Link, Google Scholar
14. Swartz M, Swanson J, Wagner H, et al: Assessment of four stakeholder groups' preferences concerning outpatient commitment for persons with schizophrenia. American Journal of Psychiatry 160:1139–1146, 2003Link, Google Scholar
15. Moerner MG, Mannuzza S, Kane JM: Anchoring the BPRS: an aid to improved reliability. Psychopharmacology Bulletin 24:112–117, 1988Medline, Google Scholar
16. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
17. McEvoy J, Apperson LJ, Appelbaum P, et al: Insight into schizophrenia: its relationship to acute psychopathology. Journal of Nervous and Mental Disease 177:43–47, 1989Crossref, Medline, Google Scholar
18. Selzer ML: The Michigan Alcoholism Screening Test: the quest for a new diagnostic instrument. American Journal of Psychiatry 127:1653–1658, 1971Link, Google Scholar
19. Skinner HA: The Drug Abuse Screening Test. Addictive Behaviors 7:363–371, 1982Crossref, Medline, Google Scholar
20. Zelen M: The analysis of several 2 x 2 contingency tables. Biometrika 58:129–137, 1971Google Scholar
21. StatXact: Statistical Software for Exact Nonparametric Inference. Cambridge, Mass, Cytel Software Corporation, 2003Google Scholar
22. LogXact. Software for Exact Logistic Regression. Cambridge, Mass, Cytel Software Corporation, 2002Google Scholar
23. Rao J, Scott A: A simple method for the analysis of clustered binary data. Biometrics 48:577–585, 1992Crossref, Medline, Google Scholar
24. Luchins DJ, Hanrahan, P, Conrad KJ, et al: An agency-based representative payee program and improved community tenure of persons with mental illness. Psychiatric Services 49:1218–1222, 1998Link, Google Scholar
25. Kessler R: The National Comorbidity Survey, in Textbook in Psychiatric Epidemiology, 2nd ed. Edited by Tsuang M, Tohen M, Zahner G. New York, John Wiley and Sons,2003Google Scholar
26. Tsemberis S, Eisenberg RF: Pathways to housing: supported housing for street-dwelling homeless individuals with psychiatric disabilities. Psychiatric Services 51:487–493, 2000Link, Google Scholar
27. Griffin P, Steadman HJ, Petrila J: The use of criminal charges and sanctions in mental health courts. Psychiatric Services 53:1285–1289, 2002Link, Google Scholar
28. In re KL, 806 NE 2d 480 (Court of Appeals of New York 2004)Google Scholar



