Service Use and Cost in 2002 Among Clients in Community Settings Who Were Discharged From a State Hospital in 1989
Despite the magnitude of changes brought about by deinstitutionalization, there is little longitudinal information on the extent to which former long-stay state hospital patients have fared in the outpatient community mental health system and whether utilization and cost of care in this population is less than the cost of institutionalization. This article provides a ten-year follow-up analysis of a group of discharged state hospital patients whose use of services and cost of care were originally documented in 1992 as part of an evaluation of a major state hospital closing in Pennsylvania ( 1 , 2 , 3 ). The study reported here examined the service patterns and cost of care for a subset of the original 1992 study cohort.
During the 1970s and 1980s many in the mental health community believed that the policy of deinstitutionalization had greatly diminished the safety net for persons with serious mental illness. A key question was whether deinstitutionalization contributed to rising rates of homelessness, substance abuse, and involvement in the criminal justice system ( 4 , 5 ). Concerns were also raised that the reduction of state hospital beds would lead to higher rates of inpatient psychiatric admissions and readmissions to community hospitals. Studies conducted over the years have found little evidence that the discharged patient population is greatly involved in the criminal justice system or admitted to homeless shelters ( 1 , 6 , 7 , 8 ). Furthermore, other studies have found that patients have done as well or better in the community as in institutions ( 9 , 10 ) and that most former patients much prefer their life outside the state hospital ( 7 , 11 , 12 , 13 ).
However, few longitudinal studies of this population have been done. One frequently cited study, the Vermont 32-year longitudinal study, found that half of the patients achieved considerable improvement after their hospital discharge ( 14 ) and, except for a small group of patients with specialized problems, most long-stay patients appeared to be capable of maintaining or improving their level of functioning while receiving treatment in a community system ( 15 ). Although these were encouraging findings, it is difficult to generalize from these results because we do not know whether the Vermont study cohort was less disabled than the patients who were being discharged in later years ( 16 ).
Studies examining utilization and cost of community care for patients after discharge from state hospitals found that the cost was no greater, and in many cases less, than the cost of institutionalization ( 1 , 2 , 3 , 8 , 12 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ). The study reported here documents the utilization and cost of care in 2002 of patients who were discharged from a state hospital in 1989 ( 1 , 3 ).
Methods
In the previous study of long-stay patients discharged to the community from the Philadelphia State Hospital in 1989, a total of 321 patients from a discharge cohort of 590 were followed for a three-year period. During that time 20%–30% had at least one hospital admission in each of the three years. The total treatment cost per participant was approximately $60,000 a year in 1992 dollars compared with the estimated cost of $130,000 per year had the patient remained institutionalized. Residential care constituted 74% of the cost of community care.
Participants
We selected 150 individuals from a group of 370 who were alive at the time of this study and continuously eligible for Medicaid during 2002, because Medicaid eligibility allowed us to obtain comprehensive service and cost data. All participants were formerly long-stay patients at Philadelphia State Hospital who had been there for a year or longer during the episode just before their discharge in 1989. Excluded were individuals whose care was reimbursed by Medicare only, because Medicare data were not available to investigators. Dually eligible individuals were included in the study, because Medicaid data included both sources of payment for those who were dually eligible.
Data sources
Demographic and diagnostic information was obtained from the state hospital data set used in the original study ( 1 ). Medicaid claims records for 2002 provided information about inpatient, nursing home, outpatient, and pharmacy services. Information about use of residential care and social and vocational services was obtained from a county database and from administrative records kept by the case management team that had been monitoring the state hospital population since discharge. Expenditure data for services and medication came from Medicaid claims records, which also included Medicare payments. Expenditures for residential care and rehabilitation were derived from county fiscal data. In addition, data on shelter admissions were obtained from the County Office of Services to the Homeless, data on jail incarceration were from the county jail file, and mortality data were from the Vital Statistics Division of the Pennsylvania Department of Health. Service data from various sources were integrated across data files, and any duplicate claims were eliminated ( 26 ).
No direct client contact was involved in the study. The research was approved by the University of Pennsylvania's institutional review board through the Office of Regulatory Affairs.
Measures
Average utilization rates per user and unit costs per participant were constructed by type of service. The per participant measure is the mean value for the study group, whereas the per user measure characterizes the care for participants who received services during the study year. Service units were measured in days, hours, visits, or contacts, and pharmaceutical information is presented as the percentage of users. Annual participant costs for psychiatric inpatient care were calculated by summing across all inpatient reimbursement amounts paid by Medicaid and Medicare in 2002 divided by the number of participants in the study. The expenditure for residential care per user was based on the total number of days spent in a given residential facility during the year multiplied by the daily cost for that facility in 2002 and divided by the number of participants living in residential settings. Finally, total cost per participant was calculated by summing all user service costs divided by the number of participants.
Unit expenditures were calculated in 2002 dollars on the basis of paid claims and program-level budget figures. The cost of state hospital care in 2002 was based on a national expenditure study showing the average per diem cost of state hospital care for adult civil patients to be $446 and the median to be $437 ( 27 ). A Pennsylvania state hospital report listed the per diem cost in 2002 as $463 per day (Altenor R., personal communication, Dec. 14, 2006). The cost estimates do not distinguish between long-stay and acute care patients.
Results
Participant characteristics
Table 1 presents information on demographic and clinical characteristics of the study sample. A majority of participants were male (63%), African American (57%), and unmarried (90%). Most had a diagnosis of schizophrenia (87%). The mean±SD age in 2002 was 51±10 years, with a median age of 48.5 years. The mean length of stay during the inpatient stay at Philadelphia State Hospital just before the 1989 discharge was 7.7±8.6 years. Ten percent were dually eligible for Medicaid and Medicare.
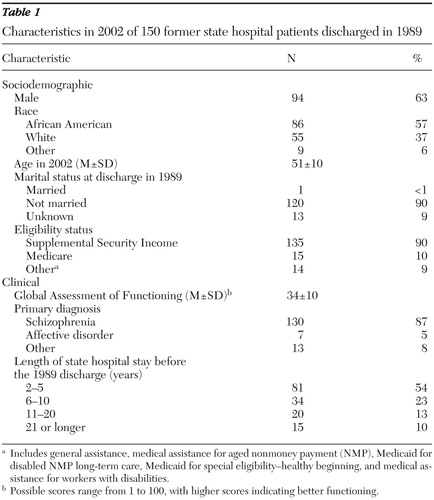 |
Few differences were noted between the current sample and the 1992 sample. In the original cohort 80% of patients were Medicaid eligible, and fewer were African American (45%) ( 1 ). No significant differences in sociodemographic characteristics were found between our sample of 150 participants and the 370 individuals from the original cohort who were alive at the time of this study; however, the excluded participants were either not long-stay patients in the original study or not Medicaid eligible during 2002.
Utilization patterns
Psychiatric service utilization.Table 2 provides information on the percentage of study participants who used services, by service type and level of use during 2002. Eighteen percent were hospitalized for psychiatric treatment in 2002 in either an acute or extended acute care psychiatric unit of a general hospital. The mean number of inpatient psychiatric days per user was 59.6±69.8; 57% were in acute units. Patients had to have an acute hospitalization before being transferred to extended acute facilities.
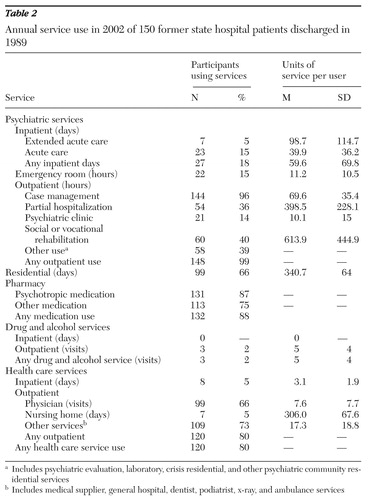 |
With respect to ambulatory care, 15% of the sample visited an emergency room at least once during 2002. Practically all participants (99%) were engaged in some form of outpatient mental health services. Intensive case management services were provided primarily by the community treatment team staff, the original case management providers at the time of the closure. The discharged clients were still tracked by these staff, even though a court settlement requiring oversight and monitoring was no longer mandated ( 3 , 28 , 29 ).
Intensive case management services were provided to 96% of the sample, with a mean of 69.6 hours or at least one hour of contact a week in 2002. The community treatment team agency also provided a nurse as part of the case management service. Partial day care services were used by 36% of the sample, with an average of 398.5 hours per user in 2002—or approximately eight hours a week over 50 weeks. Forty percent of the sample received social or vocational rehabilitation services; the mean amount of time spent in such services was 613.9 hours in 2002—or about 12 hours a week for 50 weeks. Use of psychiatric clinic services, such as individual and group psychotherapy, was relatively low (14%), with a mean of 10.1 hours in 2002. Other outpatient psychiatric services provided to 39% of the sample consisted of psychiatric evaluation, laboratory services, and crisis-related care.
Drug and alcohol use. Although the literature on serious mental illness shows a high rate of comorbidity with substance abuse ( 30 ), none of the discharged patients had an inpatient stay for substance abuse problems in 2002 and only 2% received outpatient drug and alcohol treatment, with a mean of five visits during the year.
Use of psychotropic medications. On the basis of Medicaid pharmacy claims data, 87% of the study participants received psychotropic medication in 2002, and 75% received medication for medical problems.
Use of residential care. Approximately 66% of the sample lived in residential care settings funded with state block grant dollars and operated by private providers. A majority of these residential care users lived in settings that were moderately to highly supervised, with 8% (N=8) in long-term highly structured settings with 24-hour care. The remainder of the population lived at home with relatives or in boarding homes.
Use of medical care. Most study participants (80%) received outpatient health care services; the mean number of contacts per year for physician visits was 7.6. Most of the other health care contacts (17.3 contacts) were for laboratory and diagnostic procedures. Five percent of the study participants were hospitalized for medical care in 2002, with relatively short stays of 3.1 days.
Expenditure patterns
Table 3 shows the mean and median expenditures per participant by type of service in 2002. These data reflect the group mean rather than the user mean (presented in Table 2 ).
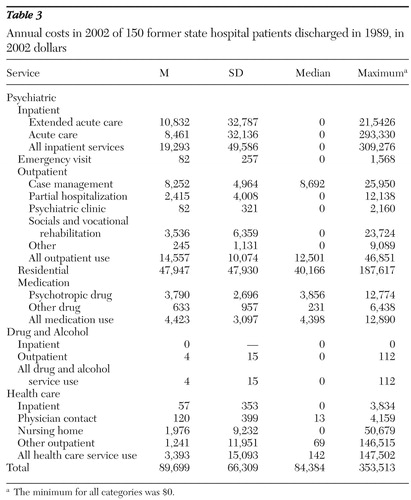 |
Psychiatric costs. Mean costs for psychiatric hospitalization per participant in 2002 were $19,293; 56% of these costs, or $10,832, were for extended care. Mean costs of outpatient services were $14,557 per participant, with case management accounting for 57%.
Residential costs. Mean housing costs for participants living in state-funded residences were $47,947 per participant, by far the largest cost component. On a per user basis this translates into $6,054 a month.
Pharmaceutical costs. Total medication expenditures were $4,423 a year, with 86% of the costs allotted to psychotropic drugs.
Drug and alcohol treatment costs. Expenditures for drug and alcohol treatment were minor because only three clients received outpatient services and none were admitted for inpatient treatment.
Health care costs. The cost of medical care was $3,393 per year, with 40% of expenditures for outpatient care. These costs were for hospitalization, nursing home care, home health care, physician visits, dental and podiatry services, laboratory and other ancillary services, and outpatient care.
Total costs. In 2002 expenditures for the former state hospital cohort were $89,699 per participant; care related to psychiatric conditions accounted for over 96% of the total cost, and residential care accounted for 56% of the psychiatric costs.
Other relevant findings
Several other findings merit discussion. First, of the original discharged sample of 590 people, 218 (37%) died between 1989 and 2002; the mean age at death was 63±15 years. Most of the deaths were from natural causes, with two recorded suicides. Second, few of these discharged state hospital patients entered homeless shelters or jails between 1989 and 2005; 14 study participants (9%) were admitted to a homeless shelter, and five (3%) were admitted to county jails.
Discussion
These data show that the cost of community care has remained fairly stable over the past decade for former residents of Philadelphia State Hospital. Cost estimates, using the consumer price index for 2002, were $78,773 in 1992 compared with $85,850 for a similar package of services in 2002. According to the 2002 national expenditure report on state hospital costs, the yearly estimate for adults in civil status units is $162,790 ( 27 ). However, this figure reflects the cost of both long-stay patients and acute care patients, who continue to be treated in many state hospital facilities. A more appropriate comparison for long-stay patients would be that of a nursing home facility, which, on the basis of our analysis of Medicaid data for study participants, ranged from $50,370 for regular nursing home care to $87,235 for skilled nursing home care in 2002.
Comparing current data with results of our previous study, we found that the annual rate of psychiatric hospitalization decreased from 30% in 1992 to 18% in 2002; over this period the cumulative annual length of stay fell from 76.2±83 to 59.6±69.8 days per year ( 1 ). One explanation that might account for reduced inpatient use is that positive psychiatric symptoms, such as hallucinations and bizarre behavior, are thought to decline with age ( 31 ).
Noteworthy is the fact that our findings do not show that the closure or downsizing of state hospitals has resulted in significant homelessness or incarceration among former patients. It is more likely that short stays in acute care hospitals and a lack of follow-up or transitional housing for patients leaving an inpatient facility is the cause of shelter use. With respect to jail incarceration rates, current surveys show that most persons with mental illness in jails tend to be young and to have substance abuse problems ( 32 ), whereas the sample in this study is likely to have aged out of criminal behavior activities ( 33 ). Our data do not, however, provide information on arrest rates, which are probably higher than the incarceration rates.
Two items warrant attention—the high mortality rate among discharged state hospital patients and the health care utilization of study participants. Out of the 590 individuals discharged in 1989 from Philadelphia State Hospital, 37% had died by 2002. Their mean age at death was 63±15 years (median of 67 years), which supports findings of previous research showing that persons with serious mental illness have a higher risk of dying at a younger age than the general population. A study done in Massachusetts that used data from 1989 to 1994 documented higher mortality rates in the psychiatric population served by the state mental health agency; the median age at death was 66 years, compared with 76 years in the general population ( 34 ). Although we can reasonably infer that mortality rates are higher among persons with serious mental illness, we cannot assume that deinstitutionalization is the cause, because data from a century ago found that the mortality rate among institutionalized patients was three to ten times higher than in the general population ( 35 ). Also, the standardized mortality rate for persons with schizophrenia, which is based on studies since 1934, is 1.7 to 4.2 times higher than in the general population ( 36 ).
It is interesting that the 80% access rate to outpatient medical treatment among study participants is only slightly less than the 89.5% for the general population in Pennsylvania. In fact, ambulatory visits to a physician were actually higher among study participants than in the general population—7.6±7.7 visits versus 3.83 visits per capita in Pennsylvania ( 37 , 38 ). Although this study did not show specific access problems, no information was obtained on the quality of health care. Also, given the fact that this sample has significant disease burden and an average age of 51, it is quite possible that both access to and intensity of health care should be higher. Evidence supporting this view was found in a recent pilot study of a psychiatric inpatient population in which a large proportion of undetected or unknown rates of metabolic and infectious disease was discovered. Laboratory tests showed that in a sample of 600 admitted patients, 10% had HIV, 32% had hepatitis B, 21% had hepatitis C, and 22% had high cholesterol levels ( 39 ). Given the combination of high-risk factors associated with smoking, obesity, and hypertension, as well as the high prevalence of metabolic and infectious disease that may go undetected, the risk of dying young is considerably increased. Implementing interventions that address the integration of medical and psychiatric care for psychiatric patients in a managed care environment should be a top priority of policy makers and consumers alike.
Finally, on a fiscal and organizational level, the study findings reflect the trend in reallocation of mental health dollars from inpatient to outpatient community care. On the basis of the State Mental Health Authority (SMHA) profiling system of the revenue and expenditure study by the National Association of State Mental Health Program Directors Research Institute, the share of state dollars in 1992 was almost equally divided between state hospitals and community care. By 2002 the share of community dollars was 67% of the SMHA budget ( 27 ). The use of Medicaid dollars to fund inpatient and outpatient treatment in the community has freed up SMHA community dollars to provide housing supports for discharged patients as well as for patients who have no access to long-term care beds. The shift in dollars does not appear to have decreased the scope or intensity of community care for our study sample, who continued to receive housing as well as substantial case management services and outpatient treatment.
There are several limitations regarding our cost methodology and the generalizability of our findings that require discussion. Our cost perspective includes only costs to the public system related to direct treatment and does not include expenditures related to the social welfare system, the consumer, and society. For example, welfare transfer costs of both federal and state dollars associated with Social Security Supplemental Income (SSI) were $623 a month in Pennsylvania in 2002 for consumers who were no longer institutionalized ( 40 ). Because 90% of our study sample was eligible for SSI and 10% of the dually eligible would have received Social Security Disability Insurance income as well, $10,320 a year at minimum can be added to the cost in the community. Other relevant costs not addressed in this analysis are the costs associated with homelessness and involvement in the criminal justice system and social costs associated with increased family burden resulting from the shifting of care to the community setting ( 41 ). Studies have estimated family burden to be between 1% ( 42 , 43 ) and 10% ( 44 ) of total costs.
Finally, it may not be possible to generalize these results to other populations discharged from state hospitals because the findings are based on individuals who were living in a community that has a well-funded public mental health system that provides access to comprehensive services.
Conclusions
This study provides important information for mental health policy makers who need to predict the costs associated with downsizing and closing state hospitals. More studies are needed to determine the extent to which the cost distribution across categories found in this study is generalizable to other sites. The finding that 79% of costs were associated with residential and psychiatric inpatient care should also be examined in terms of what has been spent in other locations.
Acknowledgments and disclosures
The authors report no competing interests.
1. Rothbard AB, Kuno E, Schinnar AP, et al: Service utilization and cost of community care for discharged state hospital patients: a 3-year follow-up study. American Journal of Psychiatry 156:920–927, 1999Google Scholar
2. Rothbard AB, Richman E, Hadley TR: Unbundling of state hospital services in the community: the Philadelphia State Hospital story. Administration and Policy in Mental Health 24:391–398, 1997Google Scholar
3. Rothbard AB, Schinnar AP, Hadley TR, et al: A cost comparison of state hospital vs community-based care for seriously mentally ill adults. American Journal of Psychiatry 155:523–529, 1998Google Scholar
4. Davoli JH: No room at the inn: how the federal Medicaid program created inequities in psychiatric hospital access for the indigent mentally ill. American Journal of Law and Medicine 29:15–183, 2003Google Scholar
5. Lamb RH, Weinberger LE, Gross BH: Mentally ill persons in the criminal justice system: some perspectives. Psychiatric Quarterly 75:107–126, 2004Google Scholar
6. McGrew JH, Wright ER, Pescosolido BA, et al: The closing of Central State Hospital: long-term outcomes for persons with severe mental illness. Journal of Behavioral Health Services and Research 26:246–261, 1999Google Scholar
7. Okin RL, Pearsall D: Patients' perceptions of their quality of life 11 years after discharge from a state hospital. Hospital and Community Psychiatry 44:236–240, 1993Google Scholar
8. Leff J, Trieman N, Gooch C: Team for the Assessment of Psychiatric Services (TAPS) project 33: prospective follow-up study of long-stay patients discharged from two psychiatric hospitals. American Journal of Psychiatry 153:1318–1324, 1996Google Scholar
9. Braun P, Kochansky G, Shapiro R, et al: Overview: deinstitutionalization of psychiatric patients, a critical review of outcome studies. American Journal of Psychiatry 138:736–749, 1981Google Scholar
10. Hargreaves WA, Shumway M: The future of mental health services research, in Effectiveness of Services for the Severely Mentally Ill. Edited by Taube CA, Mechanic D, Hohmann AA. Washington, DC, US Department of Health and Human Services, 1989Google Scholar
11. Barry M, Crosby C: Quality of life as an evaluative measure in assessing the impact of community care on people with long-term psychiatric disorders. British Journal of Psychiatry 168:210–216, 1996Google Scholar
12. Okin RL, Borus JF, Baer L: Long-term outcome of state hospital patients discharged into structured community residential settings. Psychiatric Services 46:73–78, 1995Google Scholar
13. Solomon P: The closing of a state hospital: what is the quality of patients' lives one year post-release? Psychiatric Quarterly 63:279–296, 1992Google Scholar
14. Harding CM, Brooks GW, Ashikaga T, et al: The Vermont longitudinal study of person with severe mental illness: I. methodology, study sample, and overall status 32 years later. American Journal of Psychiatry 144:718–726, 1987Google Scholar
15. Furlong RCS: Haven within or without the hospital gate: a reappraisal of asylum provision in theory and practice, in Asylum in the Community. Edited by Tomlinson D, Carrier J. New York, Routledge, 1996Google Scholar
16. Fisher WP, Barreira PJ, Geller JL, et al: Long-stay patients in state psychiatric hospitals at the end of the 20th century. Psychiatric Services 52:1051–1056, 2001Google Scholar
17. Amaddeo F, Beecham J, Bonizzato P, et al: The costs of community-based psychiatric care for first-ever patients: a case register study. Psychological Medicine 28:173–183, 1998Google Scholar
18. Beecham J, Hallam A, Knapp K, et al: Costing care in hospital and in the community, in Care in the Community: Illusion or Reality. Edited by Leff J. New York, Wiley, 1997Google Scholar
19. Fioritti A, Russo LL, Melega V: Reform said or done? The case of Emilia-Romagna within the Italian psychiatric context. American Journal of Psychiatry 154:94–98, 1996Google Scholar
20. Fisher WH, Simon L, Geller JL, et al: Case mix in the "downsizing" state hospital. Psychiatric Services 47:255–262, 1996Google Scholar
21. Girolamo DG, Mors O, Rossi G, et al: Admission to general hospital psychiatric wards in Italy: 1. a comparison between two catchment areas with differing provision of outpatient care. International Journal of Social Psychiatry 34:248–257, 1988Google Scholar
22. Girolamo DG, Mors O, Grandi L, et al: Admission to general hospital psychiatric wards in Italy: 2. inpatient characteristics. International Journal of Social Psychiatry 34:258–266, 1988Google Scholar
23. Knapp M, Beecham J, Anderson J, et al: The TAPS Project 3: predicting the community costs of closing psychiatric hospitals. British Journal of Psychiatry 157:661–670, 1990Google Scholar
24. Leff J, Dayson D, Gooch C, et al: Quality of life of long-stay patients discharged from two psychiatric institutions. Psychiatric Services 47:62–67, 1996Google Scholar
25. Tansella M, Balestieri M, Meneghelli G, et al: Trends in the provision of psychiatric care 1979–1988, in Psychological Medicine: Community Based Psychiatry: Long-Term Patterns of Care in South Verona. Edited by Tansella M. Cambridge, United Kingdom, Cambridge University Press, 1991Google Scholar
26. Rothbard B, Schinnar AP, Hadley TR, et al: Integration of mental health data on hospital and community services. Administration and Policy in Mental Health 18:91–99, 1990Google Scholar
27. Lutterman T, Hollen V, Shaw R: Fiscal Year 2002 Revenues and Expenditures Study Report. Alexandria, Va, National Association of State Mental Health Program Directors Research Institute, 2004. Available at www.nri-inc.org/reportspubs/Google Scholar
28. Edward K et al vs John White, Jr, et al. Stipulation of Settlement in US District Court for the Eastern District of Pennsylvania. CU-88-3358, 1988Google Scholar
29. Hadley TR, Turk R, Vasko S, et al: Community treatment teams: an alternative to state hospital. Psychiatric Quarterly 68:77–90, 1997Google Scholar
30. Mueser KT, Drake RE, Wallach MA: Dual diagnosis: a review of etiological theories. Addictive Behaviors 23:717–734, 1998Google Scholar
31. Schultz SK, Miller DD, Oliver SE, et al: The life course of schizophrenia: age and symptom dimensions. Schizophrenia Research 23:15–23, 1997Google Scholar
32. Cuellar AE, Snowden LM, Ewing T: Criminal records of persons served in the public mental health system. Psychiatric Services 58:114–120, 2007Google Scholar
33. Fisher WH, Roy-Bujnowski KM, Grudzinskas AJ, et al: Patterns and prevalence of arrest in a statewide cohort of mental health care. Psychiatric Services 57:1623–1628, 2006Google Scholar
34. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036–1042, 1999Google Scholar
35. Ban TA: Neuropsychopharmacology and the genetics of schizophrenia: a history of the diagnosis of schizophrenia. Progress in Neuropsychopharmacology and Biological Psychiatry 28:753–762, 2004Google Scholar
36. Felker B, Yazel JJ, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356–1363, 1996Google Scholar
37. County Profiles, 2002. Harrisburg, Pennsylvania Health Care Cost Containment Council, 2002. Available at www.phc4.org/ambulatorysurgeryGoogle Scholar
38. Machlin SR, Sommers JP: Estimates of Health Care Expenditures for the 10 Largest States, 2002. Statistical Brief 69, Medical Expenditure Panel Survey. Washington DC, Agency for Healthcare Research and Quality, Feb 2005. Available at http://www.meps.ahrq.gov/mepsweb/datastatsGoogle Scholar
39. Rothbard AB, Blank MB, Staab JP, et al: Identifying and treating metabolic syndrome and infectious disease among psychiatric inpatients: Crisis or opportunity? A report to Eli Lilly. Philadelphia, University of Pennsylvania, Center for Mental Health Policy and Services Research, Feb 2007Google Scholar
40. Provider News. Harrisburg, Pennsylvania, Community Providers Association, Dec 2006. Available at www.paproviders.org/Pages/PNArchive/PN122006.pdfGoogle Scholar
41. Solomon P, Draine J: Subjective burden among family members of mentally ill adults: relation to stress, coping, and adaptation. American Journal of Orthopsychiatry 65:419–427, 1995Google Scholar
42. Weisbrod B, Test M, Stein L: Alternative to mental hospital treatment: II. economic benefit-cost analysis. Archives of General Psychiatry 37:400–405, 1980Google Scholar
43. Dickey B, Cannon N, McGuire T: The quarterway house: a two-year cost study of an experimental residential program. Hospital and Community Psychiatry 37:1136–1143, 1986Google Scholar
44. Wolff N, Helminiak TW, Diamond RJ: Estimated societal costs of assertive community mental health care. Psychiatric Services 46:898–906, 1995Google Scholar



