Predictors of Timely Follow-Up Care Among Medicaid-Enrolled Adults After Psychiatric Hospitalization
As the duration of inpatient psychiatric hospitalizations has decreased over the past several decades ( 1 , 2 ), timely follow-up care after hospital discharge has become increasingly important. Individuals who receive timely follow-up care are less likely to be readmitted ( 3 , 4 , 5 , 6 ). Those who do not utilize follow-up care services—such as outpatient mental health care, partial hospitalization, and residential treatment—are more likely to be readmitted ( 7 , 8 ). As a result, timely care after psychiatric hospitalization is one of the behavioral health quality measures in the widely used National Committee for Quality Assurance's Health Plan Employer Data and Information Set (HEDIS) ( 9 ), and a number of states have prioritized efforts to improve timely follow-up care after psychiatric hospital discharge ( 10 , 11 , 12 , 13 ).
Multiple studies have examined who is at greatest risk of not receiving timely follow-up care, and a range of predictors has been identified, including diagnosis, treatment history, and linkages with community mental health care before hospitalization ( 3 ). For example, in a single-site hospital study that included primarily publicly insured individuals, follow-up care after inpatient hospitalization was less likely for individuals with serious mental illness who were admitted involuntarily and had no history of hospitalization in a public facility ( 14 ). A population-based study of commercially insured individuals found that having a prior relationship with a mental health provider and being diagnosed as having an affective disorder were associated with higher rates of timely follow-up care ( 4 ). A study of individuals in Veterans Affairs hospitals found higher rates of follow-up care for individuals diagnosed as having posttraumatic stress disorder than for those diagnosed as having schizophrenia or major affective disorders ( 15 ). In a study of individuals in managed Medicare, African Americans were less likely than Caucasians to receive follow-up care, and there was also a positive association between length of inpatient stay and rate of follow-up care ( 16 ).
Despite the fact that Medicaid-enrolled individuals have a greater prevalence of serious psychiatric disorders and greater utilization of intensive mental health services, compared with other populations ( 17 ), we are unaware of population-level studies that have examined predictors of timely follow-up care after inpatient care for the Medicaid-enrolled population. To better understand predictors of timely follow-up care among Medicaid-enrolled individuals and to determine whether predictors are comparable with those of individuals not enrolled in Medicaid, this study explored factors associated with timely follow-up care among Medicaid-enrolled adults. We also examined whether there is significant variation in rates of follow-up care by discharging hospital after controlling for patient characteristics. Given the findings in studies of non-Medicaid populations, we hypothesized that higher rates of follow-up care would be seen among Caucasians, individuals who had had mental health treatment before inpatient hospitalization, individuals voluntarily admitted to the hospital, and individuals who had longer inpatient stays.
Methods
Sample and data source
Using administrative claims data from the largest Medicaid-managed behavioral health organization in a large mid-Atlantic state, we identified 6,730 adults who were aged 18–64 years and were discharged from psychiatric hospitals between January 1, 2004, and December 31, 2005. For individuals with multiple psychiatric admissions, we selected their first psychiatric hospitalization for which there was no readmission within 30 days of discharge.
Variables
We defined follow-up care as any Medicaid-reimbursed specialty behavioral health service received by the individual after the last day of the psychiatric hospitalization. These services include outpatient mental health and substance use services, partial hospital care, family based therapy, and community-based care—for example, assertive community treatment.
We obtained sociodemographic variables, such as age, gender, Medicaid eligibility category, and race, from the state's membership and eligibility files. Race-ethnicity was categorized as Caucasian, African American, or other. Consistent with other analyses that include Medicaid-enrolled individuals ( 18 ), our analysis categorized individuals on the basis of their eligibility criteria, such as income—for example, Temporary Assistance to Needy Families (TANF) or Categorically Needy (CATN) ( 19 )—or medical or mental health disability—for example, Supplemental Security Income (SSI) or Supplemental Security Income With Medicare (SSIM) ( 20 ). Individuals were categorized as having comorbid mental health and substance use disorders if they had a diagnosis of drug or alcohol abuse or dependence on any claim in the year before their index admission in addition to having a mental health diagnosis. Individuals were categorized as living in an urban area if their county of residence had a population density greater than 1,000 individuals per square mile.
Individuals were categorized as being in clinical treatment if in the 30 days before their psychiatric hospitalization they had at least one outpatient or community-based treatment service. They were categorized as receiving case management services if they had at least one case management contact in the 30 days before their psychiatric hospitalization. We identified individuals involuntarily admitted to their index hospitalization and individuals discharged from their index hospitalization against medical advice by using care manager records, and we determined the length of their index hospitalization by using claims data.
Analyses
We conducted univariate and bivariate analyses to examine the relationship between seven- and 30-day follow-up care and race, Medicaid eligibility category, age, gender, presence of comorbid substance use disorders, prior treatment, hospital admission and discharge status, and length of stay. We conducted multiple logistic regression analyses to examine the relationship between seven- and 30-day follow-up care (each coded as 0 or 1 depending on whether the participant had a follow-up visit by seven or 30 days, respectively) and our sociodemographic and clinical predictor variables, including race, Medicaid eligibility category, age, gender, presence of a comorbid substance use disorder, prior treatment, hospital admission and discharge status, and length of stay. Both models converged and discriminated reasonably well. The seven-day follow-up model c statistic was .70 with an overall prediction accuracy of 70%, and the 30-day follow-up model had a c statistic of .714 with an overall prediction accuracy of 67%. The likelihood ratio chi square p values for both models was less than .001. We present adjusted odds ratios (ORs) with 95% confidence intervals (CIs). We subsequently added discharging hospital to the multiple logistic models to determine whether this was a significant source of variation in rates of seven- and 30-day follow-up care. The significance of the discharging hospital variable was evaluated with Wald chi square tests. Analyses were conducted with SAS for Windows version 9.1 ( 21 ), and the study was classified as exempt by the University of Pittsburgh Institutional Review Board.
Results
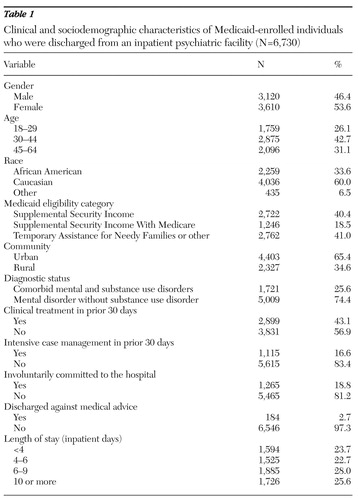
We identified 6,730 Medicaid-enrolled adults who had at least one psychiatric hospitalization during calendar years 2004 or 2005. Fifty-four percent of these individuals were women, and 34% were African American. Twenty-six percent had been identified as having a comorbid substance use disorder. More information about the sociodemographic and clinical characteristics of the population are presented in Table 1 .
 |
Approximately one-third (N=2,037, 30%) of hospitalized adults had follow-up behavioral health specialty care within seven days of discharge; 49% (N=3,280) had such follow-up care within 30 days. Of individuals receiving follow-up care within 30 days, outpatient mental health services were the most common initial follow-up care received by individuals (N=1,775, 54%). Twenty percent of individuals (N=670) initially had a medication management visit as follow-up care, 12% (N=391) first received follow-up care at a partial hospital, 10% (N=314) first received outpatient substance abuse treatment, and 4% (N=115) were first seen by an assertive community treatment team.
The strongest predictor of seven- or 30-day follow-up care was receiving clinical treatment in the month before admission. Individuals who had been in treatment were over three times as likely to receive follow-up care within seven days of discharge, and almost four times as likely to receive follow-up care within 30 days of discharge ( Table 2 ). Individuals who had received case management services in the month before admission were also significantly more likely to receive follow-up care within seven days and within 30 days than were individuals whose hospitalization exceeded nine days. African Americans, persons who were discharged against medical advice, those with a comorbid substance use disorder, or those who were enrolled in SSIM were significantly less likely than other individuals to receive seven- or 30-day follow-up care ( Table 2 ). We also found that individuals living in rural areas and those involuntarily admitted to the hospital were less likely than others to have follow-up care within seven days, but we found that these differences disappeared by 30 days ( Table 2 ).
 |
In examining the relationship between discharging hospital and timely follow-up care, controlling for individuals' sociodemographic and clinical characteristics, we found that discharging hospitals were significantly associated with rates of seven-day follow-up care (Wald χ2 =8.61; df=1, p< .01), but there was not a significant association with rates of 30-day follow-up care. When the analysis controlled for individual characteristics, the OR for seven-day follow-up care differed threefold between the top-performing discharging hospital, for which 45% of discharged individuals received follow-up care within seven days (OR=1.68, 95% CI=1.22–2.33), and the lowest-performing discharging hospital, for which 23% of discharged individuals received follow-up care within seven days (OR=.47, 95% CI=.30–.76).
Discussion
We found that almost 30% of Medicaid-enrolled adults received follow-up care within seven days of discharge from psychiatric hospitalization and that within 30 days of discharge, 49% of individuals had at least one follow-up visit. Better understanding of predictors of timely follow-up care will allow better targeted interventions designed to improve rates of timely follow-up care. Because such follow-up care has been shown to be associated with lower rates of readmissions in several studies ( 3 , 7 , 8 ), such targeted interventions have the potential of enhancing the continuity of care and reducing unnecessary hospital readmissions.
There have been few studies of predictors of follow-up care after psychiatric hospitalization in publicly insured populations. Methodological differences in qualifying follow-up services and population eligibility make direct comparisons of findings in these studies and the more widely available HEDIS numbers difficult. For example, the HEDIS rates of seven-day follow-up care for the Medicaid population included in our analyses ranged from 43% to 51% (greater than our 30% follow-up rate). This is somewhat higher than the national average (39%) for Medicaid plans reporting HEDIS data ( 22 ). Moreover, the HEDIS rate for seven-day follow-up care for our population exceeds the 39% reported by health plans for individuals in Medicare, but it is lower than the 56% HEDIS rate reported by commercial health plans. Although HEDIS rates provide a useful point of comparison across reporting health plans, clinicians and policy makers may find that more refined approaches to calculating follow-up rates (for example, separating children and adolescents from adults) are more useful in targeting the interventions.
Individuals in mental health treatment before hospitalization have been shown to be more likely to receive follow-up care ( 4 ). We also found that rates of follow-up care at seven days were substantially higher for individuals in treatment before hospitalization (46%) than they were for individuals who had not been in treatment (18%). In fact, after the analyses controlled for other factors, individuals in treatment before hospitalization were three to four times more likely to have timely follow-up care than individuals who were not in treatment. The magnitude of this difference is substantially greater than for the other factors that we were able to examine and suggests that individuals who are not in treatment before psychiatric hospitalization may require unique and novel strategies to successfully enhance the likelihood of their receiving timely follow-up care.
Others have found that individuals with co-occurring substance use disorders are at risk of poor rates of follow-up care after discharge from inpatient hospitalization ( 23 ). Engaging and retaining individuals with co-occurring disorders in follow-up care can be challenging ( 23 , 24 ), and individuals with such disorders may be at higher risk of readmission because they have not received timely follow-up care ( 25 ). The difficulties in providing high-quality care for individuals with comorbid mental health and substance use disorders may be exacerbated by fragmentation and poor coordination between the substance abuse and mental health care delivery systems. Thus experts have called for greater integration of mental health and substance abuse care to improve the quality of behavioral health care for such individuals ( 26 , 27 ).
Individuals in rural communities were significantly less likely than those in more urban communities to receive follow-up care within seven days, but the difference between these two groups did not remain at 30 days. This difference suggests that individuals in rural areas may have greater difficulty in seeing a provider right away for follow-up care but that they can be accommodated within several weeks. Studies of behavioral health services in rural areas have repeatedly documented an insufficient mental health workforce and difficulty in accessing mental health services ( 28 , 29 , 30 ). Special efforts may be necessary in rural areas to facilitate access for individuals who need to receive follow-up care immediately after hospital discharge.
Consistent with our results, other studies have found lower rates of follow-up care among individuals involuntarily admitted to the hospital ( 14 ). We also found that individuals discharged against medical advice were less likely to have timely follow-up care, possibly because they did not receive adequate and appropriate discharge planning or because optimal aftercare arrangements were not developed. Individuals involuntarily admitted to the hospital and those discharged against medical advice may be substantially less committed than other individuals to receiving mental health follow-up care, and they might be particularly appropriate candidates for programs that seek to enhance individual motivation for mental health care. Such programs have been shown to be effective in increasing engagement and retention in other populations ( 31 , 32 , 33 , 34 , 35 ).
Numerous studies have documented disparities in the access to and quality of behavioral health care received by African Americans ( 36 , 37 , 38 , 39 ), including lower rates of seven- and 30-day follow-up care ( 16 ). Despite increased attention to racial and ethnic disparities in behavioral health care and efforts to reduce these disparities in recent years ( 40 ), we found significantly lower rates of seven- and 30-day follow-up care among African Americans than in other racial or ethnic groups. Efforts to enhance rates of follow-up care among African Americans might consider addressing the cultural competency of both inpatient and outpatient providers ( 41 , 42 , 43 ), as well as other factors, such as perceived clinician empathy, which appear to influence whether individuals seek follow-up care ( 44 ).
We also found dramatic differences in the follow-up rates among discharging hospitals, after controlling for individual-level characteristics. Provider-level variation has been used to identify opportunities to improve the quality of health care services in other areas of health care ( 45 , 46 ). States, payers, consumers, and others have previously used such information to improve care by providing feedback to providers about performance on a variety of metrics ( 47 , 48 , 49 ), as well as to help identify providers or organizations that have developed novel and successful processes to improve care ( 50 ). Such approaches may also be useful in improving the behavioral health care received by individuals with mental health and substance use disorders, although the greatest impact will likely require efforts beyond simple publication of the data ( 51 ). Specifically, the approach to and quality of a hospital's discharge planning may be critically important in achieving improvements in the rates of follow-up care ( 14 , 31 ). Creative and aggressive approaches to such planning may be particularly critical for individuals with shorter hospitalizations—that is, individuals for whom we and others ( 52 ) have found lower rates of timely follow-up care and for whom there may be insufficient time in the hospital for more traditional approaches to discharge planning.
Our findings must be viewed within the context of several limitations. Our study relied primarily on administrative data. We do not know how these data correlate with patient report and medical chart abstraction data. However, Medicaid claims are subject to audit as well as edits to identify erroneous or incomplete claims at the time of submission, and published studies of the validity of Medicaid claims data have found generally high rates of agreement between medical records and claims data for both behavioral health patients ( 53 , 54 ) and physical health patients ( 55 ). Claims data also do not provide rich clinical and contextual information, such as information about socioeconomic status and other environmental factors (for example, homelessness) that are likely to be associated with follow-up rates. However, there is likely less variation in socioeconomic status among Medicaid-enrolled individuals than there is in other populations for which claims data analyses are reported, such as individuals with Medicare, commercially insured individuals, and individuals in the Department of Veterans Affairs system.
For dual-eligible Medicaid and Medicare individuals (SSIM), we may be underestimating follow-up rates, because we cannot observe services for which the provider has submitted a claim only to Medicare. Similarly, using prior claims related to substance abuse is likely to substantially underestimate the prevalence of individuals with substantial substance use disorders ( 56 ). We also did not observe services for which no claim is submitted (for example, services provided under county block grant funds, funded by charities, or for which a provider does not submit a bill), but the provision of such services is negligible in the communities in which these individuals live.
We do not know whether our findings generalize to regions where care is managed differently or where behavioral health care services for Medicaid-enrolled individuals are unmanaged; rates of follow-up care might be lower if care is unmanaged ( 57 ). We examined only the first inpatient admission during the selected time period and restricted our sample to adults, limiting our ability to compare our results with the National Committee for Quality Assurance's HEDIS quality indicators ( 58 ). We excluded from our analysis individuals readmitted within 30 days; we do not know how their inclusion might have changed the results, but we anticipate that such individuals might be less likely to have timely follow-up care. We also have no information on the quality or clinical appropriateness of claimed services.
Conclusions
Despite these limitations, better understanding of the factors associated with follow-up care among Medicaid-enrolled individuals will allow more targeted efforts to improve the continuity of care for many individuals. With the increasing use of electronic health records and comparable information technology systems in hospitals and clinical provider organizations, future research endeavors in which administrative data are linked with more robust clinical and program data will facilitate a better understanding of the factors driving utilization patterns.
With respect to interventions, prior efforts to improve follow-up rates suggest that no one approach is likely to be effective for all individuals, and our findings indicate that multiple factors, including individual characteristics, prior experiences with the behavioral health system, available outpatient treatment resources, and the discharge planning process used by discharging hospitals, may all contribute to current rates of timely follow-up care. Therefore, successful efforts will likely require multiple strategies with different approaches to improving follow-up rates and close monitoring among selected high-risk populations. These efforts may involve interventions that occur before discharge from the hospital, such as enhanced efforts to set appropriate expectations for outpatient treatment and increased attention of inpatient staff to an individual's preferences with respect to outpatient provider ( 59 , 60 ), efforts to reduce waiting lists to allow for more timely visits after discharge ( 3 ), enhancing predischarge contact between individuals who are hospitalized and outpatient providers ( 61 ), and enhancing communication between inpatient and outpatient clinicians.
System-level interventions, such as home-based visits and more aggressive case management ( 62 ), must also be considered. The development, implementation, and rigorous evaluation of feasible, acceptable, and sustainable interventions to enhance timely follow-up and subsequent engagement that build upon the existing knowledge base are sorely needed, as is the dissemination of effective practices—once these practices are identified. Because many individuals are likely to seek follow-up care from providers other than the ones to which they were referred ( 3 ), successful efforts to improve the rates of follow-up care will almost certainly require an integrated effort to implement effective practices across a range of individuals and organizations, all of whom can make an important contribution to improving the behavioral health care of consumers.
Acknowledgments and disclosures
Support for this study was provided by grant 5-P30-MH-030915-28 from the National Institute of Mental Health and the Community Care Behavioral Health Organization. The authors are indebted to Allison Guaspari, B.S., Karen Celedonia, B.S., Samantha Shugarman, M.S., and Stephanie Lonsinger, B.S., for research assistance and assistance with the preparation of the manuscript and to Susan Essock, Ph.D., Stephanie Fudurich, R.N., M.B.A., Deborah Wasilchak, M.A., Michael Jeffrey, M.S.W., Emily Heberlein, M.S., Lydia Singley, M.S.W., Kim Falk, B.S., Pat Valentine, M.S., and the consumers, providers, and other members of the Community Care's Quality Care and Management Committee for feedback on this article.
The authors report no competing interests.
1. Hudson CG: Trends in acute psychiatric inpatient care in Massachusetts. Psychiatric Services 55:1302–1304, 2004Google Scholar
2. Lieberman PB, Wiitala SA, Elliott B, et al: Decreasing length of stay: are there effects on outcomes of psychiatric hospitalization? American Journal of Psychiatry 155:905–909, 1998Google Scholar
3. Klinkenberg WD, Calsyn RJ: Predictors of receipt of aftercare and recidivism among persons with severe mental illness: a review. Psychiatric Services 47:487–496, 1996Google Scholar
4. Schoenbaum SC, Cookson D, Stelovich S: Postdischarge follow-up of psychiatric inpatients and readmission in an HMO setting. Psychiatric Services 46:943–945, 1995Google Scholar
5. Winston A, Pardes H, Papernik DS, et al: Aftercare of psychiatric patients and its relation to rehospitalization. Hospital and Community Psychiatry 28:118–121, 1977Google Scholar
6. McCranie EW, Mizell TA: Aftercare for psychiatric patients: does it prevent rehospitalization? Hospital and Community Psychiatry 29:584–587, 1978Google Scholar
7. Nelson EA, Maruish ME, Axler JL: Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatric Services 51:885–889, 2000Google Scholar
8. Cuffel BJ, Held M, Goldman W: Predictive models and the effectiveness of strategies for improving outpatient follow-up under managed care. Psychiatric Services 53:1438–1443, 2002Google Scholar
9. Health Plan Employer Data and Information Set 2007: Vol 2. Washington, DC, National Committee for Quality Assurance, 2006Google Scholar
10. 2005–2006 External Quality Review Technical Report for Health Maintenance Organizations (HMOs). Phoenix, Ariz, State of Nevada Division of Health Care Financing and Policy, 2006Google Scholar
11. Oregon Health Plan's Mental Health Care: 2005 External Quality Review Annual Report. Portland, Oreg, Office of Mental Health and Addiction Services, 2005Google Scholar
12. New York State HMO Report Card. Lake Success, NY, New York State Health Accountability Foundation, 2000Google Scholar
13. Commonwealth of Pennsylvania Follow-Up After Hospitalization for Mental Illness External Quality Review Project. Lake Success, NY, Island Peer Review Organization, 2006Google Scholar
14. Boyer CA, McAlpine DD, Pottick KJ, et al: Identifying risk factors and key strategies in linkage to outpatient psychiatric care. American Journal of Psychiatry 157:1592–1598, 2000Google Scholar
15. Druss B, Rosenheck R: Evaluation of the HEDIS measure of behavioral health care quality: Health Plan Employer Data and Information Set. Psychiatric Services 48:71–75, 1997Google Scholar
16. Virnig B, Huang Z, Lurie N, et al: Does Medicare managed care provide equal treatment for mental illness across races? Archives of General Psychiatry 61:201–205, 2004Google Scholar
17. Adelmann PK: Mental and substance use disorders among Medicaid recipients: prevalence estimates from two national surveys. Administration and Policy in Mental Health 31:111–129, 2003Google Scholar
18. Zito JM, Safer DJ, Zuckerman IH, et al: Effect of Medicaid eligibility category on racial disparities in the use of psychotropic medications among youths. Psychiatric Services 56:157–163, 2005Google Scholar
19. 55 PA Cons Stat Section 181 (1988)Google Scholar
20. Social Security Act Section 1616, 42 USC 1382e (2007)Google Scholar
21. SAS Software, Version 9.1 of the SAS System for Windows. Cary, NC, SAS, 2004Google Scholar
22. The State of Health Care Quality 2006. Washington, DC, National Committee for Quality Assurance, 2006Google Scholar
23. Wolpe PR, Gorton G, Serota R, et al: Predicting compliance of dual diagnosis inpatients with aftercare treatment. Hospital and Community Psychiatry 44:45–49, 1993Google Scholar
24. Tsuang JW, Fong TW, Ho AP: Dual diagnosis and treatment compliance. Psychiatric Services 54:576, 2003Google Scholar
25. Swindle RW, Phibbs CS, Paradise MJ, et al: Inpatient treatment for substance abuse patients with psychiatric disorders: a national study of determinants of readmission. Journal of Substance Abuse 7:79–97, 1995Google Scholar
26. Watkins KE, Hunter SB, Burnam MA, et al: Review of treatment recommendations for persons with a co-occurring affective or anxiety and substance use disorder. Psychiatric Services 56:913–926, 2005Google Scholar
27. Moggi F, Ouimette PC, Finney JW, et al: Effectiveness of treatment for substance abuse and dependence for dual diagnosis patients: a model of treatment factors associated with one-year outcomes. Journal of Studies on Alcohol 60:856–866, 1999Google Scholar
28. Hauenstein EJ, Petterson S, Merwin E, et al: Rurality, gender, and mental health treatment. Family and Community Health 29:169–185, 2006Google Scholar
29. Johnson ME, Brems C, Warner TD, et al: Rural-urban health care provider disparities in Alaska and New Mexico. Administration and Policy in Mental Health 33:504–507, 2006Google Scholar
30. Rost K, Fortney J, Fischer E, et al: Use, quality, and outcomes of care for mental health: the rural perspective. Medical Care Research and Review 59:231–265, 2002Google Scholar
31. Swanson AJ, Pantalon MV, Cohen KR: Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. Journal of Nervous and Mental Disease 187:630–635, 1999Google Scholar
32. Kemp R, Kirov G, Everitt B, et al: Randomised controlled trial of compliance therapy: 18-month follow-up. British Journal of Psychiatry 172:413–419, 1998Google Scholar
33. Daley DC, Zuckoff A: Improving compliance with the initial outpatient session among discharged inpatient dual diagnosis clients. Social Work 43:470–473, 1998Google Scholar
34. Zweben A, Zuckoff A: Motivational interviewing and treatment adherence, in Motivational Interviewing: Preparing People for Change, 2nd ed. Edited by Miller W, Rollnick S. New York, Guilford, 2002Google Scholar
35. McKay MM, McCadam K, Gonzales JJ: Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal 32:353–361, 1996Google Scholar
36. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Google Scholar
37. Wang PS, Demler O, Kessler RC: Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health 92:92–98, 2002Google Scholar
38. Alegria M, Canino G, Rios R, et al: Mental health care for Latinos: inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services 53:1547–1555, 2002Google Scholar
39. Wells K, Klap R, Koike A, et al: Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry 158:2027–2032, 2001Google Scholar
40. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Washington, DC, Department of Health and Human Services, US Public Health Service, 2001Google Scholar
41. Taylor SL, Lurie N: The role of culturally competent communication in reducing ethnic and racial healthcare disparities. American Journal of Managed Care 10:1–4, 2004Google Scholar
42. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
43. Anderson LM, Scrimshaw SC, Fullilove MT, et al: Culturally competent healthcare systems: a systematic review. American Journal of Preventive Medicine 24:68–79, 2003Google Scholar
44. Gillispie R, Williams E, Gillispie C: Hospitalized African American mental health consumers: some antecedents to service satisfaction and intent to comply with aftercare. American Journal of Orthopsychiatry 75:254–261, 2005Google Scholar
45. Wennberg JE, Fisher ES, Stukel TA, et al: Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness. Health Affairs Supplement Web Exclusive:VAR5-18, 2004Google Scholar
46. O'Connor GT, Quinton HB, Traven ND, et al: Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA 281:627–633, 1999Google Scholar
47. Kiefe CI, Allison JJ, Williams OD, et al: Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA 285:2871–2879, 2001Google Scholar
48. Hermann RC, Provost S: Interpreting measurement data for quality improvement: standards, means, norms, and benchmarks. Psychiatric Services 54:655–657, 2003Google Scholar
49. Hermann RC, Palmer RH: Common ground: a framework for selecting core quality measures for mental health and substance abuse care. Psychiatric Services 53:281–287, 2002Google Scholar
50. Gawande A: The bell curve. The New Yorker, Dec 6, 2004. Available at www.insurtecinc.com/walkforgrace/files/newyorker.pdfGoogle Scholar
51. Marshall MN, Shekelle PG, Leatherman S, et al: The public release of performance data: what do we expect to gain? A review of the evidence. JAMA 283:1866–1874, 2000Google Scholar
52. Figueroa R, Harman J, Engberg J: Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatric Services 55:560–565, 2004Google Scholar
53. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69–71, 1992Google Scholar
54. Knapp PK, Hurlburt MS, Kostello EC, et al: Child sociodemographic characteristics and common psychiatric diagnoses in Medicaid encounter data: are they valid? Journal of Behavioral Health Services and Research 33:444–452, 2006Google Scholar
55. Steinwachs DM, Stuart ME, Scholle S, et al: A comparison of ambulatory Medicaid claims to medical records: a reliability assessment. American Journal of Medical Quality 13:63–69, 1998Google Scholar
56. Summary of Findings from the 2000 National Household Survey on Drug Abuse. Rockville, Md, Substance Abuse and Mental Health Service Administration, Office of Applied Studies, 2001Google Scholar
57. Merrick EL: Effects of a behavioral health carve-out on inpatient-related quality indicators for major depression treatment. Medical Care 37:1023–1033, 1999Google Scholar
58. HEDIS 3.0. Washington, DC, National Committee for Quality Assurance, 1997Google Scholar
59. Bogin DL, Anish SS, Taub HA, et al: The effects of a referral coordinator on compliance with psychiatric discharge plans. Hospital and Community Psychiatry 35:702–706, 1984Google Scholar
60. Hagan LD, Beck NC, Kunce JT, et al: Facilitating psychiatric patient follow-up: a study of transfer attrition. Journal of Clinical Psychology 39:494–499, 1983Google Scholar
61. Olfson M, Mechanic D, Boyer CA, et al: Linking inpatients with schizophrenia to outpatient care. Psychiatric Services 49:911–917, 1998Google Scholar
62. Frederick S, Caldwell K, Rubio D: Home-based treatment, rates of ambulatory follow-up, and psychiatric rehospitalization in a Medicaid managed care population. Journal of Behavioral Health Services and Research 29:466–475, 2002Google Scholar



