End-of-Life Treatment Preferences of Persons With Serious Mental Illness
Abstract
OBJECTIVE: The goal of this study was to ascertain preferences for end-of-life care among persons with serious mental illness. METHODS: The participants were 150 community-residing adults with serious mental illness. The Health Care Preferences Questionnaire was administered to obtain information about treatment preferences in response to hypothetical medical illness scenarios: use of pain medication in the case of incurable cancer and use of artificial life support in the case of irreversible coma. Participants were asked what their treatment preferences would be for an imaginary person in each scenario ("other") as well as their preferences for themselves ("self"). RESULTS: For the scenario involving pain medication for incurable cancer, most participants chose aggressive pain management even if cognition might be affected (64 percent of respondents under the "other" scenario and 66 percent under the "self" scenario). Few participants thought a doctor should provide patients with enough medication to end their life (34 percent for self and 24 percent for other). For the scenario involving irreversible coma, respondents were divided in their choice regarding life support. Approximately one-quarter said that they would prefer to immediately terminate life support (28 percent of respondents for other and 29 percent for self), and half said they would choose to turn it off after a defined period (48 percent for other and 45 percent for self). CONCLUSIONS: Persons with serious mental illness were able to designate treatment preferences in response to end-of-life health state scenarios. Future research is needed to test advance care planning methods, assess stability of choices over time, and ascertain the utility of scenario-based preferences to guide end-of-life care decisions in this population.
Medical comorbidity, which is common among persons with serious mental illness, contributes to increased disability, health care costs, and early mortality (1,2,3,4,5). Despite advances in the use of psychiatric advance directives (6,7,8,9), public mental health systems have generally neglected medical advance directives for their consumers (10). It is likely that several factors contribute to this neglect. First, mental health providers may avoid end-of-life discussions for fear of provoking a negative reaction (11). Second, providers may assume that serious mental illness impairs a person's capacity to formulate and communicate health care choices (12,13,14). Finally, case managers and other mental health clinicians lack the knowledge, training, or standard procedures needed to facilitate and support advance care planning (10).
Little is known about the end-of-life care preferences of persons with serious mental illness or about methods for facilitating completion of medical advance directives by this high-risk population. In other reports, including an article published in this issue of Psychiatric Services (10,15), we describe the Health Care Preferences Questionnaire (HCPQ) and report on consumers' attitudes, concerns, preferences, and experiences with medical advance care planning. The purpose of this article is to describe mental health care consumers' end-of-life care preferences in relation to various hypothetical medical health state scenarios.
Methods
The participants in this study were 150 clients of the Massachusetts Department of Mental Health who were 18 years of age or older. The study was conducted from November 2000 through July 2001. A detailed description of the sample and data collection methods is provided in the companion article in this issue of the journal (15).
Information about consumers' preferences was obtained by using the HCPQ. Two hypothetical health state scenarios were adapted from standard scenarios in which patients have conditions that prevent them from expressing a choice between different types of palliative care, aggressive treatments, and life support (16,17,18,19,20,21,22,23,24,25,26). These scenarios were supplemented with questions derived from the Quest to Die With Dignity (27), an instrument used to analyze values, opinions, and attitudes concerning end-of-life care. We anticipated that hypothetical health state scenarios would enable us to learn about the advance care planning preferences of persons with serious mental illness, as they have for the general population (23,24,25,26).
The two scenarios used in the HCPQ include terminal metastatic cancer with terrible pain and total paralysis with irreparable brain damage. Interviewers read a scenario involving an imaginary patient and asked the study participant to select a treatment choice for this person. Participants were then asked to consider what treatment they would want for themselves in the same situation. A total of 140 participants (93 percent) reported treatment preferences for the imaginary person, and 141 (94 percent) reported treatment preferences for themselves.
The scenarios were preceded by assessments of health status and advance care planning and were followed by assessments of beliefs, values, and end-of-life concerns, as well as interview feedback and follow-up. The HCPQ also contains a psychiatric health state scenario. Because this scenario addresses psychiatric advance directives as distinct from medical advance directives, participants' preferences in this regard are not reported here.
Scenario-based treatment preferences were examined by using chi square analyses and logistic regressions. The logistic regressions examined predictors of congruence between responses to the "self" and "other" scenarios as well as predictors of end-of-life health care preferences. A correlation matrix was used to identify demographic, clinical, functional, advance directive, and end-of-life care preference variables that accounted for variance in dependent variables. Variables associated with significant variance were used as independent variables in regression models. Highly intercorrelated variables were removed from the analysis.
Results
As reported in our other article in this issue (15), 67 participants (45 percent) were women, and 137 (91 percent) were white. The mean±SD age of the sample was 42.0±10.4 years. The participants had predominantly been educated through high school or beyond (116 participants, or 77 percent), and most had never married (129 participants, or 86 percent). Primary diagnoses included schizophrenia or other psychosis (99 participants, or 66 percent), mood disorders (major depression and bipolar disorder) (42 participants, or 28 percent), and other disorders (personality disorders or posttraumatic stress disorder) (nine participants, or 6 percent). Ninety participants (60 percent) had at least one medical illness that required ongoing treatment.
Preferences for end-of-life care
Table 1 summarizes the participants' end-of-life care preferences under the scenario of terrible pain from terminal metastatic cancer. Most participants indicated a preference for pain medication even if it caused confusion or an inability to communicate (92 participants, or 66 percent). Nearly two-thirds of respondents endorsed this level of pain medication for the imaginary person as well (90 participants, or 64 percent). Among participants who responded to this scenario, nearly two-fifths (55 participants) expressed concern about addiction to the pain medication (data not shown).
The second part of the cancer scenario describes a patient who asks the doctor "to give him enough pain medicine to die by overdose." Most participants indicated that the doctor should not comply with this request (93 respondents, or 66 percent, under the "self" scenario and 107 respondents, or 76 percent, under the "other" scenario). However, participants were more likely to indicate a preference for an overdose for themselves on request (48 respondents, or 34 percent) than to honor the request of an imaginary person (34 respondents, or 24 percent).
A logistic regression model indicated that preference to receive pain medication that could cause confusion or an inability to communicate was positively associated with age (odds ratio [OR]=1.05, 95 percent confidence interval [CI]=1.01 to 1.10) and negatively associated with a concern about addiction (OR=.29, CI=.13 to .64). In contrast, a logistic regression model indicated that the preference to receive a medication overdose designed to end life was positively associated with a preference for medication that may cause confusion or an inability to communicate (OR=2.62, CI=1.11 to 6.18), a belief that other people should make decisions for a terminally ill person (OR=2.89, CI=1.05 to 7.90), and a preference for the immediate termination of life support (OR=2.30, CI=1.02 to 5.19).
Respondents' preferences under the scenarios of irreversible brain damage and the decision of whether to end life support are summarized in Table 2. The participants selected from terminating life support immediately, waiting for a defined period for a change to be detected (seven days or 30 days), indefinite use of life support, or other. Participants who responded "other" provided additional information about this preference and usually indicated "I don't know" (nine respondents). "I don't know" responses were coded as indefinite use of life support. More than two-fifths of respondents (61 respondents, or 43 percent, under the "self" scenario and 64 respondents, or 45 percent, under the "other" scenario) endorsed waiting a defined period. The remainder were nearly equally distributed between terminating life support immediately (40 respondents, or 28 percent, for self and 38 respondents, or 27 percent, for other) and waiting indefinitely (40 respondents, or 28 percent, for self and 39 respondents, or 28 percent, for other).
Participants gave nearly identical reasons for life support choices in relation to both the imaginary person and themselves. Among those who said that they would terminate life support immediately, 20 (48 percent) cited absence of quality of life, loss of personhood, and not wanting to be dependent on a machine or in a vegetative state. Another eight respondents (19 percent) said they did not want to prolong life, that it was "in God's hands," or that one should let nature take its course. Among participants who said that they would wait for a defined period, the most common reason was to allow time for a medical change or a "miracle" (33 respondents, or 48 percent). Finally, of participants who said that they would prolong life support indefinitely, 12 (33 percent) said that everyone deserves to live as long as possible, and an additional seven (19 percent) wanted to allow time for clinical changes or "miracles."
A logistic regression model indicated that the preference to terminate life support immediately (as opposed to waiting for at least one week) was not predicted by participant characteristics. In contrast, the preference to remain on life support indefinitely (as opposed to terminating life support immediately or waiting up to 30 days in order for a change to be detected) was positively associated with the mental health component of the Short Form-12 (SF-12) (OR=1.06, CI=1.02 to 1.10) and negatively associated with presence of a mood disorder (depression or bipolar disorder compared with other disorders) (OR=.25, CI=.08 to .79).
Congruence
Congruence for the imaginary other person and for the respondent him- or herself was high for both health state scenarios. For the scenario of terrible pain due to incurable cancer, 122 respondents (87 percent) expressed similar preferences for themselves as for an imaginary other person with respect to increasing medication despite confusion and an inability to communicate. Among individuals with noncongruent responses, preferences were split between wanting the medication for themselves but not the imaginary person (ten respondents) and wanting the medication for the imaginary person but not for themselves (eight respondents). In the scenario describing a request for medication overdose to end life, 123 respondents (87 percent) had congruent responses for themselves and for the imaginary other person. However, most individuals with noncongruent responses said that they would choose the overdose for themselves but not for another person (11 respondents), whereas only two said that they would choose it for another person but not for themselves.
Logistic regression models indicated that congruence on the question about taking medication even if it caused confusion was positively predicted by congruence on the question about medication overdose (OR= 6.51, CI=1.91 to 22.24). Congruence on medication overdose was predicted by congruence on taking medication despite its causing confusion (OR= 21.55, CI=3.54 to 131.68) and by a lower mental component score on the SF-12 (OR=.88, CI=.81 to .96).
For the scenario involving total paralysis, brain damage, and little chance of recovery, 121 participants (86 percent) identified congruent life support preferences for themselves and the imaginary person. Among individuals whose responses were noncongruent, preferences were evenly split between waiting longer to terminate life support for themselves (ten respondents) and waiting longer to terminate life support for the imaginary other person (ten respondents). Congruent responses were predicted by older age (OR=1.07, CI=1.01 to 1.13) and the presence of a mood disorder (OR=9.70, CI=1.21 to 77.72).
Distress in response to the scenarios
Follow-up information was obtained for 26 of the 29 participants who reacted negatively to at least one of the questions on the HCPQ. The question about terminal cancer distressed seven of these participants, and all the questions distressed five participants. In addition, distress was associated with the psychiatric scenario (eight participants), the entire interview (two participants), concerns pertaining to death or development of a terminal illness (two participants), questions associated with trusting one's physician (one participant), and health care proxy issues (one participant).
Six participants terminated the interview before completion because of distress. Of these participants, two terminated the interview during the question about terminal cancer, two terminated during the question about life support, and two terminated after completing the three HCPQ health state scenarios.
None of the distressed participants required crisis intervention or experienced a psychiatric decompensation. One participant accepted supportive counseling after abruptly terminating the interview, responded well, and was reassessed the next day. No additional interventions were needed.
Discussion
Obtaining advance directive preferences by using hypothetical scenarios has been promoted as practical and feasible in a variety of populations. The study reported in our companion article in this issue of the journal (15) suggests that mental health consumers are able to respond to difficult end-of-life questions with modest distress and few omissions. Although the scenarios distressed some participants, and six terminated their participation in the study at that point, none of these individuals experienced ongoing deleterious effects. This finding should help allay concerns that end-of-life care discussions will provoke serious negative reactions among persons with mental illness. Our results support the limited published findings that mental health consumers are able to participate in advance care planning for complex and potentially distressing future situations, such as identifying preferences for psychiatric hospitalization and treatments (11,28,29,30).
Components of the HCPQ that cover health status, psychiatric and medical conditions, and experience with advance care planning preceded the reading of the hypothetical scenarios. The advance care planning component includes questions about the designation of a health care proxy and the situations in which a proxy would be activated ("in case you become too sick to make medical decisions yourself" and "to communicate your health care decisions if you cannot communicate for yourself"). Because participants could question any item that they did not understand, the preceding topics may have prepared them for thinking about the end-of-life scenarios. Other authors who used scenarios to assess treatment preferences noted improvements in understanding and comfort by offering the opportunity to ask questions (31,32). In addition, those who have investigated the decision-making capacity of people with serious mental illness have also noted improvements in understanding when participants are allowed to ask questions (33,34). Recent work supports our impression that persons with serious mental illness have the cognitive capacity to respond to written scenarios (35).
We found that persons with serious mental illness frequently endorsed the same treatment options for an imaginary person as for themselves (in 83 to 88 percent of the situations described). Indicating preferences for complex, ambiguous, and emotionally difficult decisions (36) that do not require the situation to be immediately personal may be easier for participants than indicating such preferences for themselves. Presenting an imaginary situation might allow the participant to first conceptualize the situation as a story. This approach offers participants the opportunity to ask questions about the scenario and answer potentially upsetting questions about treatment choices for some unknown detached person before considering the same choices for themselves.
Individuals who were older, who had lower (worse) mental component scores on the SF-12, and who had a mood disorder were the most likely to provide congruent responses to the scenarios. Reich (37) and Andersen and colleagues (38) described decreased latency response among depressed people who were asked to predict whether positive or negative events would happen to an "average person" or to themselves. They attribute the congruence in their sample of patients with depression as representative of a depressed cognitive schema. Careful research is needed to determine whether the high congruence we observed in HCPQ responses in the subgroup of respondents who had mood disorders and lower mental component scores on the SF-12 can be attributed to decreased response latency caused by depression.
Sixty-six percent of the participants in our study said that they would choose to have pain medication administered in the case of advanced, incurable cancer with terrible pain, even if it caused them "to become confused or unable to communicate," and less than 40 percent expressed concern about becoming addicted. The preference to receive pain medication was associated with older age and with a lack of concern about addiction. In a survey of adults who were asked about taking strong pain medication in the context of terminal cancer, 49 percent were concerned about "the possibility of mental confusion," and 37 percent expressed concern "about the possibility of addiction" (39).
The physician's role in hastening or causing death was unsupported by a majority of the participants in our study (66 percent under the "self" scenario and 76 percent under the "other" scenario). Only one-third (34 percent) affirmed that they would want a physician to respond to a request to provide "enough medicine to die by overdose," and fewer (24 percent) affirmed this option for the imaginary other person. Studies of the general population reveal different results. For example, in one study 2,203 respondents (49 percent) agreed with the statement, "In case of a fatal illness a doctor should help the person end his or her life" (40). In other studies of the general population, respondents said that they would not choose physician-assisted suicide for themselves but that they would not take away someone else's right to make that choice (27).
We also found conservative preferences for terminating artificial life support among persons with serious mental illness. In contrast to findings from a survey of the general population, in which 48 percent of persons reported that they would discontinue artificial life support in a case of coma from irreversible head trauma (41), only 29 percent of our study participants said that they would do so. On the other hand, 71 percent of our participants said that they would choose to prolong artificial life support temporarily or permanently to "allow time for a possible miracle" or because people "deserve to live as long as possible."
Although these response rates are different from those of Caucasians in the general population, the choices are similar to those expressed by some racial or ethnic groups. African Americans, Latinos, and Haitians often choose to continue aggressive treatments, including artificial life support, when the prognosis is poor (42,43,44,45). Disparities in access to health care, quality of care, and delivery of services underlie distrust in health care in minority populations (46,47) and contribute to a hesitancy to discontinue intensive treatments. Persons with serious mental illness experience similar health care disparities (48,49) and may be influenced by similar feelings.
Although our study begins to address the feasibility of identifying end-of-life care preferences among persons with serious mental illness, it had several limitations. First, the study sample was small and was not culturally diverse. Second, the respondents were not randomly selected. Third, there was no comparison group. Fourth, the precise text of the scenarios was altered from that of standard advance care planning scenarios. Fifth, our methods of using scenarios for an imaginary other person and for the respondent him- or herself was not informed by relevant psychological theory (50). Finally, the follow-up was clinical and was limited to individuals who expressed a great deal of distress. Universal follow-up would have strengthened the study by providing data about advance directive completion rates and participant well-being. Thus the results should be interpreted with caution.
Despite these limitations, this is the first report we are aware of that describes end-of-life treatment preferences of a sample of persons with serious mental illness. Support for the findings requires studies of health state scenarios that have adequate power to evaluate well-defined subgroups, such as psychiatric disease, race, age, religion, health status, and methods for measuring the stability of preferences over time. The general population (51,52) and persons with serious mental illness (53) are receptive to advance care planning, although rates of completion of advance directives are low. Important barriers include consumers' concerns and misconceptions (54); lack of knowledge, education, experience, and comfort among practitioners (55); discordance between the patient, the family member or proxy, and the provider; and concerns about providers' compliance with directives (56). Potential benefits include promoting individual autonomy and empowerment; enhancing communication between patients, family members, and health care providers; and protecting individuals from receiving unwanted treatments at a time when they cannot make or communicate their own treatment decisions. Consumers are supportive of advance directives, and their participation is critical for the development and implementation of needed education, research, policies, and best practices.
Conclusions
In this study, mental health consumers were able to engage in medical advance care planning through hypothetical health state preference scenarios. In a scenario involving incurable cancer, nearly two-thirds of individuals with serious mental illness indicated preferences for aggressive pain management, even if it would impair cognition, and one-third indicated preferences for receiving a medication overdose in order to end their life. Moreover, nearly half of participants indicated that they would prefer to receive life support for a defined period, and the remainder was split between immediately terminating life support and maintaining it indefinitely.
Because persons with serious mental illness die at a younger age than the general population, it is important to begin discussions about advance directives with them as outpatients, as has been recommended for the general population (57,58). Regular review of proxy designations and medical and psychiatric treatment preferences will improve communication and empower consumers, family members, and significant others. Our suggested intervention includes obtaining information about medical and psychiatric preferences, values (59), beliefs, and health care proxy designation coupled with the flexibility to complete the directive at once or in parts. Documentation of end-of-life care preferences and inclusion of preferences in medical and case management records can support future decision making for guardians, proxies, family members, and practitioners at a time when a consumer is unable to make or communicate his or her own health care decisions.
Acknowledgments
This study was funded by grant 35497 from the Robert Wood Johnson Foundation through the Promoting Excellence in End-of-Life Care Program. The authors thank Steve Carreras, Ph.D., Anna Rubley, L.I.C.S.W., Meredith Hanrahan-Boshes, R.N., Sally Neylan Okun, B.S.N., M.M.H.S., Andrea Miller, Ed.M., M.S., and Babs Fenby, Ph.D., for their assistance in identifying participants, conducting interviews, and collecting data for the study.
Dr. Foti and Dr. Fletcher are affiliated with the department of psychiatry of the University of Massachusetts Medical School in Worcester. Dr. Foti is also State Medical Director with the Massachusetts Department of Mental Health in Boston. Dr. Bartels and Ms. Van Citters are affiliated with the New Hampshire-Dartmouth Psychiatric Research Center in Lebanon, New Hampshire. Dr. Bartels is also with the department of psychiatry of Dartmouth Medical School in Hanover, New Hampshire. Dr. Merriman is with the Nursing School of the University of Miami and with Touchstone Consulting in North Bay Village, Florida. Send correspondence to Dr. Foti at the Massachusetts Department of Mental Health, 25 Staniford Street, Boston, Massachusetts 02114-2503 (e-mail, [email protected]).
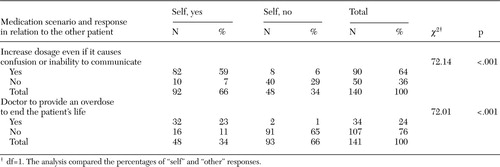 |
Table 1. Preferences for use of pain medication in the case of incurable cancer, both for an imaginary other patient and for the respondent (self), among persons with serious mental illness
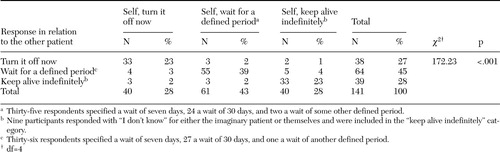 |
Table 2. Preferences for life support in the event of brain damage with little chance of recovery, both for an imaginary other patient and for the respondent (self), among persons with serious mental illness
1. Brown S, Inskip H, Barraclough B: Causes of the excess mortality of schizophrenia. British Journal of Psychiatry 177:212–217, 2000Crossref, Medline, Google Scholar
2. Jones DR, Macias C, Barreira PJ, et al: Prevalence, severity, and co-occurrence of chronic physical health problems of persons with serious mental illness. Psychiatric Services 55:1250–1257, 2004Link, Google Scholar
3. Newman SC, Bland RC: Mortality in a cohort of patients with schizophrenia: a record linkage study. Canadian Journal of Psychiatry 36:239–245, 1991Crossref, Medline, Google Scholar
4. Osborn DP: The poor physical health of people with mental illness. Western Journal of Medicine 175:329–335, 2001Crossref, Medline, Google Scholar
5. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036–1042, 1999Link, Google Scholar
6. Srebnik D, Appelbaum PS, Russo J: Assessing competence to complete psychiatric advance directives with the competence assessment tool for psychiatric advance directives. Comprehensive Psychiatry 45:239–245, 2004Crossref, Medline, Google Scholar
7. Backlar P, McFarland BH, Swanson JW, et al: Consumer, provider, and informal caregiver opinions on psychiatric advance directives. Administration and Policy in Mental Health 28:427–441, 2001Crossref, Medline, Google Scholar
8. Peto T, Srebnik D, Zick E, et al: Support needed to create psychiatric advance directives. Administration and Policy in Mental Health 31:409–419, 2004Crossref, Medline, Google Scholar
9. Srebnik D, Brodoff L: Implementing psychiatric advance directives: service provider issues and answers. Journal of Behavioral Health Services Research 30:253–268, 2003Crossref, Medline, Google Scholar
10. Foti ME: "Do It Your Way": a demonstration project on end-of-life care for persons with serious mental illness. Journal of Palliative Medicine 6:661–669, 2003Crossref, Medline, Google Scholar
11. Lee MA, Ganzini L, Heintz R: The PSDA and treatment refusal by a depressed older patient committed to the state mental hospital. HEC Forum 5:289–301, 1993Crossref, Medline, Google Scholar
12. Bursztajn HJ, Harding HP, Gutheil TG, et al: Beyond cognition: the role of disordered affective states in impairing competence to consent to treatment. Bulletin of the American Academy of Psychiatry and the Law 19:383–388, 1991Medline, Google Scholar
13. Freedman M, Stuss DT, Gordon M: Assessment of competency: the role of neurobehavioral deficits. Annals of Internal Medicine 115:203–208, 1991Crossref, Medline, Google Scholar
14. Jones GH: Informed consent in chronic schizophrenia? British Journal of Psychiatry 167:565–568, 1995Google Scholar
15. Foti ME, Bartels SJ, Merriman MP, et al: Medical advance care planning for persons with serious mental illness. Psychiatric Services 56:576–584, 2005Link, Google Scholar
16. Emanuel LL, Emanuel EJ: The medical directive: a new comprehensive advance care document. JAMA 261:3288–3293, 1989Crossref, Medline, Google Scholar
17. Emanuel L: The health care directive: learning how to draft advance care documents. Journal of the American Geriatrics Society 39:1221–1228, 1991Crossref, Medline, Google Scholar
18. Emanuel LL, Emanuel EJ: The medical directive, in Respecting Choices Advance Care Planning Course Facilitator's Manual. Hammes BJ, Briggs L. La Crosse, Wis, Gundersen Lutheran Medical Foundation, 1995Google Scholar
19. Sulmasy DP, Terry PB, Weisman CS, et al: The accuracy of substituted judgments in patients with terminal diagnoses. Annals of Internal Medicine 128:621–629, 1998Crossref, Medline, Google Scholar
20. Fischer GS, Alpert HR, Stoeckle JD, et al: Can goals of care be used to predict intervention preferences in an advance directive? Archives of Internal Medicine 157:801–807, 1997Google Scholar
21. Hesse KA: Terminal care of the very old: changes in the way we die. Archives of Internal Medicine 155:1513–1518, 1995Crossref, Medline, Google Scholar
22. Emanuel LL, Danis M, Pearlman RA, et al: Advance care planning as a process: structuring the discussions in practice. Journal of the American Geriatrics Society 43:440–446, 1995Crossref, Medline, Google Scholar
23. Emanuel LL, Barry MJ, Stoeckle JD, et al: Advance directives for medical care: a case for greater use. New England Journal of Medicine 324:889–895, 1991Crossref, Medline, Google Scholar
24. Emanuel LL, Barry MJ, Emanuel EJ, et al: Advance directives: can patients' stated treatment choices be used to infer unstated choices? Medical Care 32:95–105, 1994Google Scholar
25. Ditto PH, Danks JH, Smucker WD, et al: Advance directives as acts of communication: a randomized controlled trial. Archives of Internal Medicine 161:421–430, 2001Crossref, Medline, Google Scholar
26. Reinders M, Singer PA: Which advance directive do patients prefer? Journal of General Internal Medicine 9:49–51, 1994Google Scholar
27. Tyler B, Perry M, Lofton T, et al: The Quest to Die With Dignity: An Analysis of Americans' Values, Opinions, and Attitudes Concerning End-of-Life Care. Appleton, Wis, American Health Decisions, 1997Google Scholar
28. Appelbaum PS: Advance directives for psychiatric treatment. Hospital and Community Psychiatry 42:983–984, 1991Abstract, Google Scholar
29. Swisher KN: Implementing the PSDA for psychiatric patients: a common-sense approach. Journal of Clinical Ethics 2:199–205, 1991Medline, Google Scholar
30. Srebnik DS, LaFond JQ: Advance directives for mental health treatment. Psychiatric Services 50:919–925, 1999Link, Google Scholar
31. Schwartz CE, Wheeler HB, Hammes B, et al: Early intervention in planning end-of-life care with ambulatory geriatric patients: results of a pilot trial. Archives of Internal Medicine 162:1611–1618, 2002Crossref, Medline, Google Scholar
32. Hanson LC, Tulsky JA, Danis M: Can clinical interventions change care at the end of life? Annals of Internal Medicine 126:381–388, 1997Google Scholar
33. Carpenter WT Jr, Gold JM, Lahti AC, et al: Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry 57:533–538, 2000Crossref, Medline, Google Scholar
34. Jeste DV, Dunn LB, Palmer BW, et al: A collaborative model for research on decisional capacity and informed consent in older patients with schizophrenia: bioethics unit of a geriatric psychiatry intervention research center. Psychopharmacology 171:68–74, 2003Crossref, Medline, Google Scholar
35. Shumway M, Saunders T, Shern D, et al: Preferences for schizophrenia treatment outcomes among public policy makers, consumers, families, and providers. Psychiatric Services 54:1124–1128, 2003Link, Google Scholar
36. Abma TA, Widdershoven GA: Sharing stories: narrative and dialogue in responsive nursing evaluation. Evaluation and the Health Professions 28:90–109, 2005Crossref, Medline, Google Scholar
37. Reich DA, Weary G: Depressives' future-event schemas and the social inference process. Journal of Personality and Social Psychology 74:1133–1145, 1998Crossref, Medline, Google Scholar
38. Andersen SM, Spielman LA, Bargh JA: Future-event schemas and certainty about the future: automaticity in depressives' future-event predictions. Journal of Personality and Social Psychology 63:711–723, 1992Crossref, Medline, Google Scholar
39. Levin D, Cleeland CS, Dar R: Public attitudes toward cancer pain. Cancer 56:2337–2339, 1985Crossref, Medline, Google Scholar
40. Doyle D, Cleeland CS, Joranson D: Public Survey of Cancer Pain and Its Treatment. New Orleans, American Pain Society, 1991Google Scholar
41. Sjokvist P, Nilstun T, Svantesson M, et al: Withdrawal of life support: who should decide? Differences in attitudes among the general public, nurses, and physicians. Intensive Care Medicine 25:949–954, 1999Crossref, Medline, Google Scholar
42. Hopp FP, Duffy SA: Racial variations in end-of-life care. Journal of the American Geriatrics Society 48:658–663, 2000Crossref, Medline, Google Scholar
43. Jackson F, Schim SM, Seeley S, et al: Barriers to hospice care for African Americans: problems and solutions. Journal of Hospice and Palliative Nursing 2:65–72, 2000Crossref, Google Scholar
44. Kemp C: Culture and the end of life: Hispanic culture (Mexican-American). Journal of Hospice and Palliative Nursing 3:29–33, 2001Crossref, Google Scholar
45. Blackhall LJ, Frank G, Murphy ST, et al: Ethnicity and attitudes towards life sustaining technology. Social Science and Medicine 48:1779–1789, 1999Crossref, Medline, Google Scholar
46. Cort MA: Cultural mistrust and use of hospice care: challenges and remedies. Journal of Palliative Medicine 7:63–71, 2004Crossref, Medline, Google Scholar
47. Crawley LL: Palliative care in African-American communities. Innovations in End-of-Life Care 3, 2001. Available at www. edc.org/lastactsGoogle Scholar
48. Corrigan P, Thompson V, Lambert D, et al: Perceptions of discrimination among persons with serious mental illness. Psychiatric Services 54:1105–1110, 2003Link, Google Scholar
49. Lawrie SM, Martin K, McNeill G, et al: General practitioners' attitudes to psychiatric and medical illness. Psychological Medicine 28:1463–1467, 1998Crossref, Medline, Google Scholar
50. Kray LJ: Contingent weighting in self-other decision making. Organizational Behavior and Human Decision Processes 83:82–106, 2000Crossref, Medline, Google Scholar
51. Johnston SC, Pfeifer MP: The discussion about advance directives: patient and physician opinions about how and when it should be conducted. Archives of Internal Medicine 155:1025–1030, 1995Crossref, Medline, Google Scholar
52. Elpern EH, Yellen SB, Burton LA: A preliminary investigation of opinions and behaviors regarding advance directives for medical care. American Journal of Critical Care 2:161–167, 1993Medline, Google Scholar
53. Srebnik DS, Russo J, Sage J, et al: Interest in psychiatric advance directives among high users of crisis services and hospitalization. Psychiatric Services 54:981–986, 2003Link, Google Scholar
54. Tonelli MR: Pulling the plug on living wills: a critical analysis of advance directives. Chest 110:816–822, 1996Crossref, Medline, Google Scholar
55. Molloy DW, Russo R, Stiller A, et al: How to implement the "Let Me Decide'" advance health and personal care directive program. Journal of Clinical Outcomes Management 7:41–47, 2000Google Scholar
56. Glick KL, Mackay KM: Advance directives: barriers to completion. Journal of the New York State Nurses Association 29:4–8, 1998Medline, Google Scholar
57. Wenger NS, Oye RK, Bellamy PE, et al: Prior capacity of patients lacking decision making ability early in hospitalization: implications for advance directive administration. Journal of General Internal Medicine 9:539–543, 1994Crossref, Medline, Google Scholar
58. Nolan MT, Bruder M: Patients' attitudes toward advance directives and end-of-life treatment decisions. Nursing Outlook 45:204–208, 1997Crossref, Medline, Google Scholar
59. Peters C, Chiverton P: Use of a values history in approaching medical advanced directives with psychiatric patients. Journal of Psychosocial Nursing 41:28–36, 2003Google Scholar



