Effects of Residents' Depression, Sleep, and Demand for Medication on Benzodiazepine Use in Nursing Homes
Abstract
OBJECTIVE: This study sought to identify risk factors associated with the prescription and use of benzodiazepines in nursing homes and to assess the prevalence and determinants of demand for benzodiazepines among nursing home residents. METHODS: Data were available for 2,060 residents who had participated in a previous study of use of medications in 18 randomly selected nursing homes in Wisconsin between 1986 and 1989. Data sources included nursing home and pharmacy records; nurses' assessments of residents' behavior, pain, sleep, and demand for medication; and researchers' observations of resident requests for medication. Measures of benzodiazepine use included benzodiazepine prescriptions, prevalence and extent of as-needed drug use, and chronic use as defined by Health Care Financing Administration guidelines. RESULTS: A quarter of the residents received prescriptions for benzodiazepines. Of these, 71 percent received prescriptions to aid sleep or to be taken at bedtime; 32 percent used benzodiazepines for a longer period than recommended; and 26 percent requested medication. Logistic regression analysis showed that residents with depression, pain, or sleep problems were more likely to have received benzodiazepines and to have requested medication. Chronic use was significantly higher among residents with depression, sleep problems, or multiple benzodiazepine regimens and among those who requested medication. Demand and sleep problems also were associated with higher rates of any as-needed use and with higher numbers of as-needed doses used. CONCLUSIONS: Efforts to improve benzodiazepine use in nursing homes must address the need for better assessment and management of depression, sleep, pain, and residents' demand for these medications.
Although benzodiazepines can be effective in the treatment of anxiety and insomnia, prescription of these agents for elderly persons raises concerns about long-term use, dependence, loss of efficacy, and safety (1,2,3). The use of benzodiazepines is of special concern in nursing homes, because these drugs may be used regularly for long periods (4,5) and because depressed residents often receive benzodiazepines instead of antidepressants (6). Use of benzodiazepines also increases the risk of falls and hip fracture (3,7,8), cognitive impairment (9,10), and functional decline (11,12). Moreover, recent studies suggest that short-acting benzodiazepines are no safer than long-acting ones (3,7,8,10,12) and that explicit federal guidelines have not reduced the prevalence or chronic use of these drugs in nursing homes (5,13).
Previous studies have described the prevalence of anxiolytic and hypnotic drug use among nursing home residents in different countries and different types of institutions (5,1415,16,17,18,19,20). However, little is known about the reasons for use, the regimens used, and individual risk factors associated with different use patterns. Some studies have reported higher rates of prescription of anxiolytics and hypnotics for younger residents and those in certain diagnostic groups, but it is not clear whether these factors influence actual use (19). Others have examined specific regimens and individual factors associated with various patterns of use, but many of these studies have lacked information about pain, sleep, behavioral problems, and medication demand (18). It is important to examine these factors, because they influence benzodiazepine use in other settings (2,21,22,23,24) and may be helpful in designing future interventions.
This study had three aims. The first was to assess individual risk factors associated with four indicators of benzodiazepine use among residents of nursing homes who participated in an earlier study in Wisconsin (5,13,25)—prescriptions for benzodiazepines, any as-needed use, number of as-needed doses used, and chronic use. The second aim was to assess the prevalence and determinants of residents' demand for benzodiazepines —the resident's expression of need or desire for these medications. The third aim was to evaluate the benzodiazepine regimens of this sample of residents.
On the basis of previous studies (2,21,22), we hypothesized that residents with depression, pain, or sleep problems would be more likely to have received a prescription for a benzodiazepine, to have demanded and used medication, and to have used medication for longer periods than recommended. We also hypothesized that residents who demanded medication would have higher rates of as-needed drug use and of chronic use (23,24). Our control variables included age, gender, whether dementia was present, whether behavioral problems were present, payment source, and number of prescribed benzodiazepines (19,26,27,28).
Methods
Data were obtained from a study conducted between 1986 and 1989 that used random samples of nine for-profit and nine religiously affiliated skilled facilities ranging in size from 66 to 288 beds (5,13,25). Sampling procedures and characteristics of the facilities are described elsewhere (25). Administrators sought informed consent from 2,434 residents or their guardians according to an approved protocol. Of these, 2,060 participated, 257 refused, and 117 were excluded because of death, hospitalization, discharge, or relocation.
Data collection required two to three months per facility. During the first four to six weeks, researchers abstracted pharmacy and facility records to identify current drug regimens, start and stop dates, and demographic and clinical characteristics. Selected day nurses completed a resident assessment form for their unit. During a 14-day observation period that followed, researchers asked at least one evening nurse per unit to use the sleep assessment form to rate each resident's pain, sleep, and demand for medication. The observer then accompanied the nurse as he or she dispensed medications. A nurse encounter form was used to keep a running account of nurse-resident interactions, including residents' requests and comments. Researchers later audited pharmacy and nurses' records to determine drug use.
Measures of benzodiazepine use
We examined four drug use measures: having a current prescription for a benzodiazepine during the index month (coded 0 for no, 1 for yes); any use of as-needed orders for benzodiazepines during the index month (0 for no, 1 for yes); the number of as-needed doses used during the 14-day observation period; and chronic use, defined as ten or more continuous days for hypnotics and four or more continuous months for anxiolytics (0 for no, 1 for yes). These ranges are recommended by the Health Care Financing Administration (HCFA) (29) and are consistent with guidelines published by the American Psychiatric Association in 1985 (30). For descriptive purposes, we also assessed deviations from HCFA guidelines on type, number, and dosage of benzodiazepines prescribed.
Measures of residents'characteristics
Residents' demand was assessed with nurses' reports and researchers' observations. Nurses' reports of past demand were determined from two questions on the sleep assessment form. The first was "In the past month, how often did the resident want medication or something to help him or her sleep?" Possible responses were rarely, occasionally, and usually. The second question was "What (if anything) did he or she want?" Residents who wanted an anxiolytic or hypnotic drug received a score of 1, and others, 0. For interrater reliability, two nurses independently rated their residents' past demand; results showed 89.5 percent agreement.
Researchers' observations of demand were assessed by analyzing the nurse encounter forms. Demand was defined as an observable communication by a resident that indicated a perceived need or desire for an anxiolytic or hypnotic drug. To be counted as demanding a drug, the resident had to express a need or desire for a particular drug—that is, identify it by name, purpose, or physical appearance. The demand could be made in various forms and levels of intensity —for example, "I need my sleeping pill, now" or "Where's my blue pill?" Residents who approached the nurses' station or medication cart looking for their medication also were considered to be demanding that medication. Residents who demanded an anxiolytic or hypnotic drug received a score of 1, and others, 0. For interrater reliability, two researchers simultaneously observed residents on the same evening and then on two different evenings. Results showed 100 percent agreement on the same evening and 83.8 percent agreement on different evenings. Because past demand and observation of demand were related (χ2=102.3, df=1, p<.001), we combined them into one measure of demand, coded 0 for no and 1 for yes.
Residents' diagnoses were classified according to ICD-9-CM codes. We assigned scores of 0 or 1 for the absence or presence, respectively, of organic mental syndrome or dementia (codes 290 to 294, 310, or 331) and depression (codes 296, 298, or 311). Four items from the resident assessment form assessed disruptive or noisy behavior, agitation, physical aggressiveness, and resistance to care in the previous month, each coded 1 for rarely, 2 for occasionally, and 3 for usually. Items were summed to obtain a behavioral problem score from 4 to 12. For interrater reliability, two nurses independently rated their residents' behavior; item gamma values ranged from .85 to .96, and the Pearson correlation for the total score was .84.
Two items from the sleep assessment form were used to assess pain and sleep: "In the past month, how often was the resident in pain?" and "How often did the resident have difficulty sleeping?" Results were coded 1 for rarely, 2 for occasionally, and 3 for usually. Two nurses independently rated their residents' sleep and pain in the previous month; gamma values indicated acceptable to good reliability—.56 for sleep and .83 for pain.
Analysis
We described patterns of benzodiazepine prescription, deviation from HCFA guidelines, and prevalence of residents' demand. We then identified risk factors associated with residents' demand, as-needed use, and chronic use. Chi square and t tests were used for bivariate analyses, and logistic and linear regression techniques were used for multivariate analyses.
Results
Table 1 summarizes the sample characteristics and their association with prescriptions for benzodiazepines. The sample was similar to other nursing home populations. Of 2,060 residents, 75 percent were women, 51 percent were 85 years of age or older (mean±SD=82.3±10.8 years), and 58 percent were eligible for Medicaid benefits. Forty percent had dementia, and 12 percent had depression. About half (55 percent) occasionally or usually demonstrated behavioral problems, 34 percent had pain, and 31 percent had sleep problems.
Of 2,060 residents, 585 (28 percent) received prescriptions for benzodiazepines, 148 (7 percent) received prescriptions for diphenhydramine, and 47 (2 percent) received prescriptions for other anxiolytic or hypnotic drugs. Bivariate results showed that benzodiazepine prescription rates were significantly higher for residents who were under 85 years of age, those who did not have dementia, and those who had depression, pain, or sleep problems. Because these factors may be correlated, logistic regression was used for further analysis, with age, behavior, pain, and sleep problems entered as continuous variables. Factors that predicted benzodiazepine prescription were female gender (OR=1.30), age (OR=.98), depression (OR=1.68), pain (OR=1.20), and sleep problems (OR=2.23).
Table 2 summarizes the sample's benzodiazepine regimens and frequency of demand. Of 585 residents who had prescriptions for benzodiazepines, 15 percent received prescriptions for multiple benzodiazepines. About 71 percent had orders for sleep or bedtime doses, and 59 percent had as-needed orders only. For about 71 percent of the sample, prescriptions deviated from guidelines: 34 percent received a nonrecommended long-acting drug, 33 percent received an excessive dosage, and 32 percent had prescriptions for an excessive duration.
Nurses reported that 24 percent of the residents had occasionally or usually requested their medication in the previous month. Researchers observed requests from 13 percent during observed shifts. Demand of this type was reported or observed for about one in four residents (26 percent).
Table 3 presents the results of the bivariate analysis of residents' demand, as-needed use, and chronic use of benzodiazepines. Demand was significantly higher among residents under 85, those without dementia or behavioral problems, and those with depression, pain, sleep problems, or prescriptions for multiple benzodiazepines. The demand rate for residents with sleep problems was 47 percent, compared with 6 percent for other residents.
Among residents with an as-needed benzodiazepine prescription, 50 percent had used it in the previous month. Rates of as-needed use were significantly higher among residents who had pain, sleep problems, or multiple prescriptions and those who requested medication. The rate of use of as-needed medication for residents with sleep problems was 72 percent, compared with 33 percent for those without. The rate of as-needed use for those who requested medication was 83 percent, compared with 42 percent for other residents. This means that difficulty sleeping and demand for medication often resulted in use of as-needed doses, although clearly other factors were also involved in nurses' administration of as-needed medication.
The mean±SD number of as-needed doses used during the 14-day observation period was 2.6±4.9. Residents who did not have dementia used more doses than those who did. Frequency of use was also higher among residents with pain (4.0 compared with 1.7), multiple prescriptions (5.3 compared with 2.2), sleep problems (5.2 compared with .7), and demand (7.5 compared with 1.4).
Bivariate analyses identified five predictors of chronic use. Chronic use was higher among residents without dementia (50 percent compared with 42 percent) and those with depression (60 percent compared with 45 percent), multiple prescriptions (48 percent compared with 29 percent), sleep problems (43 percent compared with 22 percent), and demand (49 percent compared with 25 percent).
Table 4 presents the results of two regression models for each dependent variable. Model 1 introduced demographic characteristics, diagnoses, pain, behavioral problems, and benzodiazepine regimens; model 2 added sleep and demand variables. The adjusted odds ratios for demand were significantly lower among residents with dementia and behavioral problems and more than twice as high among residents with depression, pain, or multiple prescriptions. These factors were significant even after sleep problems were controlled for in model 2. The adjusted rate of demand was nearly five times as high among residents with sleep problems.
Rates of any use of as-needed benzodiazepines were significantly higher among residents with multiple prescriptions or behavioral or sleep problems and among those who demanded medication. Of interest, residents with depression had lower rates of use of as-needed medication use after other factors were controlled for.
Two factors predicted higher use of as-needed doses in model 1: frequent pain and multiple prescriptions. Model 2 showed that the presence of pain was nonsignificant after sleep and demand variables were added, suggesting that pain might have had an indirect effect by increasing sleep problems and demand, in turn triggering more frequent use of as-needed prescriptions. For predicting the use of as-needed doses, R2 was .12 for model 1 and .38 for model 2, which suggests that sleep problems and the demand for medication improved prediction.
The adjusted odds of chronic use were twice as high among residents with depression and multiple prescriptions. These factors remained significant even after the sleep and demand variables were added. Sleep problems and demand for medication were also significant in the final model.
To better understand benzodiazepine use, we explored the characteristics of residents who used higher doses (data not shown). Logistic regression showed that younger residents used higher doses (adjusted OR=.98, p<.05), as did residents who demanded medication (adjusted OR=2.78, p<.001). Nonsignificant effects were observed for demographic characteristics, diagnosis, pain, sleep problems, and behavioral problems.
Discussion and conclusions
This study is one of the first to examine the effects of residents' sleep and demand for medication on benzodiazepine use in nursing homes. Unlike in past studies, we analyzed nurses' records and nurse assessment forms and observation of residents' behavior. These data yielded important findings. Nearly one in three residents had sleep problems; 71 percent of benzodiazepine prescriptions were for sleep or to be taken at bedtime; one in four residents demanded medication for sleep or at bedtime; and sleep problems and demand for medication were among the strongest and most consistent predictors of as-needed and chronic drug use.
Although behavioral problems increased the odds of any use of as-needed benzodiazepines, the frequency of behavioral problems was unrelated to the number of as-needed doses used and to chronic use. Thus benzodiazepines were used primarily for sleep, not behavioral control.
The association between residents' demand and chronic use is consistent with previous investigations of demand in community and hospital settings (23,24). Unfortunately, it is difficult to determine whether demand causes chronic use or whether chronic use induces dependence, poorer sleep, and further demand (4). Prospective studies are needed to assess how chronic use develops and why some residents are more likely, after other risk factors have been controlled for, to demand their medication. It would be interesting to know how many residents were encouraged to try a drug holiday or a dose reduction and how many would have been willing to participate in a sleep hygiene program. To our knowledge, none of the study facilities had a formal sleep hygiene program at the time of data collection.
As expected, demand was significantly higher among alert residents and those with diagnosed depression and pain. We also found that depression was a risk factor for chronic benzodiazepine use and that 44 percent of residents with diagnosed depression and prescriptions for a benzodiazepine did not have prescriptions for an antidepressant. These results suggest inadequate treatment of primary problems that can induce insomnia and are consistent with past research showing that alert residents with diagnosed depression often receive benzodiazepines as the sole treatment of depression (6). If our findings and interpretations are correct, then efforts to improve the assessment and treatment of pain and depression may reduce secondary insomnia, demand for medication, chronic use, and possibly adverse events.
Although individual risk factors help explain variations in use of benzodiazepines, organizational risk factors also can influence the prevalence and appropriateness of the use of anxiolytic or hypnotic drugs in nursing homes. For example, previous studies have found significant associations between poorer nurse staffing and more extensive use of various psychoactive drugs by nursing home residents (5,13,27,28). Recent research (13) has also shown a significant link between a nursing home's treatment culture and patterns of drug use, with lower rates of antipsychotic drug use in facilities that have "resident-centered cultures" that encourage the use of nonpharmacologic interventions and interdisciplinary collaboration. Further analyses are needed to determine whether and how medication demand and other individual risk factors affect the use of benzodiazepines under these different nursing home conditions.
A major limitation of this study is that data were collected between 1986 and 1989. However, we believe the results are relevant, for several reasons. First, the prevalence of anxiolytic and hypnotic drug use in nursing homes has remained relatively constant despite regulatory efforts and the availability of newer antidepressants. Studies of drug use from 1986 to 1993 have found significant declines in the use of antipsychotic drugs but no change in the use of anxiolytics and hypnotics (5,13,19,26,31). More recent studies of drug use from 1993 to 2000 found a 20 percent increase in the use of antidepressants but again no change in the use of anxiolytics and hypnotics (15). Second, reimbursement policies, staffing, and processes of nursing home care have not changed substantially since the late 1980s. Continuous use of hypnotics remains a frequent problem (32), and contemporary facilities still lack formal sleep hygiene programs (33). Recent data on prescribing practices in primary care further demonstrate that many elderly patients with depression receive benzodiazepines rather than antidepressants and that 64 percent of benzodiazepine regimens deviate from HCFA guidelines on drug type and dose (34).
This study had several additional limitations. First, we wanted to minimize the burden on staff and include all residents regardless of their physical and mental status. Thus we had to rely on recorded diagnoses and nurses' assessments. Further studies are needed to validate these measures. Second, we were unable to survey physicians or examine previous treatment efforts. It would be interesting to know what types of treatments were attempted unsuccessfully before the study and before nursing home admission. Third, our sample was similar to other nursing home populations, but we cannot generalize to other states because of potential differences in state regulation, reimbursement, and other conditions that might affect drug use. Finally, we recognize that the relationships among depression, pain, sleep, demand, and benzodiazepine use are complex and subject to alternative explanations (35,36,37). Further studies are needed to provide an understanding of these risk factors, their interrelationships, and how they respond to different interventions (38,39).
Acknowledgments
This study was supported in part by grant R01-AG5120 from the National Institute on Aging and grant P50-MH43555 from the National Institute of Mental Health. The authors thank Roberta Braun Curtin, Ph.D., David McKee, Ph.D., Elizabeth Larson, M.S., and Matt Powers, B.Pharm.
Dr. Svarstad is William S. Apple distinguished professor of social pharmacy and professor of sociology and Dr. Mount is associate professor of social pharmacy at the School of Pharmacy, University of Wisconsin-Madison, 777 Highland Avenue, Madison, Wisconsin 53705 (e-mail, [email protected]).
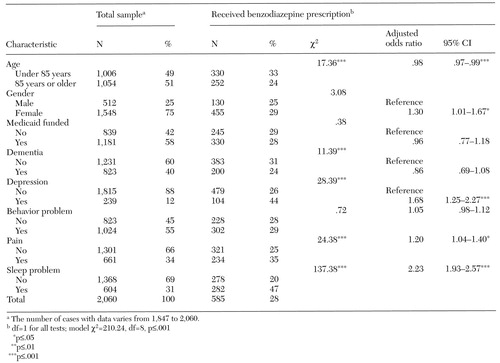 |
Table 1. Demographic and clinical characteristics and benzodiazepine prescriptions among 2,060 residents in 18 nursing homes in Wisconsin
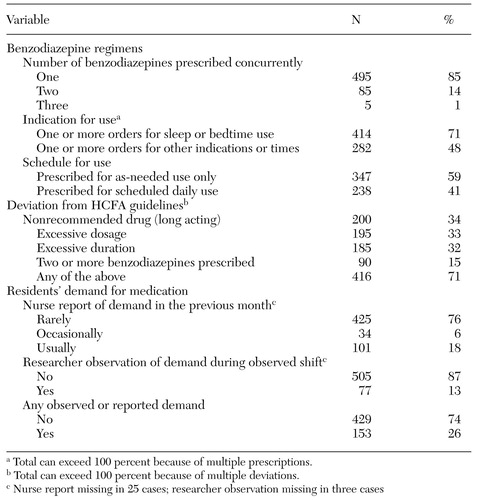 |
Table 2. Evaluation of benzodiazepine regimens and demand among 585 residents with benzodiazepine prescriptions in 18 nursing homes in Wisconsin
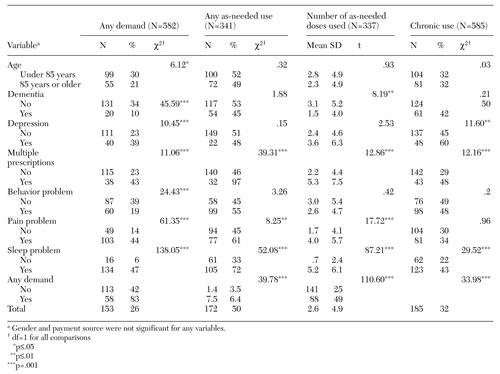 |
Table 3. Bivariate analysis of demand, as-needed use, and chronic use of benzodiazepines among residents 18 nursing homes in Wisconsin
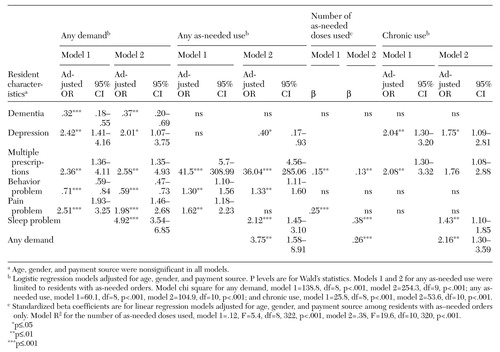 |
Table 4. Multivariate results of regression models predicting demand, as-needed use, and chronic use of benzodiazepines among residents in 18 nursing homes in Wisconsin
1. Griffiths R, Weerts E: Benzodiazepine self-administration in humans and laboratory animals: implications for problems of long-term use and abuse. Psychopharmacology 134:1-37, 1997Crossref, Medline, Google Scholar
2. Egan M, Moride Y, Wolfson C, et al: Long-term continuous use of benzodiazepines by older adults in Quebec: prevalence, incidence, and risk factors. Journal of the American Geriatrics Society 48:811-816, 2000Crossref, Medline, Google Scholar
3. Wang PS, Bohn RL, Glynn RJ, et al: Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. American Journal of Psychiatry 158:892-898, 2001Link, Google Scholar
4. Opedal K, Schjott J, Eide E: Use of hypnotics among patients in geriatric institutions. International Journal of Geriatric Psychiatry 13:846-851, 1998Crossref, Medline, Google Scholar
5. Svarstad BL, Mount JK: Chronic benzodiazepine use in nursing homes: effects of federal guidelines, resident mix, and nurse staffing. Journal of the American Geriatrics Society 49:1673-1678, 2001Crossref, Medline, Google Scholar
6. Heston LL, Garrard J, Makris L, et al: Inadequate treatment of depressed nursing home elderly. Journal of the American Geriatrics Society 40:1117-1122, 1992Crossref, Medline, Google Scholar
7. Leipzig R, Cumming R, Tinetti M: Drugs and falls in older people: a systematic review and meta-analysis: I. psychotropic drugs. Journal of the American Geriatrics Society 47:30-39, 1999Crossref, Medline, Google Scholar
8. Ray W, Thapa P, Gideon P: Benzodiazepines and the risk of falls in nursing home residents. Journal of the American Geriatrics Society 48:682-685, 2000Crossref, Medline, Google Scholar
9. Foy A, O'Connell D, Henry D, et al: Benzodiazepine use as a cause of cognitive impairment in elderly hospital inpatients. Journal of Gerontology: Medical Sciences 50A:M99-M106, 1995Google Scholar
10. Hanlon J, Horner R, Schmader K, et al: Benzodiazepine use and cognitive function among community-dwelling elderly. Clinical Pharmacology and Therapeutics 64:684-692, 1998Crossref, Medline, Google Scholar
11. Ried L, Johnson R, Gettman D: Benzodiazepine exposure and functional status in older people. Journal of the American Geriatrics Society 46:71-76, 1998Crossref, Medline, Google Scholar
12. Sarkisian C, Honghu L, Gutierres P, et al: Modifiable risk factors predict functional decline among older women: a prospectively validated clinical prediction tool. Journal of the American Geriatrics Society 48:170-178, 2000Crossref, Medline, Google Scholar
13. Svarstad BL, Mount JK, Bigelow W: Variations in treatment culture and nursing home response to drug regulations. Psychiatric Services 52:666-672, 2001Link, Google Scholar
14. Hughes M, Lapane K, Mor V, et al: The impact of legislation on psychotropic drug use in nursing homes: a cross-national perspective. Journal of the American Geriatrics Society 48:931-937, 2000Crossref, Medline, Google Scholar
15. Tobias D, Sey M: General and psychotherapeutic medication use in 328 nursing facilities: a year 2000 national survey. Consultant Pharmacist 16:54-64, 2001Google Scholar
16. Yee D, Tobias D: General and psychotherapeutic medication use in Canadian long-term care facilities. American Society of Consultant Pharmacists 15:1025-1031, 2000Google Scholar
17. Bassa R, Law J, Goldberg L: Hypnotics usage among elderly patients in homes and hospital wards in Salford. Pharmaceutical Journal 252:474-476, 1994Google Scholar
18. Buck J: Psychotropic drug practice in nursing homes. Journal of the American Geriatrics Society 36:409-418, 1988Crossref, Medline, Google Scholar
19. Castle N: Changes in resident and facility risk factors for psychotropic drug use in nursing homes since the Nursing Home Reform Act. Journal of Applied Gerontology 18:77-98, 1999Crossref, Google Scholar
20. Borson S, Doane K: The impact of OBRA-87 on psychotropic drug prescribing in skilled nursing facilities. Psychiatric Services 48:1289-1296, 1997Link, Google Scholar
21. Isacson D: Long-term benzodiazepine use: factors of importance and the development of individual use patterns over time: a 13-year follow-up in a Swedish Community. Social Science and Medicine 44:1871-1880, 1997Crossref, Medline, Google Scholar
22. Hardo P, Kennedy T: Night sedation and arthritic pain. Journal of Social Medicine 84:73-75, 1991Crossref, Medline, Google Scholar
23. Linden M, Bär T, Geiselmann B: Patient treatment insistence and medication craving in long-term low-dosage benzodiazepine prescriptions. Psychological Medicine 28:721-729, 1998Crossref, Medline, Google Scholar
24. Bayer A, Pathy M: Requests for hypnotic drugs and placebo response in elderly hospital in-patients. Postgraduate Medical Journal 61:317-320, 1985Crossref, Medline, Google Scholar
25. Mount JM: Nursing home responsiveness to research requests: results of a field study. Gerontologist 32:414-419, 1992Crossref, Medline, Google Scholar
26. Garrard J, Chen V, Dowd B: The impact of the 1987 federal regulations on the use of psychotropic drugs in Minnesota nursing homes. American Journal of Public Health 85:771-776, 1995Crossref, Medline, Google Scholar
27. Schmidt I, Claesson C, Westerholm B, et al: Resident and organizational factors affecting the quality of drug use in Swedish nursing homes. Social Science and Medicine 47:961-971, 1998Crossref, Medline, Google Scholar
28. Svarstad BL, Mount JK: Nursing home resources and tranquilizer use among the institutionalized elderly. Journal of the American Geriatrics Society 39:869-875, 1991Crossref, Medline, Google Scholar
29. Medicaid State Operations Manual: Provider Certification, Transmittal 250. Washington, DC, US Department of Health and Human Services, Health Care Finance Administration, April 1992Google Scholar
30. Manual of Psychiatric Peer Review, 3rd ed. Washington, DC, American Psychiatric Association, 1985Google Scholar
31. Rovner BW, Edelman GA, Cox MP, et al: The impact of antipsychotic drug regulations on psychotropic drug prescribing practices in nursing homes. American Journal of Psychiatry 149:1390-1392, 1992Link, Google Scholar
32. Kelly M, Swegle J, Clarke C, et al: Appropriateness of medication use in Iowa Medicaid recipients residing in long-term care facilities and receiving 15 or more medications. Consultant Pharmacist 15:1184-1191, 2000Google Scholar
33. Cramer GW, Chaponis RJ, Bauwens S, et al: Evaluation of sleep disorders in nursing facilities. Consultant Pharmacist 14:545-548,553-556, 1999Google Scholar
34. Zisselman M, Rovner B, Shmuely Y: Benzodiazepine use in the elderly prior to psychiatric hospitalization. Psychosomatics 37:38-42, 1996Crossref, Medline, Google Scholar
35. Ferrell BA, Ferrell BR, Osterweil D: Pain in the nursing home. Journal of the American Geriatrics Society 38:409-414, 1990Crossref, Medline, Google Scholar
36. Cramer GW, Galer BS, Mendelson MA, et al: A drug use evaluation of selected opioid and nonopioid analgesics in the nursing facility setting. Journal of the American Geriatrics Society 48:398-404, 2000Crossref, Medline, Google Scholar
37. Nicassio P, Wallston K: Longitudinal relationships among pain, sleep problems, and depression in rheumatoid arthritis. Journal of Abnormal Psychology 101:514-520, 1992Crossref, Medline, Google Scholar
38. Avorn J, Soumerai SB, Everitt DE, et al: A randomized trial of a program to reduce the use of psychoactive drugs in nursing homes. New England Journal of Medicine 327:168-173, 1992Crossref, Medline, Google Scholar
39. Gilbert A, Owen N, Innes J, et al: Trial of an intervention to reduce chronic benzodiazepine use among residents of aged-care accommodation. Australia and New Zealand Journal of Medicine 23:343-347, 1993Crossref, Google Scholar