Firearms Risk Management in Psychiatric Care
Abstract
OBJECTIVE: This study sought to assess the effectiveness of a firearms risk management program. METHODS: A firearms risk management program, which included multidisciplinary assessment, treatment, and discharge planning, was developed and implemented among 46 civilly committed psychiatric inpatients at the Twin Valley Psychiatric System, a behavioral health organization of the Ohio Department of Mental Health. RESULTS: The research sample comprised mainly men who had personality disorders and histories of substance abuse and who had expressed an intent to use a firearm to commit suicide. On discharge, none of the patients had access to a firearm. Of the 16 patients who were hospitalized during the next 24 months, only five were noted to have threatened to harm themselves or others with a firearm or to have access to a firearm. CONCLUSIONS: Multidisciplinary and focused assessment, treatment, and discharge planning can be effective in neutralizing the risk of firearms use among psychiatric patients.
Public support for greater regulation of firearms in the United States is widespread among people who own firearms and those who do not (1). Nevertheless, according to data from the National Crime Victimization Survey, about 1.2 million violent crimes were committed with a firearm in 1995 alone (2). In the same year, 69 percent of the nation's 22,552 homicides involved the use of a firearm (2,3).
The Centers for Disease Control and Prevention estimate that for every person who is shot to death in the United States, nearly three others are injured with firearms, suggesting that more than 400,000 individuals were injured by a firearm in 1995 (4). An additional 18,503 suicides in 1995 were committed with firearms (2).
The rates of injury and death due to firearms and the rate of crimes committed with firearms are far higher in the United States than in any other industrialized nation (5). Every hour, firearms are used to kill four people and to commit 120 crimes in the United States (5). In 1992 an estimated daily average of 36 people were murdered with a firearm, 32 women were raped at gunpoint, 931 people were held up at gunpoint, and an additional 1,557 people were assaulted with a firearm (6). In the same year, about 50 people a day used a firearm to kill themselves (6).
Forty percent of adults in the United States live in a household that has a firearm, and 25 percent own a firearm themselves (7). In addition, persons who purchase a handgun are 57 times more likely than the general population to commit suicide in the week after the purchase, and they continue to have a higher risk of suicide, even after six years (7,8).
The U.S. Department of Justice has reported that although the overall rate of violent crime has decreased in recent years, the rate of offenses committed with firearms has increased (6). In fact, the number of all violent crimes involving firearms as reported to the Federal Bureau of Investigation increased by 55 percent between 1987 and 1992 (6). In 1998, 65 percent of all murders and 40 percent of all robberies involved a firearm (3).
Mental illness and access to firearms
It has become increasingly evident from media coverage that persons who have untreated mental illnesses have easy access to firearms. There appears to be some understanding that persons with mental illness who commit assaults with firearms cannot be held wholly accountable for their actions, as evidenced in these cases. The problem is therefore most often viewed as societal rather than individual, in terms of both unimpeded access to deadly weapons and availability of treatment for which supply does not meet demand (1).
According to statistics compiled by the Treatment Advocacy Center in Arlington, Virginia, about 1,000 homicides a year are committed by people who have mental disorders (9), which accounts for about 5 percent of the nation's total number of homicides annually. Homicides committed by persons with mental illness are more likely to receive media scrutiny because of the vulnerable feelings they arouse in the general public, thus contributing substantially to the stigma associated with mental illness—perhaps, paradoxically, discouraging persons who have mental illnesses from seeking treatment.
Possibly as a result of the media scrutiny received and the vulnerable feelings aroused by these cases, advocacy groups in many states are seeking mandatory medication laws. The premise underlying the push for involuntary treatment is that specific symptoms of untreated mental illness—for example, paranoid delusions and auditory hallucinations—can lead to violent behavior. It is believed that if these psychiatric symptoms are controlled or eliminated, the risk of violence will also be reduced or eliminated. Although this may be a valid premise, it does not address ownership of firearms. As we have noted, among firearms purchasers who have no known history of mental illness, possession of a firearm substantially increases the risk of death by suicide (8). Epidemiologic studies have shown that persons who have certain psychiatric disorders also have a greater risk of suicide (10,11,12). It stands to reason that access to firearms might further increase that risk.
Given that firearms remain relatively easy to acquire and that individuals who have severe mental illnesses are at risk of hurting themselves or others with firearms, the mental health community should place greater emphasis on managing firearms risk in psychiatric populations. However, currently nothing in the psychiatric or psychological literature addresses specific interventions aimed at the risks associated with access to firearms. Accordingly, the Twin Valley Psychiatric System in Columbus, Ohio, developed and implemented a multidisciplinary risk management program specifically designed to address access to firearms in psychiatric populations.
Methods
Sample
The research sample comprised 46 civilly committed psychiatric inpatients—38 men and eight women. During the admission process, these patients were identified as having threatened to harm themselves or others with a firearm or as having access to a firearm. They were selected from a total of 664 admissions to the Twin Valley Psychiatric System in 1999. The research sample was also classified along seven other descriptive variables: DSM-IV diagnoses, psychiatric hospitalizations, type of weapon possessed, intended victim, living situation, relationship instability, and life failures.
Procedure
Assessment. All patients were assessed by a psychiatrist on admission. Psychiatrists used a checklist of risk factors to record each patient's psychiatric symptoms and DSM-IV diagnoses as well as specific information on history of violence, crime, and psychosocial stressors as indicated by information obtained from a mental status examination, behavioral observations by staff, and collateral resources.
This information was then passed on to a multidisciplinary treatment team, who reviewed the information within 24 hours of the patient's admission. The multidisciplinary team— typically composed of the patient's attending psychiatrist, a registered nurse, a psychologist, a social worker, the patient's case manager, various ancillary therapists, and the patient—determined the patient's risk-related needs and gathered more detailed information about the patient's history of threatening to harm him- or herself or others with a firearm and the patient's access to firearms.
For patients who were identified as having threatened to harm themselves or others with a firearm or as having access to a firearm, the multidisciplinary treatment team implemented a treatment plan that included measures to immediately address the risk posed to the patient or to others—for example, notifying family members of threats or referring the patient to a firearms treatment group. During the next 72 hours, a more comprehensive treatment plan was implemented, which addressed issues beyond the risk of harm posed by the patient—for example, substance abuse and lack of housing.
Throughout treatment, patients who were identified as having threatened themselves or others with a firearm or as having access to a firearm were further assessed by an assigned social worker. The social worker completed a firearms flow sheet, which documented the type and location of the firearm and any identified victim and that victim's awareness of the threat. The social worker then contacted the patient's family, the patient's case manager, and law enforcement officials, as necessary, to verify the patient's access to a firearm and any firearm-related threats.
If family members minimized the issue of the patient's access to a firearm or threats to use a firearm, the social worker explained the potential associated risks. In addition, the social worker strongly encouraged the families of patients who had access to a firearm to restrict that access—for example, to remove the firearm from the home. Information gathered from collateral sources and the steps taken by the social worker to neutralize the risk of the patient's using the firearm were then documented on the firearms flow sheet.
Monitoring. Each patient's treatment plan was subjected to a quality assurance process to determine whether all the identified risk-related needs were being adequately addressed. Risk-related needs that were identified as not being adequately addressed were referred back to the multidisciplinary treatment team. A follow-up review occurred within 48 hours to ensure that the indicated corrections or additions had been made.
Treatment. A therapy group on self-control skills for interpersonal stressors was specifically designed for patients who were identified as having threatened to harm themselves or others with a firearm or as having access to a firearm. Staff members from the psychology and social work departments facilitated this group. In the therapy group, patients learned to identify how they had relied on external physical means—firearms in particular—to deal with their psychiatric, psychological, and emotional problems.
Members of the group specifically learned to distinguish between internal and external coping skills and then to identify and begin using alternative and socially appropriate methods to gain control. They learned not to rely on or to use firearms or other weapons. The facilitator taught basic cognitive-behavioral concepts, including understanding the relationship between thoughts, feelings, physiology, and behavior and the relationship between antecedents, behaviors, and consequences. The patients were trained in behavioral time-outs, relaxation techniques, and stress management exercises. Treatment goals focused on effective and assertive communication, problem solving, and conflict resolution without the use of force or threats.
Consultation. Consultation was available to address diagnostic issues or interventions at any point during a patient's assessment or treatment. Consultations were requested by the patient's multidisciplinary treatment team and included professionals such as forensic psychiatrists, psychopharmacologic experts, and the medical services director.
Discharge. After a patient had been stabilized, the priority of treatment was to discharge the patient to the least restrictive, safest environment available, while maintaining neutralization of the risk of firearms use. To this end, the treatment team developed a detailed relapse prevention plan for identifying symptomatic and behavioral cues related to risk and for activating outpatient assessment on the emergence of any of the identified cues. Twenty-four hours before discharge, the patient's social worker forwarded the firearms flow sheet to the social work supervisor, who reviewed the flow sheet and the medical record to determine whether there were any outstanding risk issues and, if so, how these issues should be addressed. The discharge plan and related information were then forwarded to the community discharge agency.
After the patient's discharge, the community discharge agency was responsible for continually monitoring whether the patient had regained access to a firearm. If the patient had regained access, appropriate actions could have included—but would not necessarily have been limited to—protecting the patient from self-harm and notifying potential victims of the possible danger.
Results
The demographic data, DSM-IV diagnoses, and data on psychiatric hospitalizations for the research sample and the larger sample of 664 admissions from which the research sample was drawn are compared in Table 1. Data on the five other descriptive variables for the research sample are shown in Table 2. These data are generally consistent with the results of other studies that have shown that persons who use firearms are likely to use them for suicide, to be male, to abuse alcohol, and to have an antisocial or borderline personality disorder (8,13,14,15,16). The average age of patients in the admission sample was 31 years (range, 17 to 67 years), and the average age of patients in the research sample was 33 years (range, 19 to 60 years).
As Table 3 shows, by the time of discharge the treatment team had successfully neutralized the risk associated with all the firearms that had been accessible to patients in the research sample on admission. Thirty-two (70 percent) of the 46 patients had never had access to a firearm—that is, their claims about intending to use a firearm had been threats only. Of the patients who did have access to a firearm, eight (17 percent) relinquished control of the firearm to a family member or a significant other, four (9 percent) turned their firearms over to law enforcement officials, and two (4 percent) permitted their case manager to take responsibility for the firearms. Thus, of the 46 patients who had threatened to use a firearm on admission, none had access to a firearm on discharge.
Preliminary follow-up analyses of our research sample are also shown in Table 3. Of the 46 patients, 16 (35 percent) were readmitted to the hospital within 24 months. Of these 16 patients, five had threatened themselves or others with a firearm or had regained access to a firearm. Thus neutralization of the risk of firearms use had remained relatively effective for 89 percent of the research sample.
Discussion
Firearms are relatively accessible in the United States (1,7), and their dangerousness is evident in the number of suicides, murders, assaults, and other crimes that are committed with them (2,3). Persons who are mentally ill, in particular, are at high risk of using a firearm to hurt themselves or others (8). However, few studies have addressed the management of firearms risk and specific interventions to neutralize the accessibility of firearms to persons who have mental illness.
To address this dearth in the literature, the Twin Valley Psychiatric System developed and implemented a firearms risk management program consisting of multidisciplinary assessment, treatment, and discharge planning. The research sample comprised mainly men with personality disorders and a history of substance abuse who had expressed an intent to use a firearm to commit suicide. These characteristics were consistent with those found in previous studies of firearms and suicide (8,13,14,15,16). Other data were collected as well, including demographic, psychiatric, and psychosocial characteristics, such as marital status, psychiatric hospitalizations, and living situation. In conjunction with future research, this information will assist in more accurately identifying the risk factors associated with the use of firearms in psychiatric populations.
Sixteen of the 46 patients in the research sample were identified as having threatened to harm themselves or others with a deadly weapon other than a firearm—for example, a knife. This finding suggests that persons who own or have access to a firearm may also have access to another type of deadly weapon. Future research and treatment programs should take this possibility into account.
Through the assessment process, we determined that a majority of the patients in the research sample (70 percent) did not in fact have immediate access to a firearm. However, a relationship clearly exists between threatening to commit suicide or homicide and eventually committing the act (15,17). Thus it was imperative that all the patients undergo treatment.
The objective of neutralizing access to firearms was met—none of the patients in the research sample had access to a firearm when they were discharged. Neutralization persisted for most of the patients—of the 46 patients in the research sample, 16 were rehospitalized, and only five of them were noted at that time to have threatened to harm themselves or others with a firearm or to have had access to a firearm. However, we did not assess the legitimacy of the claims of these rehospitalized patients; it is possible that some or all of these patients did not in fact have access to a firearm when they were readmitted.
Future programs for managing the risk of firearms use should more heavily emphasize consistent follow-up with the community discharge agency that is responsible for monitoring the patient identified as being at risk. Likewise, outpatient monitoring should be enhanced to maximize the likelihood of sustained neutralization of access to firearms, which could be facilitated through greater involvement of frontline staff—for example, case managers—with at-risk patients in the community.
Conclusions
We developed and implemented a firearms risk management program, which included multidisciplinary assessment, treatment, and discharge planning. None of the 46 patients who had access to or had threatened to use a firearm still had access to a firearm at discharge, and only five were noted to have threatened to use a firearm or to have had access to a firearm on rehospitalization. Thus access to firearms can be successfully neutralized, even in high-risk populations, through the implementation of focused multidisciplinary assessment, treatment, and discharge planning.
The authors are affiliated with the Twin Valley Psychiatric System, 2200 West Broad Street, Columbus, Ohio 43223 (e-mail, [email protected]).
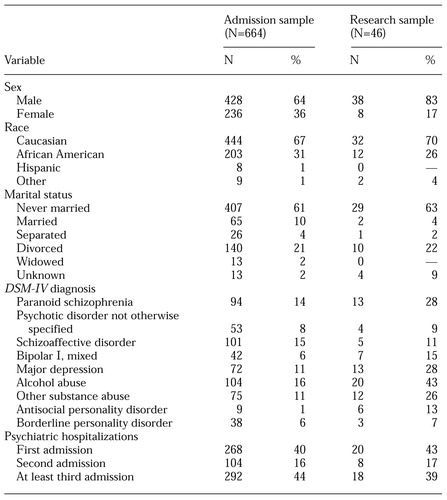 |
Table 1. Demographic data and clinical characteristics of 664 admissions to a psychiatric facility and a research sample of 46 patients who threatened to harm themselves or others with a firearm or who claimed to have access to a firearm at admission
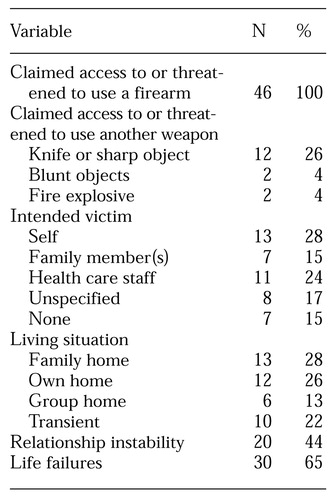 |
Table 2. Characteristics of 46 patients in a psychiatric facility who threatened to harm themselves or others with a firearm or who claimed to have access to a firearm at admission
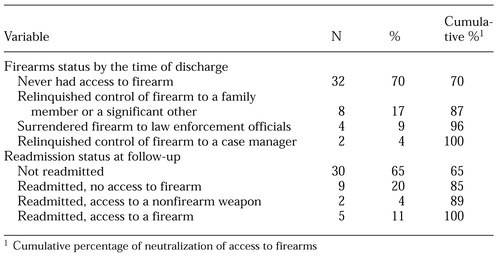 |
Table 3. Firearms status by the time of discharge and readmission status at 24-month followup among 46 patients in a psychiatric facility who threatened to harm themselves or others with a firearm or who claimed to have access to a firearm at admission
1. Teret SP, Webster DW, Vernick JS, et al: Support for new policies to regulate firearms. New England Journal of Medicine 339:813-818, 1998Crossref, Medline, Google Scholar
2. Federal Bureau of Investigation: Uniform Crime Reports for the United States. Washington, DC, US Department of Justice, 1995Google Scholar
3. Federal Bureau of Investigation: Uniform Crime Reports for the United States. Washington, DC, US Department of Justice, 1998Google Scholar
4. Centers for Disease Control and Prevention Web site. Available at http://www.cdc.gov/ncipc/factsheets/fafacts.htmGoogle Scholar
5. Hemenway D: Regulation of firearms. New England Journal of Medicine 339:843-845, 1998Crossref, Medline, Google Scholar
6. Federal Bureau of Investigation: Uniform Crime Reports for the United States. Washington, DC, US Department of Justice, 1992Google Scholar
7. Wintemute GJ, Drake CM, Beaumont JJ, et al: Prior misdemeanor conviction as a risk factor for later violent and firearm-related criminal activity among authorized purchasers of handguns. JAMA 280:2083-2087, 1998Crossref, Medline, Google Scholar
8. Wintemute GJ, Parham CA, Beaumont JJ, et al: Mortality among recent purchasers of handguns. New England Journal of Medicine 341:1583-1589, 1999Crossref, Medline, Google Scholar
9. Treatment Advocacy Center Web site. Available at http://www.psychlaws.org/general resources/fact1.htmGoogle Scholar
10. Kessel N, Grossman G: Suicide in alcoholics. British Medical Journal 2:1671-1672, 1961Crossref, Medline, Google Scholar
11. Linehan MM, Shearin EN: Lethal stress: a social-behavioral model of suicidal behavior, in Handbook of Life Stress, Cognition, and Health. Edited by Fisher S, Reason J. New York, Wiley, 1988Google Scholar
12. Roy A: Suicide in chronic schizophrenics. British Journal of Psychiatry 141:171-177, 1982Crossref, Medline, Google Scholar
13. De Moore GM, Robertson AR: Suicide attempts by firearms and by leaping from heights: a comparative study of survivors. American Journal of Psychiatry 156:1425-1431, 1999Abstract, Google Scholar
14. Frierson RL, Lippmann SB: Psychiatric consultation for patients with self-inflicted gunshot wounds. Psychosomatics 31:67-74, 1990Crossref, Medline, Google Scholar
15. Peterson LG, Peterson M, O'Shanick GJ, et al: Self-inflicted gunshot wounds: lethality of method versus intent. American Journal of Psychiatry 142:228-231, 1985Link, Google Scholar
16. Selway R: Gunshot suicides in Victoria, Australia, 1988. Medicine, Science, and the Law 31:76-80, 1991Crossref, Medline, Google Scholar
17. Asnis GM, Kaplan ML, Hundorfean G, et al: Violence and homicidal behaviors in psychiatric disorders. Psychiatric Clinics of North America 20:405-425, 1997Crossref, Medline, Google Scholar



