Adherence to Antipsychotics Among Latinos and Asians With Schizophrenia and Limited English Proficiency
Antipsychotic medications are the foundation of treatment for people with schizophrenia. Despite the demonstrated ability of antipsychotic medications to reduce symptoms and relapse rates and improve health outcomes, nonadherence to them is common, with average rates of 40% to 50% ( 1 , 2 , 3 , 4 , 5 , 6 , 7 ). Poor adherence is associated with increased relapse, psychiatric hospitalizations, emergency room visits, and hospitalization costs ( 3 , 6 , 8 , 9 , 10 , 11 , 12 ). Nonadherence is also associated with poor social outcomes, including greater risk of arrest, violence, victimization, and substance use and poorer mental functioning and life satisfaction ( 9 ).
Numerous factors can influence adherence to a prescribed treatment plan. Osterberg and Blaschke's review ( 13 ) of general medication adherence identified numerous factors that may influence adherence, including patient-level factors (such as forgetfulness, other priorities, intentional omission of doses, and emotional factors) and provider-level factors (such as prescription of a complex medication regimen, failure to explain side effects and benefits associated with the medication, disregard for a patient's lifestyle or economic resources, and poor patient-provider relationships). Lacro and colleagues ( 14 ) identified additional patient- and provider-level factors predictive of nonadherence to antipsychotic medication among persons with schizophrenia, including poor insight, negative attitude or negative subjective response toward medication, substance abuse, shorter illness duration, and inadequate discharge planning or aftercare environment ( 14 ). A patient's knowledge about the benefits of a medication and its side effects, frequency, duration, and dosing may be affected by providers' explanations about new medications ( 15 ), which a patient with limited language proficiency may misunderstand. Similarly, a client's level of health literacy may affect the processing of information provided during clinical visits ( 16 ).
Few studies have examined the relationship between adherence to antipsychotic medications among adults from ethnic minority groups who have a diagnosis of schizophrenia ( 6 , 17 , 18 ). Diaz and colleagues ( 17 ) conducted a community-based study using an electronic monitoring system of bottle openings to assess psychotropic medication utilization behaviors among 19 African Americans, 44 monolingual and 25 bilingual Latinos, and 34 Caucasians. They found that African Americans and monolingual Spanish-speaking clients were less likely than Caucasians to be adherent. Another study, which used Texas Medicaid data, found that African-American and Mexican-American clients were less adherent than non-Latino whites ( 18 ). A third study, in San Diego County, found that Latinos and African Americans were significantly less likely to be adherent than non-Latino whites ( 6 ).
With the exception of the work by Diaz and colleagues ( 17 ), we are aware of no other study that has examined adherence to antipsychotics by language status. This study provides a unique contribution by examining the relationship of race-ethnicity and language status to adherence to antipsychotic medications among Latino and Asian clients with schizophrenia in a large public mental health system. San Diego County is a large, ethnically diverse county located on the United States-Mexico border. It is home to large ethnic minority and foreign-born populations, particularly Latinos of Mexican origin and Asians, most of whom are Filipino and Vietnamese. In 2007 San Diego County had a total population of approximately 3.1 million; 29% were Latino, 9% were Asian, and 5% were African American ( 19 ).
Expanding on prior research, the objectives of this study were to analyze the relationship between race-ethnicity, English proficiency, and adherence to antipsychotic medications among persons with a diagnosis of schizophrenia and to analyze the relationships between race-ethnicity, English proficiency, adherence, psychiatric and nonpsychiatric hospitalization, and costs.
Methods
A conceptual model of language, adherence, and service use
We propose an expanded model of adherence that considers the roles of language and family support in predicting adherence to antipsychotic medication and use of mental health services. The studies reviewed above found that patient and provider factors interact to affect adherence and that language proficiency affects the exchange of information between patient and provider. However, a client's level of English proficiency may also be a proxy for migration history, culture, and family and social support. Ramirez Garcia and colleagues ( 20 ) found that familial support predicted better medication adherence among Mexican Americans with schizophrenia. Although a client with low English proficiency may experience difficulty in communicating with his or her provider, the client may also benefit from engagement of family members in the treatment process. Thus a client's low English proficiency may result in increased participation in care by family members. Barriers to communication and adherence may be reduced if family members can effectively serve as linguistic and social translators between the patient and provider ( 21 ).
Adherence to antipsychotic medications is associated with fewer inpatient admissions ( 3 , 6 , 8 , 9 , 10 , 11 , 12 ). We propose an additional link between English proficiency and service use ( 22 , 23 ). That is, we expect that the set of cultural and social factors associated with English proficiency has an independent effect on hospitalizations and costs beyond their effects on medication adherence.
Sample and independent variables
Data from San Diego County Adult and Older Adult Mental Health Services (AOAMHS) encounter-based management information system (MIS) were merged with data from California's Department of Health Care Services to identify Medi-Cal (California's Medicaid program) beneficiaries with schizophrenia who were living in the community and receiving psychiatric services and who filled prescriptions for oral antipsychotic medications during 1999–2004 (N=31,560 person-years). The MIS includes demographic information—age, gender, self-reported race or ethnicity, and self-reported preferred language for mental health services.
As in previous research, we used a client's preferred service language as a proxy for limited English proficiency status ( 22 , 23 ). Clients report their preferred language for receiving services at admission to each service. In California, language is highly correlated with foreign-born status. We analyzed data from the California Health Interview Survey and found that among Latino adults in San Diego in homes where Spanish is spoken, 73% were born in Mexico, and among Asians in homes where Chinese or Vietnamese is spoken, 86% were born in Asia or the Pacific Islands ( 24 ). The sample for the study reported here is limited to Latinos with a preferred language of Spanish or English, Asians with a preferred Asian language (for example, Vietnamese and Tagalog) or English, and non-Latino whites (hereafter, whites) with a preferred language of English. Among the 460 Asian clients in the sample, 44% (N=201) were Filipino, 17% (N=78) were Vietnamese, 8% (N=36) were Japanese, 7% (N=32) were Chinese, and 25% (N=113) were from other Asian groups.
Clients also report their living situation at admission to each service. We classified clients by their most commonly reported living situation. We included persons living independently, residents in assisted living facilities (also known as board-and-care facilities), homeless adults, and adults with unknown living situations. We excluded persons residing primarily in jails or long-term institutional care facilities. We also excluded persons with no insurance, because data on medication use, payment, and health services costs were unavailable. Conservatorship status was ascertained from the MIS, and Medicare eligibility was identified from the Medi-Cal data. Diagnosis of a substance use disorder was identified across both systems. Medi-Cal has strict requirements to verify residency status. Thus clients included in this study are either U.S. citizens or documented immigrants.
We used ICD-9 diagnosis codes from the Medi-Cal claims to assess comorbid illness severity with the Chronic Illness and Disability Payment System (CDPS) ( 25 ). CDPS is a diagnostic classification system that is commonly used by Medicaid programs to assess illness severity and make health-based capitated payments to health plans that enroll Medicaid beneficiaries. The CDPS software assigns diagnostic codes obtained from claims to 56 diagnostic categories within 18 major diagnostic groups corresponding to major body systems (for example, cardiovascular) or type of disease (for example, diabetes). CDPS scores then are assigned on the basis of age, gender, and presence of diagnostic categories. These scores reflect illness severity on the basis of predicted future expenditures; a score permits comparison to the average expenditure across all Medicaid beneficiaries. For example, a 40-year-old male with schizophrenia but no general medical comorbidity would have a risk score of 1.2, and therefore would be expected to have 20% greater Medicaid costs than an average beneficiary. (Additional information on CDPS and public use software is available at cdps.ucsd.edu ).
Dependent variables
Adherence to prescribed regimens was determined by examining Medi-Cal claims by means of medication refill records. Adherence was measured by the annual medication possession ratio (MPR), which was computed for each person in each calendar year. The MPR was calculated by dividing the number of days that medications were available for consumption by the number of days that adults were eligible for Medi-Cal. For example, a person eligible for Medi-Cal for the entire year but who received a total of 240 days' supply of prescribed antipsychotic medication would have an MPR of .66. Quetiapine is commonly used as a sleeping aid; thus, we excluded it when prescribed at a low daily dosage (200 mg or less) in conjunction with another antipsychotic. We also excluded individuals who were prescribed depot antipsychotics, because the pharmacokinetic profiles of depot antipsychotic medications and oral medications vary considerably and because users of depot medications are typically more nonadherent to medication regimens and are frequent users of inpatient services. We categorized adherence during a person-year on an ordinal scale derived from the MPR using the following designations: nonadherent (MPR<.49), partially adherent (MPR=.50–.79), adherent (MPR=.80–1.10), and fillers of excess medication (MPR<1.10). Reasons for excess filling of medications include overuse, loss, or theft of medications.
We used Medi-Cal claims to determine whether someone was hospitalized in a given year in an acute psychiatric facility, a psychiatric ward of a community hospital, or a medical-surgical ward of an acute care hospital. We calculated the total amount paid by Medi-Cal for health services (inpatient and outpatient psychiatric and general medical care, laboratory and radiological services, and other noninpatient acute care), the amount paid for all pharmaceuticals, and the total amount paid for acute care. Costs are reported in 2004 dollars.
This merged MIS-Medi-Cal database has been previously used to examine utilization of mental health services by language status and costs associated with nonadherence to antipsychotic medications ( 6 , 23 ). The University of California, San Diego, Institutional Review Board and the San Diego County Mental Health Services Research Committee approved the use of these data for this study in accordance with the privacy rule of the Health Insurance Portability and Accountability Act of 1996.
Statistical analyses
We used multinomial logistic regression to estimate the probability of being nonadherent, partially adherent, adherent, or an excess filler as a function of race-ethnicity and preferred language while controlling for age, gender, conservatorship status, Medicare coverage, living situation, type of antipsychotic medication, CDPS score, and diagnosis of a comorbid substance use disorder. The resulting parameter estimates were used to calculate estimates of adherence by race-ethnicity and language status standardized to the underlying population characteristics. For example, we calculated the probability of being adherent among Latinos with limited English proficiency as the mean probability of being adherent across all persons as if all had limited English proficiency. Standard errors were estimated by using the nonparametric bootstrap method with 1,000 replications; p values were computed from the estimated distributions ( 26 ). To account for potential individual-correlated errors, data for the bootstrap analysis were sampled by the individual, rather than by observation.
We used logistic regression to estimate the probability of psychiatric admission, nonpsychiatric admission, and any inpatient admission and to calculate standardized estimates by adherence category and race-ethnicity language status using the methods described above and similarly controlling for the additional demographic and clinical characteristics. Finally, we used generalized linear regression, assuming a gamma distribution and a log link function, to estimate health services costs, pharmaceutical costs, and total costs and to provide standardized estimates of costs by race-ethnicity and language status using the methods described above ( 27 , 28 ).
Results
Table 1 provides information by English proficiency status on selected characteristics of adults treated for schizophrenia with antipsychotic medications. The data include 7,784 unique Medi-Cal beneficiaries, including 5,695 non-Latino whites, 1,196 English-proficient Latinos, 523 Latinos with limited English proficiency, 298 English-proficient Asians, and 162 Asians with limited English proficiency. Latinos and Asians with limited proficiency were older than English-proficient Latinos and Asians and roughly the same age as whites. Latinos with limited proficiency were more likely than English-proficient Latinos to be female (52% compared with 42%). Asian clients with limited proficiency were less likely than English-proficient Asians to have dual Medicare-Medi-Cal coverage (24% and 31%).
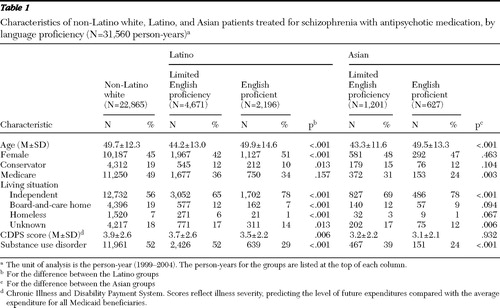 |
Across language and racial-ethnic groups, the majority of adults (>50%) treated for schizophrenia resided independently. Notably, more than three-quarters of Latinos and Asians with limited English proficiency resided independently (78% of each); these proportions are higher than those of English-proficient Latinos or Asians (65% and 69%, respectively). The mean CDPS score exceeded 3 for each group, indicating that this sample is expected to have health care costs at least three times as high as an average Medicaid beneficiary. Fewer adults with limited proficiency had comorbid substance use disorders compared with English-proficient adults. For example, 52% of English-proficient Latinos had a substance use disorder diagnosis compared with 29% of Latinos with limited proficiency; among Asians, differences by language status were less pronounced but nevertheless significant (39% and 24%, respectively).
Probability of hospitalization by level of adherence is shown in Table 2 . Clients who were adherent to their medications were least likely to experience a psychiatric admission (15%), a nonpsychiatric admission (18%), and any admission (28%). Overall, nearly half (48%) of nonadherent adults were hospitalized. These results support the validity of the MPR as a measure of adherence.
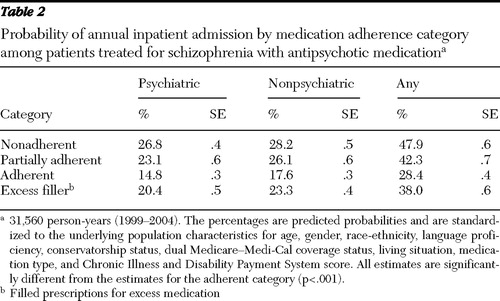 |
Adherence to antipsychotic medications by race-ethnicity and English proficiency is shown in Table 3 . Notably, a greater proportion of Latinos with limited proficiency were adherent compared with English-proficient Latinos (41% and 36%; p=.002). In contrast, a smaller proportion of Asians with limited proficiency were adherent compared with their English-proficient counterparts (40% and 45%; p=.034). Both Latino and Asian adults with limited proficiency were less likely than their English-proficient peers to be excess fillers of antipsychotic medication. For example, 15% of Latinos with limited proficiency met criteria for excess medication filling compared with 20% of English-proficient Latinos (p<.001). Similarly, 13% of Asians with limited proficiency were excess fillers compared with 17% of English-proficient Asians (p=.002). Notably, for Latinos the higher rate of adherence among those with limited proficiency was entirely attributable to their being less likely to be excess fillers. Non-Latino whites were most likely to be excess fillers (22%).
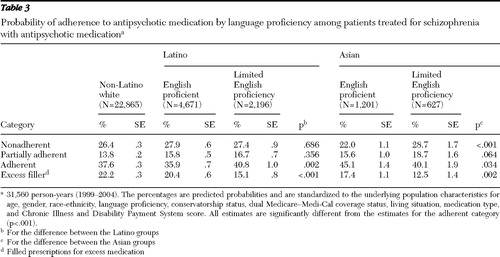 |
Several of the controlling variables were also related to adherence. For the overall sample, the probability of being adherent increased with age, from 25% among those aged 24 or younger to 37% among those aged 25 to 59 and 43% among those aged 60 and older. Clients who resided in assisted living facilities were highly likely to be adherent (47%) or excess fillers (34%), and clients who were homeless were highly likely to be nonadherent (49%). Clients with a diagnosis of a substance use disorder were less likely to be adherent than those without such a diagnosis (32% and 44%).
The probability of inpatient hospitalization by race-ethnicity and language status is shown in Table 4 (the analysis controlled for level of adherence). Latinos with limited proficiency were less likely than English-proficient Latinos to experience psychiatric admissions (17% and 21%; p<.001) and nonpsychiatric admissions (20% and 22%; p=.014); the rate of overall inpatient admissions was also lower (33% and 38%; p<.001). Overall admissions were lower among Asians with limited proficiency compared with English-proficient Asians, although this effect did not reach significance (33% and 38%; p=.070).
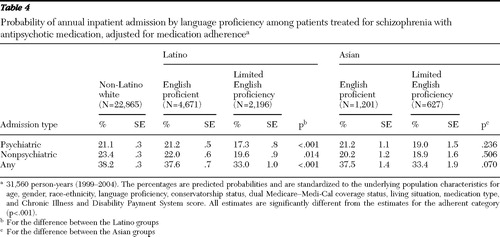 |
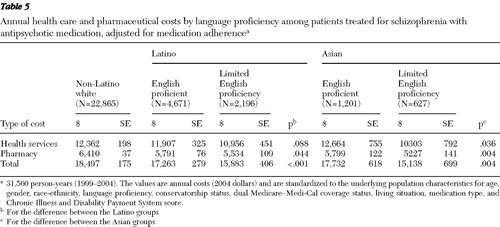
Costs of health services and pharmacy costs by race-ethnicity and language status are shown in Table 5 (the analysis controlled for level of adherence). Latinos and Asians with limited proficiency had the lowest overall costs ($15,883 and $15,138, respectively) compared with other groups, an outcome that resulted from lower health services and pharmacy costs among adults with limited proficiency compared with their English-proficient counterparts.
 |
Discussion
Although several studies have examined adherence to psychiatric medications, only a few have addressed the relationship between antipsychotic adherence and race-ethnicity, and we know of only one small study that examined adherence among monolingual and bilingual Spanish-speaking Latino clients ( 17 ). No study that we know of has examined adherence among Asian clients in the United States by language status. The study presented here addressed these gaps by examining the experiences of a large public mental health system providing care to an ethnically and linguistically diverse community. Given the nation's growing immigrant population ( 29 ), it is critical to understand the factors that influence the mental health outcomes of ethnically and linguistically diverse adults with serious mental illness.
This study found that Latinos with limited English proficiency were more likely than English-proficient Latinos to be adherent to antipsychotic medications. The difference in adherence among these two Latino groups was entirely attributable to differences in excess filling of prescriptions. Excess filling is also an indicator of poor medication management. In this study, individuals who were excess fillers were more likely than those who were adherent to be hospitalized, and excess fillers have been shown to have higher costs resulting from higher rates of hospitalizations and to increased pharmaceutical costs ( 6 ). After the analyses controlled for adherence and comorbidity, Latinos with limited English proficiency were less likely to be hospitalized and had lower pharmaceutical and total costs. In contrast, Asians with limited proficiency were less likely than English-proficient Asians to be adherent, although they were also less likely to be hospitalized and had lower costs.
One explanation for the higher rate of adherence and lower rate of hospitalization among Latinos with limited English proficiency is that they may benefit from a higher level of familial and social support. Cultural variation within and between groups may lead to differential adherence outcomes associated with race-ethnicity and English proficiency. Family social support may serve as a cultural buffer, and family involvement in the client's life and treatment plan may improve medication adherence and independently affect service utilization. Barrio and colleagues ( 21 ) found that the monolingual Spanish-speaking Latino clients were often accompanied during medical visits by English-speaking relatives (for example, adult children, spouses, or siblings), who advocated on their behalf with providers. Ramirez Garcia and colleagues ( 20 ) found that family instrumental (task-oriented) support predicted higher medication adherence among Mexican Americans with schizophrenia who were living with family members. In contrast, Kopelowicz and colleagues ( 30 ) did not find improved medication adherence among Latino clients who received skills training.
However, the hypothesis about greater family support is inconsistent with our finding of lower adherence and a lower probability of hospitalization among Asians with limited English proficiency. It may be that familial and social support operates differently among Asians. Perceived susceptibility to disease, perceived benefits of Western medication, perceived benefits of cultural or traditional medication, or stigma associated with psychiatric medication may serve to reduce adherence among Asians with limited English proficiency ( 31 , 32 ). Culturally appropriate medication management services may prove effective in improving adherence among Asian clients.
Unfortunately, we were unable to test explicitly for the independent effects of language proficiency and social support. The language status measure is potentially correlated with several aspects of clients' life experiences, including heritage, culture, acculturation, physiology, genetics, and preferences. Future data collection efforts may address these limitations by including specific measures that will permit us to more fully explore the mechanisms that drive these differences in adherence and service utilization.
Our results are limited by the use of administrative data, which lack some of the dimensions needed to fully study issues related to antipsychotic medication adherence among racial-ethnic minority populations. At the same time, our large sample size may have resulted in findings that are statistically significant but clinically insignificant. We used medication refill records from claims data to assess adherence. Although this approach is limited in its inability to directly monitor medication administration, claims data represent an objective and unobtrusive measure of adherence. We lacked clients' self-reported English proficiency status, and we did not have data on the language that was most commonly spoken at home. Both of these measures have been employed in other research examining the impacts of language on health service use ( 33 ). Patients' use of alternative treatments was unknown in this study. Use of alternative practitioners by Asian patients is common and may have resulted in lower rates of adherence or service use ( 34 , 35 ). Because of sample size limitations, Asians were classified as a single group despite the wide heterogeneity of cultural backgrounds, language, and family dynamics. For these reasons, our findings should be replicated with a larger sample that can disaggregate data by Asian subgroup. Future investigations may examine the role of various levels of social support provided by families (for example, instrumental support compared with emotional support) in medication adherence and service utilization across Asian subgroups. Finally, the high rate of excess prescription filling among residents of assisted living facilities warrants further investigation. Medication therapy management, which is a pharmacist-led review of clients' pharmacotherapy that includes consideration of therapeutic goals, interactions, side effects, and adherence, would provide a deeper understanding of the causes of excess filling in this setting and may provide a vehicle for intervention if excess filling is inconsistent with clients' treatment goals.
Conclusions
We found that adherence to antipsychotic medication among Latinos and Asians with schizophrenia varied by English language proficiency. A systematic examination of clinical outcomes by language status is needed in order to assess whether health disparities may be emerging among certain patient subgroups. Health care organizations should continue to prioritize the use of professional translation services for patients with limited English proficiency, rather than relying on family or friends, in order to ensure both patients' confidentiality and the accurate conveyance of health information ( 36 ). It is also critical that medical schools and allied health professional programs, such as nursing and physician assistant programs, continue to promote an ethnically diverse and linguistically adept health care workforce ( 37 ), so that patients and providers may communicate with each other in a timely manner and without intermediaries.
Acknowledgments and disclosures
Financial support was provided by grant P30-MH066248 from the National Institute of Mental Health and grant 3R01-DA019829-S2 from the National Institute on Drug Abuse. The authors gratefully acknowledge the County of San Diego Health and Human Services Agency Adult and Older Adult Mental Health Services for access to the management information system.
The authors report no competing interests.
1. Fenton WS, Blyler CR, Heinssen RK: Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophrenia Bulletin 23:637–651, 1997Google Scholar
2. Svarstad BL, Shireman TI, Sweeney JK: Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatric Services 52:805–811, 2001Google Scholar
3. Valenstein M, Copeland LA, Blow FC, et al: Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Medical Care 40:630–639, 2002Google Scholar
4. Lacro JP, Dunn LB, Dolder CR, et al: Prevalence of and risk factors for medication nonadherence inpatients with schizophrenia: a comprehensive review of recent literature. Journal of Clinical Psychiatry 63:892–909, 2002Google Scholar
5. Dolder CR, Lacro JP, Jeste DV: Adherence to antipsychotic and nonpsychiatric medications in older patients with psychotic disorders. Psychosomatic Medicine 65:156–162, 2003Google Scholar
6. Gilmer TP, Dolder CR, Lacro JP, et al: Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. American Journal of Psychiatry 161:692–699, 2004Google Scholar
7. Valenstein M, Ganoczy D, McCarthy JF, et al: Antipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective review. Journal of Clinical Psychiatry 67:1542–1550, 2006Google Scholar
8. Terkelsen KG, Menikoff A: Measuring the costs of schizophrenia: implications for the post-institutional era in the US. Pharmacoeconomics 8:199–222, 1995Google Scholar
9. Ascher-Svanum H, Faries DE, Zhu B, et al: Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. Journal of Clinical Psychiatry 67:453–460, 2006Google Scholar
10. Weiden PJ, Olfson M: Cost of relapse in schizophrenia. Schizophrenia Bulletin 21: 419–429, 1995Google Scholar
11. Marcus SC, Olfson M: Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophrenia Bulletin 34: 173–180, 2007Google Scholar
12. Sun SX, Liu GG, Christensen DB, et al: Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Current Medical Research and Opinion 23:2305–2312, 2007Google Scholar
13. Osterberg L, Blaschke T: Adherence to medication. New England Journal of Medicine 353:487–497, 2005Google Scholar
14. Lacro JP, Dunn LB, Dolder CR, et al: Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. Journal of Clinical Psychiatry 63:892–909, 2002Google Scholar
15. Tarn DM, Heritage J, Paterniti DA, et al: Physician communication when prescribing new medications. Archives of Internal Medicine 166:1855–1862, 2006Google Scholar
16. Nielsen-Bohlman L, Panzer A, Kindig DA, et al: Health Literacy: A Prescription to End Confusion. Washington, DC, National Academies Press, 2004Google Scholar
17. Diaz E, Woods SW, Rosenheck R: Effects of ethnicity on psychotropic medications adherence. Community Mental Health Journal 41:521–537, 2005Google Scholar
18. Opolka JL, Rascati KL, Brown CM, et al: Role of ethnicity in predicting antipsychotic medication adherence. Annals of Pharmacotherapy 37:625–630, 2003Google Scholar
19. San Diego Region Fast Facts. San Diego, San Diego Association of Governments, Aug 2006Google Scholar
20. Ramirez Garcia JI, Chang CL, Young JS, et al: Family support predicts psychiatric medication usage among Mexican American individuals with schizophrenia. Social Psychiatry and Psychiatric Epidemiology 41:624–631, 2006Google Scholar
21. Barrio C, Palinkas LA, Yamada AM, et al: Unmet needs for mental health services for Latino older adults: perspectives from consumers, family members, advocates, and service providers. Community Mental Health Journal 44:57–74, 2007Google Scholar
22. Folsom D, Gilmer T, Barrio C, et al: A longitudinal study of the use of mental health services by persons with serious mental illness: do Spanish-speaking Latinos differ from English-speaking Latinos and Caucasians? American Journal of Psychiatry 164:1173–1180, 2007Google Scholar
23. Gilmer TP, Ojeda VD, Folsom DP, et al: Initiation and use of public mental health services by persons with severe mental illness and limited English proficiency. Psychiatric Services 58:1555–1562, 2007Google Scholar
24. California Health Interview Survey, 2005. Available at www.chis.ucla.edu Google Scholar
25. Kronick R, Gilmer T, Dreyfus T, et al: Improving health-based payment for Medicaid beneficiaries: CDPS. Health Care Financing Review 21:29–64, 2000Google Scholar
26. Efron B: An Introduction to the Bootstrap. New York, Chapman & Hall, 1993Google Scholar
27. Blough DK, Madden CW, Hornbrook MC: Modeling risk using generalized linear models. Journal of Health Economics 18: 153–171, 1999Google Scholar
28. Manning WG: The logged dependent variable, heteroscedasticity, and the retransformation problem. Journal of Health Economics 17:283–285, 1998Google Scholar
29. Schmidley AD: Profile of the Foreign-Born Population in the United States: 2000. Washington, DC, US Census Bureau, 2001Google Scholar
30. Kopelowicz A, Zarate R, Gonzalez Smith V, et al: Disease management in Latinos with schizophrenia: a family-assisted, skills training approach. Schizophrenia Bulletin 29: 211–217, 2003Google Scholar
31. Kim SW, Yoon JS, Choi SK: Survey of medication adherence in patients with schizophrenia: Korean ADHES data. Human Psychopharmacology 21:533–537, 2006Google Scholar
32. Li WW, Stewart AL, Stotts N, et al: Cultural factors associated with antihypertensive medication adherence in Chinese immigrants. Journal of Cardiovascular Nursing 21:354–362, 2006Google Scholar
33. Ponce NA, Ku L, Cunningham WE, et al: Language barriers to health care access among Medicare beneficiaries. Inquiry 43: 66–76, 2006Google Scholar
34. Smith M, Lin K, Mendoza R: "Nonbiological issues" affecting psychopharmacotherapy: cultural considerations, in Psychopharmacology and Psychobiology of Ethnicity. Edited by Lin K, Poland R, Nakasaki G. Washington DC, American Psychiatric Press, 1993Google Scholar
35. Lin KM, Cheung F: Mental health services for Asian Americans. Psychiatric Services 48:539–540, 1999Google Scholar
36. Ngo-Metzger Q, Massagli MP, Clarridge BR, et al: Linguistic and cultural barriers to care. Journal of General Internal Medicine 18:44–52, 2003Google Scholar
37. Ngo-Metzger Q, Sorkin DH, Phillips RS, et al: Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. Journal of General Internal Medicine S2:324–330, 2007Google Scholar



