Service Utilization and Help Seeking in a National Sample of Female Rape Victims
A growing body of literature reveals a significant imbalance between the prevalence of mental disorders and utilization of mental health services. The Epidemiologic Catchment Area study, conducted from 1980 to 1985, reported that individuals diagnosed as having a mental disorder sought treatment in the past year ( 1 ) and that help seeking was more likely to occur among individuals with a history of sexual assault ( 2 ). The National Comorbidity Survey, conducted from 1990 to 1992, estimated that only 25% of respondents with a mental disorder received treatment within the past year ( 3 ). The National Comorbidity Survey Replication ( 4 ), conducted between 2001 and 2003, estimated that 41% of respondents with a diagnosis of a mental disorder received past-year treatment. Taken together, these studies suggest that increases in mental health service utilization among those with mental disorders have occurred over the past two decades but that levels of use among those in need of care remain low.
A key finding of the National Comorbidity Survey Replication was that patterns of service use differed by the type of disorder ( 4 ). That is, significant variability exists across populations in perceived need for treatment, and it follows that determinants of help seeking may also differ by disorder. This underscores the potential value of research that isolates specific at-risk populations in an attempt to identify unique predictors of service use as well as modifiable factors that may be targeted by intervention.
Studies on help seeking in traumatic stress populations (for example, rape victims and adults with posttraumatic stress disorder [PTSD]) have revealed a similarly striking disconnect between the number of individuals receiving a diagnosis and those who initiate services ( 5 , 6 , 7 ), and further, this disconnect has been noted specifically within populations of rape victims ( 8 ). However, only a handful of studies have examined help-seeking behavior in traumatic stress populations, and none has examined how different types of rape (for example, forcible rape versus drug- or alcohol-facilitated rape) may be related to victims' likelihood of seeking help and characteristics of help-seeking behavior (for example, seeking help from a religious figure versus a psychologist).
Research of this nature has high public health significance, because rape affects about one in seven U.S. women at some time in their lives ( 9 , 10 ) and because rape is associated with a wide range of mental health difficulties ( 11 , 12 , 13 , 14 ), as well as substance use disorders ( 12 ). Further, different types of rape may relate in unique ways to victims' help-seeking decisions because of stigma issues, self-blame, and other factors ( 15 , 16 ). For example, forcible rape is more likely than incapacitated rape to be reported to law enforcement ( 17 ). The study presented here explored these issues by examining factors associated with distinct categories of help-seeking behavior by using a national probability sample of female victims of forcible rape, incapacitated rape, and drug- or alcohol-facilitated rape.
We examined demographic characteristics, rape history, incident characteristics, psychopathology, and substance abuse variables in relation to various forms of formal help seeking, which were based on categories of help seeking from past research ( 2 , 18 ). On the basis of previous research, we hypothesized that experiencing more than one assault, having a history of psychopathology, and having a history of substance abuse would be positively associated with ever seeking help ( 5 , 8 , 19 ). In regard to specific rape types, it was thought that forcible rape would be associated with increased likelihood of ever seeking help, compared with other types of rape ( 17 ).
Methods
Participants
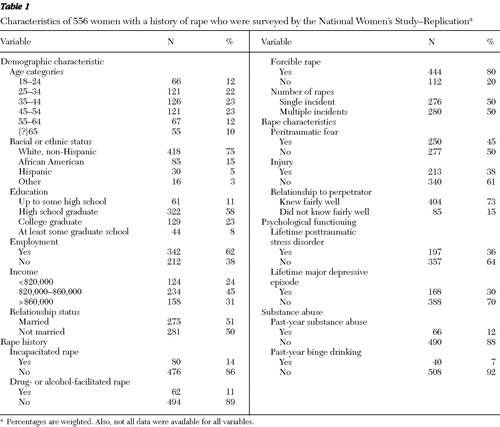
Data from this study came from the National Women's Study-Replication. The household sample of 3,001 women was formed from two population samples: a national cross-section of 1998 women aged 18 to 34, plus a cross-section of 998 women aged 35 and older, and five women who refused to provide their age. Weights were used for all analyses with this sample to maximize representativeness by bringing the distribution of sample characteristics in line with census figures. Of these women, only those endorsing a history of at least one rape experience were included in analyses. This sample of women with a rape history consisted of 556 women (aged 18 to 76 years) with a mean±SD age of 42.91±15.08.
We used random-digit-dial methodology involving three steps. First, the sample was geographically stratified with sample allocation proportionate to population distribution. Second, a sample of assigned telephone banks was randomly selected from an enumeration of the "working residential hundreds block" (defined as each block of 100 potential telephone numbers with an exchange that includes one or more residential listings) within the active telephone exchanges within the strata. Third, a two-digit number was randomly generated by computer for each working residential hundreds block. All interviews were conducted between January 23, 2006, and June 26, 2006.
Measures
Help seeking. To determine whether participants ever sought help, they were asked, "Have you ever contacted a professional for help with emotional problems?" If they answered yes, they were asked whether they contacted a medical professional, a religious counselor (priest, minister, or rabbi), or a mental health professional (psychiatrist, psychologist, social worker, or other therapist). Participants were not specifically asked whether they had sought help in regard to emotional problems resulting from being raped.
Rape experiences. We assessed women's most recent incident of rape (or only incident, if there was only one) and, if applicable, the first incident of rape. Rape was defined as penetration of the victim's vagina, mouth, or rectum without consent. Cases were defined as forcible rape if the perpetrator used force or threat of force. The key element of incapacitated rape was that the victim perceived the perpetrator to have raped her when she was intoxicated and impaired via voluntary intake of drugs or alcohol by the victim. In contrast, the key element of drug- or alcohol-facilitated rape was that the perpetrator was perceived by the victim as having deliberately attempted to produce incapacitation by administering drugs or alcohol to the victim. In both drug- or alcohol-facilitated rape and incapacitated rape cases, the victim was unable to consent as a result of incapacitation (for example, lack of consciousness, awareness, or ability to control behavior). Questions were closed ended and behaviorally specific.
Classification of individuals into rape categories was based on the history of each type of rape; classification was nonmutually exclusive. For example, women who reported a history of forcible rape as their most recent or only incident but who also reported a first incident that met criteria for drug- or alcohol-facilitated rape were considered to have a history of both forcible rape and drug- or alcohol-facilitated rape. Women who reported elements of multiple rape types during that same incident were classified as having experienced each rape type they endorsed for that incident.
Rape characteristics. Rape characteristics assessed included whether they had experienced fear of death or injury, whether they experienced physical injury, and whether they knew the perpetrator. Relationship to the perpetrator was assessed by asking women whether they "knew the [perpetrator] fairly well or not." For women who reported multiple incidents, we used data from the most recent incident.
Mental health. PTSD and major depressive episode were assessed with the PTSD and major depressive episode modules from the National Women's Study; the modules consisted of structured interviews based on DSM-IV ( 20 ) criteria ( 21 , 22 ). Research on the PTSD module from the National Women's Study has provided support for the module's concurrent validity and several forms of reliability (for example, temporal stability, internal consistency, and diagnostic reliability) ( 14 , 23 ). The major depressive episode module assesses hallmark symptoms of depression, including persistent feelings of sadness and loss of interest or pleasure. Support for internal consistency and convergent validity of the module exist ( 14 ). Functional impairment was also assessed as part of the PTSD and major depressive episode modules.
Substance use. Two substance use outcomes were measured in this study: past-year binge drinking and past-year substance abuse. Past-year binge drinking was defined as consumption of five or more drinks of an alcoholic beverage with at least monthly frequency (at least 12 or more days within the past year). To assess binge drinking, women were asked to estimate the number of days in the past 12 months that they consumed five or more drinks of alcoholic beverages. Past-year substance abuse was assessed with the substance use module from the National Women's Study interview, approximating the criteria set forth by the DSM-IV. These criteria were modified to include women meeting criteria for dependence as well as abuse and have been shown to have adequate face validity, because these criteria have been shown to be significantly associated with a higher mean number of heavy drinking days and a higher mean number of days of reported intoxication ( 12 ). (Interview measures are available upon request.)
Procedure
Women were interviewed with a computer-assisted telephone interviewing system. This system is designed to reduce interviewer error in both data collection and data recording. Because of the nature of the study, only experienced female interviewers were involved in survey procedures. English and Spanish versions of the interview were developed; the version administered was based on respondent preference. Completed interviews averaged 20 minutes.
After determining that the residence contained one or more women eligible for the study, the interviewer introduced the study and provided a toll-free telephone number to confirm authenticity of the study. When a residence had more than one woman who met study criteria, the woman with the most recent birthday was selected. Whenever possible, women were interviewed immediately after respondent selection was determined. Otherwise, appointments were scheduled or blind callbacks were made at different times of day and days of the week. A minimum of five callbacks were made before a case was abandoned. This study was approved by an institutional review board. After a complete description of the study was provided, oral consent was obtained.
Statistical analyses
Logistic regression analyses were conducted to identify variables within each predictor set that were associated with each of the four help-seeking variables (ever sought services and sought services from medical professionals, religious figures, and mental health professionals). Significant predictors emerging from these analyses were entered into a final multivariable logistic regression analysis. A count of types of services utilized was computed, ranging from zero (the participant did not seek help) to three (the participant sought all three types of help). Linear regression analyses were conducted by using the same method as described above for the binary outcome variables.
Results
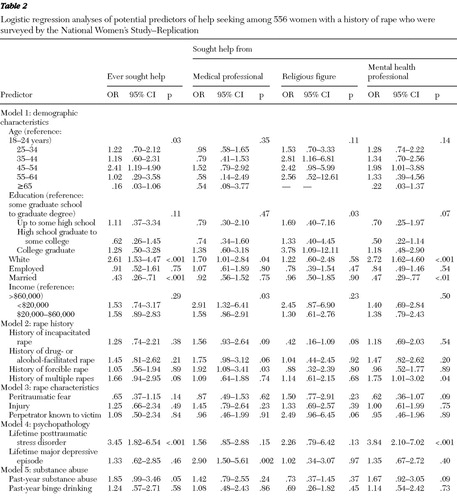
Sample characteristics for the subsample of rape victims extracted from the national sample are described in Table 1 . Prevalence of help seeking in this sample was high. More than half of the sample reported ever seeking help (60%). In regard to specific types of help sought, 38% went to a medical professional, 15% sought religious counsel, and 54% sought help from a mental health specialist. (Percentages are weighted.) Table 2 describes results of logistic regression analyses within each predictor set.
 |
 |
Ever sought services
Significant demographic predictors that were related to odds of ever having sought services were being 45 to 54 years of age (OR=2.41), being white (OR=2.61), and being married (OR=.43). No rape history variables or rape characteristics were related to the outcome variable. For the psychopathology analysis, only PTSD was related to increased odds of ever seeking help (OR=3.45). Finally, substance abuse was marginally predictive of ever seeking help (OR=1.85). The significant predictors were entered into a multivariate model ( Table 3 ), and only white race, PTSD, and being unmarried remained significantly positively associated with ever seeking help.
 |
Medical professional. Among demographic variables, white race (OR=1.70) and income of less than $20,000 (OR=2.91) were predictive of seeking medical services. Forcible rape (OR=1.92) was the only rape variable related to seeking help from a medical professional. No rape characteristics were predictive. Only major depressive episode (OR=2.90) was predictive of help seeking. Neither substance abuse variable was significantly related. The final multivariate analysis revealed that only major depressive episode remained significant in predicting seeking help from a medical professional.
Religious counsel. Having a college education (OR=3.78) was the only variable that was related to seeking religious counsel. The final multivariate model revealed no significant predictors of seeking religious counsel.
Mental health professional. Many variables were related to seeking help from a mental health professional. Among the demographic variables, being white (OR=2.73) and being married (OR=.47) were associated with seeking help. History of multiple rapes (OR=1.75) was the only significant rape history variable that predicted help seeking from a mental health professional. PTSD (OR=3.84) was associated with seeking mental health treatment. Neither substance abuse variable was significantly related. All variables, except history of multiple rapes, remained significant in the final model.
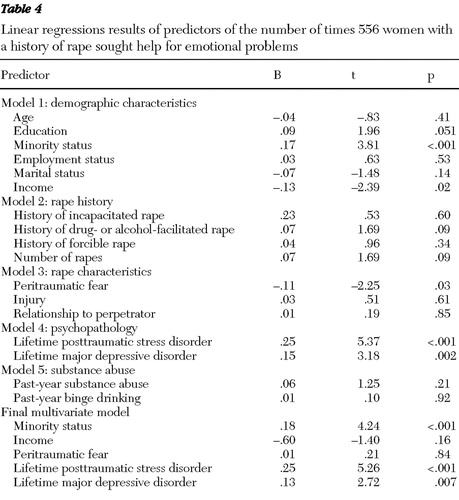
Number of services
Results from linear regression analyses predicting the number of services utilized are reported in Table 4 . Minority status and income were significant predictors. No variables were significant among the different types of rape. Among the rape characteristics, peritraumatic fear was a significant predictor. Both PTSD and major depressive episode were significant predictors, whereas neither substance abuse variable was related. In the final model, minority status, PTSD, and major depressive episode were significantly associated with the number of services sought.
 |
Discussion
To our knowledge, this is the first study to examine determinants of different forms of service utilization in a large national sample of rape victims. In our sample, white women were more likely than women from a minority group to report help seeking; specifically, white race was the only consistent predictor of help seeking among rape victims. These results are consistent with previous studies that have found that persons from minority groups are less likely to seek treatment after assault ( 5 ). Although community-level factors have been shown in previous studies to make some contribution to health care disparities, research suggests that individual factors, such as race and ethnicity, remain central in contributing to disparities ( 24 ).
PTSD was related to ever seeking treatment, number of services accessed, and seeking mental health treatment. One potential explanation is that PTSD is a complex constellation of symptoms that may be more likely to be diagnosed by a mental health professional than by a general medical professional. Interestingly, lifetime depression was a significant predictor of seeking medical help and was not a predictor of mental health service utilization. Although Lewis and colleagues ( 19 ) previously found that depression was predictive of formal help seeking among women, unlike the study presented here, they did not differentiate between medical professionals and mental health professionals. Depression is frequently associated with worse global health ratings, more reported health concerns, and more severe concerns, a greater likelihood of seeking medical treatment for unexplained physical symptoms, and more emergency room visits, and some evidence suggests that depression mediates the relation between PTSD diagnosis and physical health complaints ( 25 , 26 , 27 ). This strong relation between depression and physical health may serve to partially explain its prediction of medical service utilization in this study. Further research could elucidate factors influencing rape victims' decision to seek medical rather than mental health services for their depressive symptoms.
The women in our sample endorsed relatively high rates of past-year substance abuse, underscoring the importance of standard assessment for substance use disorders in this population. The elevated rate of substance abuse among rape victims is consistent with previous research ( 12 , 14 , 28 ), and lack of a strong relationship between substance use and help seeking also is consistent with prior studies ( 6 ). It is possible, given the wording of our question ("Have you ever contacted a professional for help with emotional problems?"), that we underdetected receipt of services for substance use disorders. Further, several service modalities often used to treat substance abuse (for example, group therapy, inpatient hospitalization, residential treatment, and day treatment) were not specifically referenced in the prompts for type of service provider.
Neither type of rape nor history of multiple rapes was found to be important with respect to help seeking. One possible explanation for this finding is that this study assessed general help seeking, not assault-related help seeking. Because forcible rape has been found in previous studies to be associated with greater life disruption, compared with other forms of rape ( 29 , 30 ), it was hypothesized that forcible rape would be associated with higher rates of help seeking than drug- or alcohol-facilitated rape and incapacitated rape. This hypothesis was not supported. However, a majority of our sample had experienced a forcible rape (nearly 80%), thereby limiting our power to detect possible differences among rape types. Additionally, no incident characteristics were predictive of help seeking in this sample.
This was one of the first studies to examine social and psychological correlates of multiple forms of help seeking by using a large, representative sample of adult rape victims. This study also had several limitations. First, findings were based strictly on retrospective self-report data, which introduces potential recall biases. Second, our interview was necessarily brief because a lengthy interview would have been cost-prohibitive. Use of a brief interview prevented a comprehensive assessment of help seeking (for example, amount of help seeking, informal help seeking, and forensic medical examination postrape), as well as the temporal directionality of rape, mental health outcomes, substance abuse, and help seeking. Additionally, other forms of potentially traumatic events that have an impact on help seeking ( 8 ), such as physical assault and child sexual abuse, were not assessed. It should also be noted that this study examined general help seeking for emotional problems among rape victims and is therefore not restricted to rape-specific help seeking. Finally, future research should include analysis of possible interactions between incident characteristics and rape type.
In addition to addressing the aforementioned limitations, future research in this area should continue to explore variables associated with women's choice of provider. Our data suggest that those who seek help do so from approximately two modalities, yielding a potentially high societal cost. Also, the finding that two-fifths of women never sought formal help of any kind underscores the need for further research on barriers to care, particularly within populations who are traditionally underserved (for example, ethnic minority groups). Such information could inform public health campaigns that are aimed at both treatment seekers and treatment providers.
Conclusions
Several notable findings emerged: minority status decreased odds of help seeking, mirroring previous findings of health disparities as a function of race or ethnicity; PTSD and major depressive episode were differentially predictive of seeking mental health services and medical services; although prevalent in our sample, substance abuse was not associated with help seeking; and help seeking was not associated with specific types of rape or by the cumulative effect of traumatic events.
Results strengthen the call for increased provision of targeted psychoeducation for practitioners and policy makers. With PTSD being a predictor of seeking mental health services, practitioners at all levels of service delivery should be informed of the availability of existing empirically supported treatments, both pharmacologic and psychotherapeutic ( 31 , 32 ), for PTSD. This should be incorporated into training programs and included in continuing education for practitioners. Public policy implications also exist in that insurance reimbursement for PTSD and other mental health conditions should be provided, which may assist in addressing an important barrier to help-seeking in this population. Consistent with previous studies, women from ethnic minority groups were less likely to seek formal help for emotional problems. Targeted interventions should be aimed specifically at this group of women with the primary goal of addressing and reducing existing barriers to care.
Acknowledgments and disclosures
This research was supported by grant 2005-WG-BX-0006 from the National Institute of Justice (NIJ). Views expressed in this article do not necessarily represent those of NIJ.
The authors report no competing interests.
1. Narrow WE, Regier DA, Rae DS, et al: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Archives of General Psychiatry 50:95–107, 1993Google Scholar
2. Golding JM, Stein JA, Siegel JM, et al: Sexual assault history and use of health and mental health services. American Journal of Community Psychology 16:625–644, 1988Google Scholar
3. Kessler RC, Zhao S, Kats SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156: 115–123, 1999Google Scholar
4. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629–640, 2005Google Scholar
5. Koenen KC, Goodwin R, Struening E, et al: Posttraumatic stress disorder and treatment seeking in a national screening sample. Journal of Traumatic Stress 16:5–16, 2003Google Scholar
6. Ullman SE, Brecklin LR: Sexual assault history, PTSD, and mental health service seeking in a national sample of women. Journal of Community Psychology 3:261–279, 2002Google Scholar
7. Kimerling R, Calhoun KS: Somatic symptoms, social support, and treatment seeking among sexual assault victims. Journal of Consulting and Clinical Psychology 62:333–340, 1994Google Scholar
8. Ullman SE: Mental health services seeking in sexual assault victims. Women and Therapy 30:61–84, 2007Google Scholar
9. Kilpatrick DG, Edmunds CN, Seymour AK: Rape in America. Charleston, SC, National Victim Center, 1992Google Scholar
10. Tjaden P, Thoennes N: Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women: Findings From the National Violence Against Women Survey. Washington, DC, National Institute of Justice, US Department of Justice, 2000Google Scholar
11. Kessler RC, Sonnega A, Bromet E, et al: Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 52:1048–1060, 1995Google Scholar
12. Kilpatrick DG, Acierno R, Resnick HS, et al: A 2-year longitudinal analysis of the relationship between violent assault and substance abuse in women. Journal of Consulting and Clinical Psychology 65:834–847, 1997Google Scholar
13. Kilpatrick DG, Acierno R, Schnurr PP, et al: Risk factors for adolescent substance abuse and dependence: data from a national sample. Journal of Consulting and Clinical Psychology 68:19–30, 2000Google Scholar
14. Kilpatrick DG, Ruggiero KJ, Acierno R, et al: Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology 71:692–700, 2003Google Scholar
15. Filipas HH, Ullman SE: Social reactions to sexual assault victims from various support sources. Violence and Victims 16:673–692, 2001Google Scholar
16. Starzynski LL, Ullman SE, Filipas HH, et al: Correlates of women's sexual assault disclosure to informal and formal support sources. Violence and Victims 20:417–432, 2005Google Scholar
17. Kilpatrick DG, Resnick HS, Ruggiero KJ, et al: Drug-Facilitated, Incapacitated, and Forcible Rape: A National Study: Final Report Submitted to the National Institute of Justice. Washington, DC, National Institute of Justice, 2007Google Scholar
18. Golding JM, Siegel JM, Sorenson SB, et al: Social support sources following sexual assault. Journal of Community Psychology 17:92–107, 1989Google Scholar
19. Lewis SF, Resnick HS, Ruggiero KJ, et al: Assault, psychiatric diagnoses, and sociodemographic variables in relation to help-seeking behavior in a national sample of women. Journal of Traumatic Stress 18:97–105, 2005Google Scholar
20. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
21. Acierno R, Resnick H, Kilpatrick DG, et al: Risk factors for rape, physical assault, and posttraumatic stress disorder in women: examination of differential multivariate relationships. Journal of Anxiety Disorders 13:541–563, 1999Google Scholar
22. Ruggiero KJ, Smith DW, Hanson RF, et al: Is disclosure of childhood rape associated with mental health outcome? Results from the National Women's Study. Child Maltreatment 9:62–77, 2004Google Scholar
23. Resnick HS, Kilpatrick DG, Dansky BS, et al: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology 61:984–991, 1993Google Scholar
24. Stockdale SE, Tang L, Zhang L, et al: The effects of health sector market factors and vulnerable group membership on access to alcohol, drug, and mental health care. Health Services Research 42:1020–1041, 2007Google Scholar
25. Elhai JD, North TC, Frueh BC: Health Service Use Predictors Among Trauma Survivors: A Critical Review. Psychological Services 2:3–19, 2005Google Scholar
26. Newman MG, Clayton L, Zuellig A, et al: The relationship of childhood sexual abuse and depression with somatic symptoms and medical utilization. Psychological Medicine 30:1063–1077, 2000Google Scholar
27. Kimerling R, Clum GA, Wolfe J: Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: replication and extension. Journal of Traumatic Stress 13:115–128, 2000Google Scholar
28. Burnam MA, Stein JA, Golding JM, et al: Sexual assault and mental disorders in a community population. Journal of Consulting and Clinical Psychology 56:843–850, 1988Google Scholar
29. Abbey A, BeShears R, Clinton-Sherrod AM, et al: Similarities and differences in women's sexual assault experiences based on tactics used by perpetrator. Psychology of Women Quarterly 28:323–332, 2004Google Scholar
30. Testa M, Livingston JA, Vanzile-Tamsen C, et al: The role of women's substance use in vulnerability to forcible and incapacitated rape. Journal of Studies on Alcohol 64:756–764, 2003Google Scholar
31. Amstadter AB, McCart M, Ruggiero KJ: Psychosocial interventions for adults with crime-related PTSD. Professional Psychology: Research and Practice 38:640–651, 2007Google Scholar
32. Kilpatrick DG, Amstadter AB, Resnick HS, et al: Rape related PTSD: issues and interventions. Psychiatric Times 24:7, 2007Google Scholar



