Admission to Women's Crisis Houses or to Psychiatric Wards: Women's Pathways to Admission
Women's crisis houses are an innovative alternative to psychiatric hospital admission. Admission to crisis houses is potentially less stigmatizing and coercive, and the houses themselves are less "institutional." A women's crisis house is a residential mental health crisis facility for women who would otherwise be considered for hospital admission. The development of women's crisis houses has been recommended by the U.K. Department of Health and designated a priority by the National Institute for Mental Health in England ( 1 ).
The few descriptions and evaluations of women's crisis houses have had substantial methodological limitations. Previous findings suggest that women's crisis houses admit women with severe and enduring mental health problems. For example, a retrospective study of a random sample of 100 admissions to a women's crisis house in North London found that women were most commonly admitted for suicidal ideation or self-harm and more than a fifth were admitted because of a relapse of psychosis ( 2 ). A prospective observational study of more than 250 admissions to a women's crisis house in South London found a significant improvement from admission to discharge in scores on the Brief Psychiatric Rating Scale, symptom scores on the Beck Depression Inventory, Global Assessment of Functioning scores, and number of unmet needs ( 3 ). These findings of improvement suggest that the women's crisis house was effective in treating women who needed admission; however, no control group was included in the study.
A qualitative study comparing women's experience of admission to a women's crisis house and admission to general acute wards in the same catchment area found that, in general, women's crisis houses were highly valued by service users ( 4 ). The women reported that their recovery was promoted by the homelike environment of the crisis house, the absence of disturbed male patients, the ready availability of staff for talking through current and past difficulties, and good support from other residents; however, the women admitted to the crisis house perceived that the service was relatively selective, both in excluding those who were not severely ill enough to be considered for hospital admission and in filtering out very unwell women who were unable to take responsibility for their own safety.
Observational research conducted in a mixed-gender crisis house in North England found that after admission to the crisis house, use of acute psychiatric wards and accident and emergency departments decreased over the following year ( 5 ). However, this study did not use a control group, and thus the finding is difficult to interpret. There has been one randomized controlled trial of admission to a general hospital compared with admission to a mixed-gender crisis house ( 6 ). The study found a similar case mix in both types of service, and patient satisfaction was comparable in the two settings. However, no controlled quantitative studies have compared admissions to women's crisis houses and traditional psychiatric wards. It is also not clear from the studies described above what factors predict admission to a crisis house when both a crisis house and a psychiatric ward are available. In addition, no research has compared pathways to admission to women's crisis houses and to psychiatric wards and investigated whether differences in pathways reflect the case mix in the two settings. A pathway to admission or care is defined as "the sequence of contacts with individuals and organizations prompted by the distressed person's efforts, and those of his or her significant others, to seek help as well as the help that is supplied in response of these efforts" ( 7 ).
The study examined three hypotheses. First, women admitted to psychiatric hospital wards are more likely to have a psychotic disorder than women admitted to women's crisis houses. Second, women admitted to psychiatric hospital wards have a history of more hospital admissions over the previous two years than women admitted to women's crisis houses. The third hypothesis was that women admitted to psychiatric hospital wards have more adverse pathways (contact with police or accident and emergency services before admission) and more complex pathways (a greater number of contacts with services) to admission than women admitted to women's crisis houses.
We therefore compared the sociodemographic and clinical characteristics of women admitted to women's crisis houses and women admitted to traditional psychiatric wards and investigated whether pathways to admission differed for the two types of service.
Methods
We used a retrospective survey study design, obtaining data as soon as possible after the day of admission. Data on referral pathways of all admissions to women's crisis houses and hospital wards were collected over 12 weeks. Deidentified information was obtained from clinicians about the referral pathways, demographic characteristics, and details of illness for each woman.
Setting
The study was conducted in four London boroughs—Croydon, Lambeth, Camden, and Islington—where psychiatric services include traditional psychiatric wards, home treatment teams, and women's crisis houses. Both the traditional psychiatric wards and women's crisis houses admit women aged 18 and over. The women's crisis houses are all located on an ordinary residential street, have a domestic atmosphere, and are funded by the U.K. National Health Service. Staff are available 24 hours a day and are either nurses or health care workers with a background in mental health. Women's crisis houses are not permitted to admit women who are detained under the Mental Health Act at admission (that is, all admissions to the crisis houses are voluntary). In addition, women who are considered to be at risk of violent behavior, who are misusing drugs or alcohol such that they require detoxification under medical supervision, or who are unable to engage in a safety plan and therefore need constant supervision are not admitted to women's crisis houses.
Three women's crisis houses were included in this study (one of the houses served women from two boroughs). The Croydon women's crisis house, which opened in 1999, is a nursing-led service with support from a female psychiatrist. It has eight beds and a mean length of stay of 21 days. Referral is made by telephone, by the woman herself, or by a concerned other (including family members, friends, neighbors, or health professionals). If telephone assessment finds that admission is appropriate, the woman is invited to see a staff member at the women's crisis house for further assessment. The Croydon catchment area has two psychiatric wards—a women-only ward and a mixed-gender acute psychiatric ward.
The Lambeth women's crisis house opened in South London in 2004. It has nine beds, a mean length of stay of 28 days, and an assessment process similar to that of the Croydon women's crisis house (although without self-referral). Almost all women in this catchment area who are admitted to hospitals are accommodated in women-only hospital wards. The North London women's crisis house opened in December 1995 and serves the inner-London boroughs of Camden and Islington. It has 12 beds (plus four beds for children) and a mean length stay of 19 days. Both self-referrals and referrals from professionals are accepted. After referral, women are invited to come to the house for assessment. Camden has a women-only inpatient ward. Islington has an enhanced women-only ward and mixed wards.
Sample
The sample consisted of all 388 female admissions (338 women) admitted to an acute psychiatric inpatient ward or a women's crisis house in the boroughs of Croydon, Lambeth, Camden, and Islington during a 12-week period in 2006 from mid-April to mid-July. A total of 191 women (56%) were white, 111 (33%) were black (black African and black Caribbean), and 31 (9%) were Asian or of other ethnic groups. Information about race-ethnicity was not recorded for five women.
Instruments
A questionnaire was designed and piloted for the purpose of studying pathways to admission. It included reasons for admission and a modified version of the World Health Organization's Pathways to Care Schedule ( 8 ). Information about the pathway to admission included who initiated contact with mental health services and details of when the acute crisis started, the number of contacts on the pathway to admission (with statutory services, such as police, general practitioners, and care coordinators, as well as with informal sources, such as family members and neighbors); whether there was previous contact with mental health services; and whether the patient had an allocated care coordinator (that is, a mental health care professional with a background in nursing, social work, or occupational therapy who coordinates care for patients under the care of mental health services).
The Threshold Assessment Grid (TAG) ( 9 ) was used as an indicator of severity of the psychiatric disorder. The TAG is a standardized brief assessment of the severity of an individual's mental health problems; when rated by mental health professionals it has an intraclass correlation for total TAG scores of .58 ( 10 ). The TAG was completed by the researchers on the basis of key workers' ratings as soon as possible after admission. The severity of the patient's difficulties was rated in three areas: safety, risk, and needs and disabilities. A TAG score of 5 or more indicates moderately severe problems that need secondary mental health care. Data also were collected on whether the patient was detained under the Mental Health Act either at or during the admission, demographic characteristics (census categories for ethnicity were used), and clinical diagnoses based on ICD-10 criteria.
Informed consent was not obtained from individual women because the data were collected anonymously from clinicians. Ethical approval was obtained from the University College London Hospital Research Ethics Committee.
Data collection and analysis
Immediately after each admission, the questionnaire was completed by mental health staff familiar with the circumstances of the patient's admission. Additional information was obtained from medical notes in the patient's record.
SPSS version 12 was used for data analysis. Descriptive statistics, chi square tests, and t tests and nonparametric tests were used to identify any significant sociodemographic differences between women admitted to women's crisis houses and those admitted to psychiatric wards. Because some women were admitted more than once, the analysis then focused on differences between admissions to women's crisis houses and admissions to psychiatric wards. Data were dichotomized when appropriate—for example, employment status was categorized as employed (including student status) or not employed (including voluntary work). Forward stepwise logistic regression models were then used to examine possible associations between potential predictors and the dependent variable (admission to a women's crisis house). Models included a history of admission, employment status, ethnicity, current contact with mental health services, having a care coordinator, type of accommodation, living arrangements, having children under age 16, inpatient discharge within the last month, primary diagnosis, diagnosis of personality disorder, comorbid substance misuse, TAG score, number of contacts on the pathway to admission, and nature of contacts (that is, with police, a general practitioner, or accident and emergency services). These models were based on a complete case analysis because a preliminary analysis revealed no factors associated with missing data. The Bonferroni correction for multiple testing was used for analysis of differences in reasons for admission.
Results
Of the 388 female admissions during the study period of 12 weeks in the four London boroughs under investigation, 41 women had more than one admission. A total of 301 admissions were to wards, and 87 admissions were to women's crisis houses. The mean±SD age of women admitted to women's crisis houses was 40.4±11.2 years, and for women admitted to wards it was 40.0±13.0 years (not a significant difference).
Demographic characteristics
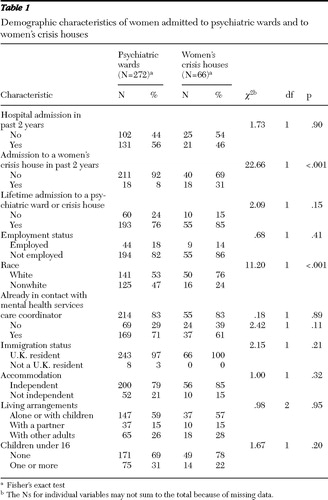
As shown in Table 1 , women admitted to a women's crisis house were significantly more likely than women admitted to a hospital ward to have been admitted to a women's crisis house in the previous two years. We also found that compared with nonwhite women, white women were significantly more likely to have been admitted to a women's crisis house than a hospital ward.
 |
Clinical characteristics and pathways
Results of the univariate analysis in Table 2 showed that admissions to a women's crisis house were significantly more likely to have a primary diagnosis of a nonpsychotic disorder. No significant between-group difference was found in the mean TAG scores. Women admitted to crisis houses were significantly more likely to have seen a general practitioner before the admission and less likely to have been seen at an accident and emergency department or to have had contact with police before admission. Pathways to admission were significantly less complex (fewer contacts) for women admitted to women's crisis houses.
 |
A total of 108 women were detained under the Mental Health Act. Because women's crisis houses do not admit women detained under the act, there was a significant difference between the two groups on this variable ( χ2 =40.12, df=1, p<.001). In addition, status in regard to the Mental Health Act was associated with ethnicity—nonwhite women were significantly more likely than white women to be admitted under a section of the act (61% compared with 39%; χ2 =27.74, df=1, p<.001). Women admitted voluntarily who were later detained under the act (N=28) were all on wards rather than in a crisis house ( χ2 =13.12, df=1, p<.001); however, it cannot be determined from these data whether this difference reflects the illness severity of women admitted to the respective facilities or the nature of the environment.
Multivariate analysis
In the multivariate analysis, after adjustment for center, admissions where women had a care coordinator and where the pathway to admission involved the police or accident and emergency services were significantly less likely to be to a women's crisis house; admissions of white women were significantly more likely to be to a women's crisis house ( Table 3 ).
 |
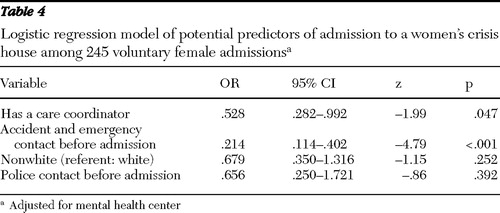
Because women detained under the Mental Health Act are not admitted to women's crisis houses, the multivariate analysis was repeated to compare pathways to admission only for voluntary admissions to hospital wards and women's crisis houses ( Table 4 ). In this model, ethnicity and police involvement were not significant. However, having a care coordinator or having had contact with an accident and emergency department on the pathway to admission remained significantly associated with admission to a psychiatric ward.
 |
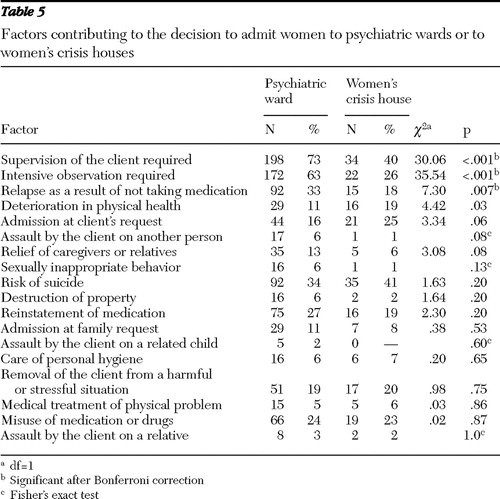
Reasons for admission were then examined with chi square tests. At a nominal significance level of .05, significant reasons for admission to a psychiatric ward were that supervision of the client was required, that intensive observation was required, and that relapse as a result of not taking medication was evident; deterioration in physical health was significantly associated with admission to a crisis house. However, after a Bonferroni correction (p=.0025) only the three reasons for admission to a psychiatric ward were significant ( Table 5 ).
 |
Discussion
We found few differences in the pathways to admission to women's crisis houses and to psychiatric wards. Results of the multivariate analysis indicated that for admissions to women's crisis houses, women were less likely to have a care coordinator or to have had contact with an accident and emergency department, but no other clinical or sociodemographic differences between voluntary admissions to crisis houses or psychiatric wards were found. We therefore did not find evidence to support our first hypothesis that among female admissions to psychiatric hospital wards, the women were more likely to have a psychotic disorder than among female admissions to women's crisis houses.
Although nonwhite women were significantly less likely than white women to be admitted to women's crisis houses, the association appears to reflect their significantly higher rate of detention under the Mental Health Act. Many studies have found high rates of detention under the act for nonwhite groups ( 11 , 12 ). When only voluntary admissions were included in the multivariate analysis, ethnicity was no longer an independent predictor of admission to psychiatric wards.
Our second hypothesis was also not supported; our data showed that for female admissions to psychiatric hospital wards, women did not have a history of more hospital admissions. Of note, however, was the finding that for admissions to women's crisis houses, women were more likely to have a previous admission to a women's crisis house. We found evidence to support our third hypothesis—pathways to admission were more adverse and complex for admissions to psychiatric hospital wards than for admissions to women's crisis houses. Among female admissions to psychiatric hospital wards, there was a higher likelihood of contact with an accident and emergency department or contact with the police before admission than among admissions to a women's crisis house; female admissions to psychiatric wards were also characterized by more contacts with services before admission.
It is unclear why women who visited accident and emergency departments were more likely to be admitted to wards. The difference may reflect staff preferences or patient characteristics that were not examined in this study. An investigation of factors associated with being admitted to a hospital rather than being managed at home by a crisis resolution and home treatment team also found that being assessed in an accident and emergency department was associated with a greater likelihood of hospital admission when adjustment was made for a range of other factors ( 13 ). Patients' and caregivers' expectations that hospital admission will ensue from admission to an accident and emergency department is one potential factor. The proximity of hospital wards and the context of assessment, in which it is difficult to assess social factors in the crisis and the persons' ability to cope with daily living activities, may also play a part. Similarly, the association between having a care coordinator and being admitted to a psychiatric ward may reflect staff preferences or the more complex mental health needs of patients in contact with secondary mental health services. However, other clinical factors, including previous history of service contacts, number of hospital admissions, diagnosis, TAG score, and a low level of employment, were not associated with admission to either a crisis house or a ward, which suggests that women's crisis houses were admitting patients with complex and severe mental health problems. This study therefore suggests that women's crisis houses are a viable alternative to psychiatric wards for women who need admission to a psychiatric facility but who do not need intensive observation or detoxification and are not violent.
Examination of reasons for admission also found few differences between the two types of service. Not surprisingly there were significantly more women admitted to hospital wards because they needed intensive observation or supervision, but the only other significant difference after correcting for multiple testing was that women who experienced a relapse as a result of not taking medication were more likely to be admitted to a ward.
This study has several limitations. Many different clinicians reported the data retrospectively, although the data were collected soon after admission and clinician recall should not have been a major problem. For practical reasons the data were not collected from patients but only from clinicians and therefore reflected clinicians' knowledge of the patients and their pathways to care, although there is no reason to believe that there would be systematic bias in clinicians' reports. Interrater consistency could not be measured for practical reasons, because many busy clinicians were involved in rating the women who were admitted. The study's strengths are its large sample size, the use of three different women's crisis houses and psychiatric wards in the same catchment areas, and the use of a previously well-validated measure of pathways to care.
This study could not address several important questions. We did not ask the women themselves which service they preferred and why, and we were also unable to explore why staff in the community arranged admission into one type of service rather than the other. However, perhaps the most important questions still to be addressed are whether women's crisis houses are as effective and cost-effective as psychiatric wards and whether they are accessible to women from different ethnic and cultural backgrounds. Additional studies are needed to address these questions, ideally using a randomized controlled study design. Nevertheless, this study suggests that women's crisis houses may be a less institutional and less stigmatizing alternative to traditional psychiatric admission for women who need admission but who do not require intensive observation or supervision and who are not at risk of violence or in need of detoxification. At present, however, there is a scarcity of such facilities internationally ( 14 ).
Conclusions
Little is known about the effectiveness of women's crisis houses, but this study found few clinical or sociodemographic differences between women voluntarily admitted to traditional psychiatric facilities and women admitted to women's crisis houses. The findings suggest that women's crisis houses are a viable alternative to traditional psychiatric hospitals for women with severe mental illnesses who do not require intensive observation or supervision.
Acknowledgments and disclosures
This study was funded by grant G0401241 from the U.K. Medical Research Council. The authors acknowledge the assistance of the Mental Health Research Network of the National Institute for Health Research. The authors thank all the clinicians who provided data for this study.
The authors report no competing interests.
1. Mainstreaming Gender and Women's Mental Health: Implementation Guidance. London, Department of Health, 2003Google Scholar
2. Killaspy H, Dalton J, McNicholas S, et al: Drayton Park, an alternative to hospital admission for women in acute mental health crisis. Psychiatric Bulletin 24:101–104, 2000Google Scholar
3. Meiser-Stedman C, Howard L, Cutting P: Evaluating the effectiveness of a women's crisis house: a prospective observational study. Psychiatric Bulletin 30:324–326, 2006Google Scholar
4. Johnson S, Bingham C, Billings J, et al: Women's experiences of admission to a crisis house and to acute hospital wards: a qualitative study. Journal of Mental Health 13:247–262, 2004Google Scholar
5. Hodgson R, Carr D, Weallean L: Brunswick House: a weekend crisis house in North Staffordshire. Psychiatric Bulletin 26:453–455, 2002Google Scholar
6. Fenton WS, Mosher LR, Herrel JM, et al: Randomized trial of general hospital and residential alternative care for patients with severe and persistent mental illness. American Journal of Psychiatry 155:516–522, 1998Google Scholar
7. Rogler LH, Cortes DE: Help-seeking pathways: a unifying concept in mental health care. American Journal of Psychiatry 150: 554–561, 1993Google Scholar
8. Gater R, De Almeida E, Sousa B, et al: The pathways to psychiatric care: a cross-cultural study. Psychological Medicine 21:761–774, 1991Google Scholar
9. Slade M, Powell R, Rosen A, et al: Threshold Assessment Grid (TAG): the development of a valid and brief scale to assess the severity of mental illness. Social Psychiatry and Psychiatric Epidemiology 35:78–85, 2000Google Scholar
10. Slade M, Cahill S, Kelsey W, et al: Threshold 2: the reliability, validity and sensitivity to change of the Threshold Assessment Grid (TAG). Acta Psychiatrica Scandinavica 106:453–460, 2007Google Scholar
11. Bebbington PE, Feeney ST, Flannigan CB, et al: Inner London collaborative audit of admissions in two health districts: II. ethnicity and the use of the Mental Health Act. British Journal of Psychiatry 165:743–749,759, 1994Google Scholar
12. Morgan C, Mallett R, Hutchinson G, et al: Pathways to care and ethnicity: 1. sample characteristics and compulsory admission: report from the AESOP study. British Journal of Psychiatry 186:281–289, 2005Google Scholar
13. Cotton MA, Johnson S, Bindman J, et al: An investigation of factors associated with psychiatric hospital admission despite the presence of crisis resolution teams. BMC Psychiatry 7:52, 2007Google Scholar
14. Leff J, Warner R: Social Inclusion of People With Mental Illness. Cambridge, United Kingdom, Cambridge University Press, 2006Google Scholar



