Racial Differences in Medication Switching and Concomitant Prescriptions in the Treatment of Bipolar Disorder
The use of multiple medicines in the treatment of a disease is referred to as polypharmacy. Often the term has a negative connotation because it can suggest indiscriminate, unscientific, or excessive prescribing. However, for bipolar disorder, a chronic and intermittent illness that requires accurate diagnosis and skillful management, administration of several psychiatric drugs concurrently may result in a more rapid onset of relief or intensification of therapeutic effectiveness at the start of treatment ( 1 ).
Considerable variations in prescribing practices have already been documented for patients with bipolar disorder. Patients with bipolar disease who are from minority groups are less likely to receive innovative treatment or higher-cost innovations ( 2 ). In particular, black patients are less likely than white patients to receive second-generation antipsychotic medication ( 2 ). Although the defining characteristic of second-generation antipsychotic medications is efficacy with a significantly lower risk of side effects, none of the second-generation neuroleptics have a perfect side effect profile ( 3 , 4 , 5 ).
This study examined the treatment of bipolar disorder in common practice on the basis of retrospective analysis of data from a large database. It also assessed the association between race and differences in medication use and outcomes.
Methods
Design and patient selection
Data for patients with bipolar disorder obtained from the Henry Ford Health System (HFHS) were examined by using a retrospective cohort design. The database is vertically integrated and contains data on more than 540,000 covered persons. Care provided each year by HFHS includes more than 2.5 million patient contacts, 20,000 ambulatory surgeries, and 65,000 hospital admissions. Most of the care is provided under a system-affiliated, salaried physician group. It is one of the nation's largest group practices, with nearly 900 physicians in more than 40 specialties.
The study population was identified from the subset of patients with insurance coverage under the health system's mixed-model managed care plan; these patients have access to the HFHS provider network and may also have contacts with other provider networks. For patients who reach Medicare age, the health system offers both traditional Medicare (Medicare Complementary) and its own HFHS Medicare product (Medicare Risk).
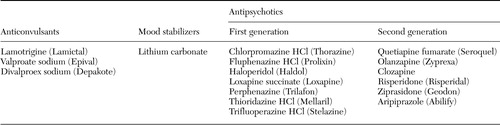
The study population consisted of all patients 19 years of age and older who met four criteria: an ICD-9 ( 6 ) diagnosis of bipolar disorder (codes 296.0x-296.1x and 296.4x-296.7x); at least one prescription for anticonvulsants, mood stabilizers, first-generation antipsychotics, or second-generation antipsychotics between January 1998 and March 2004 ( Table 1 ); one year of continuous enrollment in the managed care plan before the index date (that is, the date the patient was first prescribed one of the medications of interest); and one year of continuous follow-up after the index date. Patients were followed from one year before the index date to one year after. Analyses were conducted for the study population overall and stratified by race (black versus nonblack). Demographic variables, such as race, were provided by patient self-report and obtained from the HFHS database.
 |
Descriptive statistics
Age, gender, and insurance coverage were categorized, and differences were assessed using t tests for continuous measures and chi square tests for categorical measures.
Comorbid conditions
Comorbid conditions thought to influence therapy selection, mortality, or financial charges were determined a priori on the basis of a literature review and consultation with physicians. Baseline comorbid conditions were identified on the basis of the presence of at least two ICD-9 codes before the index date (the codes are available from the authors on request).
Pharmacotherapy, switching, and concomitant prescriptions
Four categories of psychotropic medications—anticonvulsants, mood stabilizers, first-generation antipsychotics, and second-generation antipsychotics—prescribed at the index date were identified by their generic names by using National Drug Codes ( 7 ). The number of changes in psychotropic drug classes was determined—that is, switches from one class to another or the additional prescription of a drug from a different class. Multiclass switching was the sequential prescription of at least two medications from different classes rather than only one medication (with or without a prescription overlapping period). Concomitant prescription was the prescription of at least two medications from different classes at the same time (versus only one) or the prescription of at least two second-generation antipsychotic medications (versus one or none) either at the same time or sequentially. Patients who received multiple medications of the same class were not considered to have multiclass switching or concomitant prescriptions.
Adverse effects of pharmacotherapy
Potential adverse effects of pharmacotherapy examined in the study were determined a priori from a literature review and physicians' opinions. Specified adverse effects were identified by the presence in the database of ICD-9 codes, laboratory values, or a prescription for benztropine (Cogentin) during follow-up.
Outcomes, resource utilization, and charges
Outcomes and resource utilization were examined from the index prescription date over a one-year follow-up period. Charges were examined for the year before and the year after the index date. Emergency department visits or hospitalizations were analyzed individually and as a composite measure (either an emergency department visit or a hospitalization). The mean total cost per patient for all health care—including physical and mental health—was considered.
Multivariate logistic modeling
Logistic regression models determined the relationship between outcomes and multiclass switching or concomitant prescriptions while adjusting for covariates. The odds of having an emergency department visit or hospitalization were calculated for patients with multiclass switching or concomitant prescriptions in relation to patients without multiclass switching or concomitant prescriptions.
Two multivariate models were created that adjusted for all potential covariates. One model included all patients and used the main predictor of two or more psychotropic medications (versus only one). The second model included all patients and used the main predictor of two or more second-generation antipsychotics (versus none or one). On the basis of a priori specifications, covariates with p values less than .2 were retained in the final models.
Results
Descriptive statistics
As shown in Table 2 , the study population consisted of 1,113 patients. The mean age was 44.3 years, and 60.7 percent of patients were female. In terms of race or ethnicity, 326 (29.3 percent) were black, 759 (68.2 percent) were white, and 28 (2.5 percent) were categorized as "other." Because of the small size of the "other" category, patients who were not black were grouped into one category (787 nonblack patients, or 70.7 percent)
 |
As shown in Table 2 , black patients were significantly more likely than nonblack patients to be female (70.9 percent compared with 56.4 percent; χ 2 =20.1, df=1, p<.001). The groups did not differ significantly in age. Overall, the two groups differed significantly in health care coverage (χ 2 =14.4, df=4, p=.006); a larger proportion of black patients were covered by Medicaid (8.3 compared with 5.3 percent) and Medicare Complementary (12.3 compared with 8.9 percent); a smaller proportion of black patients were covered by Medicare Risk (6.1 compared with 11.8 percent).
Comorbid conditions
Axis I psychiatric disorders were the most commonly encountered comorbid conditions overall (947 patients, or 85.1 percent). Patients had cardiovascular conditions (365 patients, or 32.8 percent), substance use disorders (150 patients, or 13.5 percent), neurologic impairments (135 patients, or 12.1 percent), diabetes mellitus (100 patients, or 9.0 percent), and thyroid dysfunction (86 patients, or 7.7 percent). Compared with nonblack patients, a significantly larger proportion of black patients had a comorbid diagnosis of axis I psychiatric disorders (288 patients, or 88.3 percent, compared with 659 patients or 83.7 percent; χ 2 =3.9, df=1, p=.050). No significant differences were found between the two groups for other comorbid conditions.
Pharmacotherapy, switching, and concomitant prescriptions
The most common psychotropic medication prescribed at the index date was anticonvulsants (471 patients, or 42.3 percent). Anticonvulsants were followed by second-generation antipsychotics (388 patients, or 34.9 percent), mood stabilizers (256 patients, or 23 percent), and first-generation antipsychotics (106 patients, or 9.5 percent). At the index date 108 patients (9.7 percent) received at least two medications from different drug classes simultaneously. More than one-third of all patients (407 patients, or 36.6 percent) received at least two medications from different drug classes simultaneously during the follow-up period.
For most patients, no multiclass switch occurred (793 patients, or 71.2 percent), whereas 238 (21.4 percent) had one such switch, and 83 (7.2 percent) had multiple such switches. Of those who had any change in drug classes, 102 (31.8 percent) experienced a sequential switch from one class to another, and for 251 (78.2 percent) a medication from another class was added on to their previous medication and they received two or more medications simultaneously. For patients with any drug change, the mean time to the first change was 113.7±110 days; the mean time to the first drug switch was 186.4±105.3 days, and the mean time to the first drug add-on was 95.2±102.7 days. The mean number of medications from the four classes prescribed per patient was 1.52±.81, and the mean number of prescriptions per patient was 9.74±7.42 over the one-year follow-up.
Nearly half of the black patients (159 patients, or 48.8 percent) were given a prescription for a second-generation antipsychotic at index compared with less than a third of the nonblack patients (229 patients, or 29.1 percent) (χ 2 =39.3, df=1, p<.001). In contrast, 215 of the nonblack patients (27.3 percent) received mood stabilizers compared with 41 of the black patients (12.6 percent) (χ 2 =28.3, df=1, p<.001). The proportions of patients who received anticonvulsants and first-generation antipsychotics did not differ by race.
Among black patients, 41 (12.6 percent) received two or more psychotropic medications simultaneously at the index date compared with only 67 (8.5 percent) of nonblack patients (χ 2 =4.3, df=1, p=.037). A total of 134 black patients (41.1 percent) received two or more psychotropic medications at any time compared with only 273 nonblack patients (34.7 percent) (p=.043). The number of patients who received two or more second-generation medications at any time did not differ by race. The number of drug changes, time to first change, and the number of different drugs a patient received also did not differ by race.
Adverse effects of pharmacotherapy
Baseline laboratory values before psychotropic treatment for patients with laboratory data available are shown in Table 2 . According to the computerized database, most patients did not experience a symptomatic adverse event during follow-up. The most common events were abnormal cholesterol levels (101 patients, or 9.1 percent) and abnormal triglyceride levels (43 patients, or 3.9 percent). Among black patients, 24 (7.4 percent) had abnormal cholesterol levels and seven (2.2 percent) had abnormal triglyceride levels. Among nonblack patients, the proportions of patients with abnormal values were slightly larger (for cholesterol, 77 patients, or 9.8 percent; for triglycerides, 36 patients, or 4.6 percent), but the differences between the two groups were not significant. Other adverse events included tardive dyskinesia, hypotension, seizures, dysphagia, suicide attempts, weight gain, cataracts, hypothyroidism, transaminase elevations, and extrapyramidal symptoms, but none varied by race.
Outcomes, resource use, and charges
Overall, 231 patients (20.8 percent) were hospitalized, and 371 (33.3 percent) had an emergency department visit during the first year of follow-up; 492 patients (44.2 percent) had at least one emergency department visit or hospitalization. Of those patients with a hospitalization, the mean length of stay was 8.1±10.8 days. The mean total cost in the year after the index date was $11,836±$17,222 per patient.
A larger proportion of black patients had an emergency department visit or hospitalization after the index date; 86 black patients (26.4 percent) were hospitalized compared with 145 nonblack patients (18.4 percent) (χ 2 =8.9, df=1, p=.003). A total of 132 black patients (40.5 percent) had an emergency department visit compared with 239 nonblack patients (30.4 percent) (χ 2 =10.6, df=1, p=.001). Black patients with a hospitalization had a mean length of stay of 7.6±7.8 days compared with 8.4±12.2 days among nonblack hospitalized patients, but the difference was not significant. Compared with nonblack patients, black patients were more likely to be hospitalized or to have an emergency department visit during follow-up (319 nonblack patients, or 40.5 percent, compared with 173 black patients, or 53.1 percent; χ 2 =14.7, df=1, p<.001). The mean total health care costs in the year after the index date did not differ by race.
Multivariate logistic modeling
Table 3 presents the two multivariate models. Patients who received two or more of the medications of interest during follow-up were significantly more likely to have an emergency department visit or hospitalization than patients who received one medication, after the analyses adjusted for covariates. Race was a significant covariate in this model; black patients were significantly more likely to have a hospitalization or emergency department visit than nonblack patients. As Table 3 shows, having a comorbid substance use disorder or a comorbid cardiovascular condition also significantly increased the odds of a hospitalization or emergency department visit.
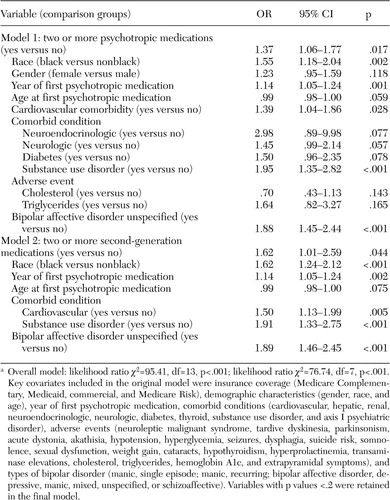 |
a Overall model: likelihood ratio χ 2 =95.41, df=13, p<.001; likelihood ratio χ 2 =76.74, df=7, p<.001. Key covariates included in the original model were insurance coverage (Medicare Complementary, Medicaid, commercial, and Medicare Risk), demographic characteristics (gender, race, and age), year of first psychotropic medication, comorbid conditions (cardiovascular, hepatic, renal, neuroendocrinologic, neurologic, diabetes, thyroid, substance use disorder, and axis I psychiatric disorder), adverse events (neuroleptic malignant syndrome, tardive dyskinesia, parkinsonism, acute dystonia, akathisia, hypotension, hyperglycemia, seizures, dysphagia, suicide risk, somnolence, sexual dysfunction, weight gain, cataracts, hypothyroidism, hyperprolactinemia, transaminase elevations, cholesterol, triglycerides, hemoglobin A1c, and extrapyramidal symptoms), and types of bipolar disorder (manic, single episode; manic, recurring; bipolar affective disorder, depressive, manic, mixed, unspecified, or schizoaffective). Variables with p values <.2 were retained in the final model.
Patients who received two or more second-generation antipsychotics were significantly more likely to have an emergency department visit or hospitalization than patients who had one second-generation antipsychotic or no second-generation antipsychotics, after the analyses adjusted for covariates. Black patients in this group were more likely to have a hospitalization or emergency department visit than nonblack patients. Having a comorbid substance use disorder or a comorbid cardiovascular disorder significantly increased the odds of a hospitalization or emergency department visit.
Discussion
This study examined the treatment of bipolar disorder in usual practice through analysis of a large patient claims database. The purpose was to determine whether treatment of bipolar disorder in a real-world setting involved combinations of psychotropic medications that differed between subpopulations and even individual patients, as previous studies have indicated. In addition, this study evaluated the differences in medication use and outcomes among racial groups. The findings, notably those related to differences in treatment patterns among black patients, have not been demonstrated in previous studies.
Few studies have documented the use of multiclass switching or concomitant prescriptions in the treatment of bipolar disorder and its effect on resource utilization. Our analysis supported previous findings of an increased prevalence of multiclass switching or concomitant prescriptions. More than one-third of patients received multiple medications. However, patients who received at least two psychotropic medications were significantly more likely to be hospitalized or to have an emergency department visit than patients who received one psychotropic medication, even after the analysis adjusted for covariates. Similar results were found when the sample was stratified by race. These findings suggest that there may be a need for a more comprehensive assessment of multiclass switching and concomitant prescriptions and the associated risks and benefits for patients with bipolar disorder. The findings also suggest that multiclass switching and concomitant prescriptions are more likely to be found among patients with more severe illness, who are also more likely to be at increased risk of an emergency department visit or a hospitalization.
Studies have consistently shown that members of racial and ethnic minority groups use medical care at a lower rate than whites and have poorer access ( 8 ). Lower socioeconomic status and lower rates of health insurance coverage among blacks and Hispanics often lead to disparities in health care. Unfortunately, racial and ethnic differences in health care persist even among those with health insurance coverage and when other socioeconomic characteristics are controlled for ( 9 ). In a cross-sectional nationally representative survey of households, Hargraves and colleagues ( 8 ) found that blacks in general were less likely to have a regular provider and were more likely to use emergency departments for medical care. These findings are consistent with those of the study reported here, which indicate that black patients are more likely than nonblack patients to receive prescriptions for medications from an emergency department physician. Emergency care is both the most costly and the least effective method of treating the types of chronic problems that claim the greatest number of lives each year ( 10 ). Furthermore, patients who use the emergency department as their primary source of care often do not develop relationships with primary care physicians, hindering their access to adequate preventive care or the continuity of care that is necessary for a chronic psychiatric illness such as bipolar disorder.
Sociodemographic characteristics, such as socioeconomic status, sex, age, marital status, and race or ethnicity, have also been reported to be predictors of psychiatric disorders. Previous studies have found increased rates of certain psychiatric disorders among individuals with low socioeconomic status, among women, and among patients from minority racial or ethnic groups ( 11 ). The study reported here had similar findings: black patients were more likely than nonblack patients to be given a diagnosis of an axis I psychiatric disorder and were more likely to be female and enrolled in Medicaid. These results may be attributable to the effects of increased psychosocial stress associated with the circumstance of poverty and to a synergistic relationship between limited education and decreased opportunities for employment ( 12 ).
Racial and ethnic variations in pharmacotherapy have been documented in recent studies, indicating that blacks may be less likely than whites to receive second-generation antipsychotic medications or selective serotonin reuptake inhibitors ( 13 ). In the study reported here, the occurrence of detectable adverse effects did not differ between black and nonblack patients. However, Herbeck ( 14 ) noted that blacks tended to receive medications that are not first-line recommendations and that have a greater risk of producing tardive dyskinesia and extrapyramidal side effects. As a result, black patients could be expected to suffer diminished clinical status. This treatment disparity may also contribute to lower compliance rates among black patients as well as more frequent emergency department visits and psychiatric hospitalizations ( 14 ), which would explain the higher health care resource use seen for black patients in this study. Multiclass switching and concomitant prescriptions were more prevalent among black patients; however, the number of psychotropic prescriptions per person was lower.
Poorer treatment compliance may help explain the observed associations between race and outcomes—that is, emergency department visits and hospitalizations. The variations in treatment regimens, compliance, and outcomes could also be explained by physicians' skills, knowledge, and treatment preferences; metabolic differences between racial or ethnic groups; and economic and health system factors ( 14 ). These issues raise concerns about the adequacy of care that is provided to patients with bipolar disorder, especially for a disease that requires monitoring on a regular basis.
Contrary to previous studies, this study showed that black patients were significantly more likely to receive second-generation antipsychotics and less likely to receive mood stabilizers. Black patients may have more severe disease, and when the disease is properly diagnosed they might be more likely to be given second-generation antipsychotics. It has also been stated that black patients metabolize antipsychotics more slowly, resulting in a faster and higher response rate to the medication than white patients ( 15 ). Antipsychotic metabolism is a complex process, and considerable controversy surrounds this issue ( 16 , 17 ). However, if black patients do metabolize antipsychotics more slowly, the greater resource use for black patients may also be attributable to the increase in prescriptions of second-generation antipsychotics, because a slow metabolic rate may increase the incidence of side effects ( 15 ).
This study had a number of limitations. Retrospective data often lack clinical details that can be helpful in studies of treatment and outcomes in bipolar disorder. For example, it is not possible to precisely identify an existing condition by reviewing clinical notes or charts; therefore, ICD-9 codes are the most robust option for determining the presence of various diagnoses. In addition, no information was available on the decision-making process or the intent of clinicians, which may play a crucial role in multiclass switching and concomitant prescriptions and in discrepancies in treatment by race. As with any retrospective analysis, associations can be demonstrated, but causality cannot be conclusively determined. Therefore, although patients who received two or more psychotropic medications were more likely to be hospitalized, the two factors may not be causally linked. Instead, it is possible that the sicker, more treatment-resistant patients—that is, those who are more likely to seek hospital treatment—are also more likely to require treatment with multiple medications.
Similarly, this study did not control for the severity of a patient's illness, so it is possible that multiclass switching and concomitant prescriptions are associated with greater severity of illness, which may explain the increased negative outcomes. Also, it may not be race per se but a behavior or factor that is more prevalent within certain racial or ethnic groups that accounts for the association with negative outcomes. This study was also unable to fully distinguish race from socioeconomic status because of the limited availability of information (only information on race is included in the database). To fully understand how multiclass switching and concomitant prescriptions are related to outcomes, future research in the form of a randomized, prospective, head-to-head trial that controls for the severity of illness at baseline is required. Nonetheless, database studies allow for analysis of large patient populations over lengthy periods, permitting assessment of population health and economic trends.
Conclusions
This study demonstrated that switching between different classes of psychotropic medications and concomitant prescription of medications are common in the treatment of patients with bipolar disorder. These trends were found for black and nonblack patients. In addition, use of second-generation antipsychotics was higher among black patients. Black patients tended to have a higher rate of resource use than white patients, which was probably a result of both racial and socioeconomic differences. This study demonstrates the need for further exploration of the effects of multiclass switching, concomitant prescriptions, and use of second-generation antipsychotics on patient populations and the importance of establishing treatment guidelines for bipolar disorder.
Acknowledgment
This study was funded by AstraZeneca, LP.
1. Thase ME, Bhargava M, Sachs GS: Treatment of bipolar depression: current status, continued challenges, and the STEP-BD approach. Psychiatric Clinics of North America 26:495-518, 2003Google Scholar
2. Daumit GL, Crum RM, Guallar E, et al: Outpatient prescriptions for atypical antipsychotics for African Americans, Hispanics, and whites in the United States. Archives of General Psychiatry 60:121-128, 2003Google Scholar
3. Rajiv T, Jibson MD: Extrapyramidal side effects of antipsychotic treatment: scope of problem and impact on outcome. Annals of Clinical Psychiatry 14:123-129, 2002Google Scholar
4. Hamner M: The effects of atypical antipsychotics on serum prolactin levels. Annals of Clinical Psychiatry 14:163-173, 2002Google Scholar
5. Antai-Otong D: Metabolic effects associated with atypical antipsychotic medications. Perspectives in Psychiatric Care 40:70-73, 2004Google Scholar
6. International Classification of Diseases, 9th Rev, Clinical Modification. Los Angeles, Practice Management Information Corp, 2003Google Scholar
7. Redbook for Windows. Greenwood Village, Colo, Thompson Micromedex, 2004Google Scholar
8. Hargraves JL, Cunningham PJ, Hughes RG: Racial and ethnic differences in access to medical care in managed care plans. Health Service Research 36:853-868, 2001Google Scholar
9. Shi L: Vulnerable populations and health insurance. Medical Care Research Review. 57:110-134, 2000Google Scholar
10. Connolly C: Some finding no room at the ER: screening out non-urgent cases stirs controversy. Washington Post, Apr 26, 2004, p A1Google Scholar
11. Taylor RR, Jason LA, Jahn SC: Chronic fatigue and sociodemographic characteristics as predictors of psychiatric disorders in a community-based sample. Psychosomatic Medicine 65:896-901, 2003Google Scholar
12. Williams DR, Takeuchi DT, Adair RK: Marital status and psychiatric disorders among blacks and whites. Journal of Health and Social Behavior. 33:140-157, 1992Google Scholar
13. Wang PS, West JC, Tanielian T, et al: Recent patterns and predictors of antipsychotic medication regimens used to treat schizophrenia and other psychotic disorders. Schizophrenia Bulletin 26:451-457, 2000Google Scholar
14. Herbeck DM, West JC, Ruditis I, et al: Variations in use of second-generation antipsychotic medication by race among adult psychiatric patients. Psychiatric Services 55:677-684, 2004Google Scholar
15. Lawson WB: Racial and ethnic factors in psychiatric research. Hospital and Community Psychiatry. 37:50-54, 1986Google Scholar
16. Frackiewicz EJ, Sramek JJ, Herrera JM, et al: Ethnicity and antipsychotic response. Annals of Pharmacotherapy 31:1360-1369, 1997Google Scholar
17. Emsley RA, Roberts MC, Rataemane S, et al: Ethnicity and treatment response in schizophrenia: a comparison of 3 ethnic groups. Journal of Clinical Psychiatry 63:9-14, 2002Google Scholar



