Impact of Family Burden and Affective Response on Clinical Outcome Among Patients With Bipolar Disorder
Abstract
OBJECTIVE: This study evaluated the direct and indirect effects of family burden and affective response on medication adherence and outcome among patients with bipolar disorder. METHODS: Data were examined for 126 patients who were consecutively admitted to the psychiatric service at a university-affiliated hospital and who met research diagnostic criteria for bipolar I or II disorder or for schizoaffective disorder, manic type, and their family caregivers. A total of 101 pairs of patients and family caregivers (80 percent) completed 15 months of study and were included in the analyses. Patients and their identified caregivers were assessed within two weeks of either discharge from the index inpatient admission or initiation of outpatient treatment (baseline assessment). Patients and caregivers were also assessed seven and 15 months after the baseline assessment. Structural equation modeling was used to evaluate caregivers' influences on patients' medication adherence seven months after baseline and on clinical outcome 15 months after baseline. RESULTS: The indexes of overall fit for the path model confirmed the a priori measurement model. Significant paths were found from the caregiver's perceived burden at baseline to the caregiver's emotional overinvolvement at baseline, from the caregiver's emotional overinvolvement at baseline to the patient's medication adherence at the seven month follow-up, and from the patient's medication adherence at the seven-month follow-up to the patient's outcome at the 15-month follow-up. The paths from the caregiver's perceived burden at baseline to the patient's medication adherence seven months after baseline and the patient's outcome 15 months after baseline were not significant. CONCLUSIONS: When caregivers of patients with bipolar illness experience a high burden, patient outcome is adversely affected. This relationship is mediated through families' affective response and patients' medication adherence.
The term family or caregiver burden commonly refers to the effects of the mental illness of one family member on the emotional well-being of other family members, as well as on the family members' use of time, finances, and general living conditions (1). Although most studies of burden have focused solely on the challenges to families of caring for a mentally ill relative, research in schizophrenia has suggested that families' experiences of burden may have adverse repercussions for persons with the illness (2,3). A naturalistic, prospective study by Perlick and colleagues (4) recently demonstrated that patients with bipolar disorder were more likely to meet criteria for a major affective episode at the 15-month follow-up when their families reported higher levels of burden during the patients' acute episode at baseline. This finding remained significant when the analysis controlled for the baseline symptom level. In this study we applied structural equation modeling to data from a subsample of this study cohort to evaluate an exploratory model identifying the mediating mechanism through which families' experiences of burden might impede the recovery of their relatives with bipolar illness.
Methods
Sample
The sample for our study consisted of the first 126 patients and 126 caregivers enrolled in a study of family experience and outcome in bipolar disorder (4,5). This sample was chosen for our study because only this cohort had been evaluated on a measure of caregiver affective response, the Camberwell Family Interview (CFI) (6), which was administered only during the first nine months of the study. These patients were admitted for treatment of bipolar disorder to a psychiatric inpatient or outpatient service in a private hospital that is affiliated with a medical college, and they were selected in order of consecutive admission on the basis of eligibility criteria: a lifetime diagnosis of bipolar depression with mania (bipolar I) or with hypomania (bipolar II) or schizoaffective disorder, manic type, by research diagnostic criteria (7), as evaluated by using the Schedule for Affective Disorders-Lifetime Version (SADS-L) interview (8); availability of a qualifying caregiver for the study; age of 16 years or older; and being judged able to participate by their primary clinician. On the basis of the method established by Pollak and Perlick (9), the primary caregiver was defined as the family member, friend, or significant other who satisfied the greatest number (and at least three) of five criteria: is a spouse, parent, or spouse equivalent; has the most frequent contact with the patient; helps to support the patient financially; has been the most frequent collateral participant in the patient's treatment; and is the person contacted by treatment staff in case of emergency. We obtained approval from the institutional review board of the Yale Human Investigations Committee and informed consent from participants.
Participants were enrolled between October 1993 and September 1995, and follow-up data were collected for 15 months, through December 1996. Eighty percent (N=101) of the 126 pairs of patients and caregivers completed 15 months of the study and were included in our analysis. A comparison of the 101 pairs of patients and caregivers who completed 15 months of the study with the 25 pairs who did not complete the study showed no significant differences on any of the 14 sociodemographic and clinical variables examined. A comparison of the 101 pairs who completed our study with the 138 pairs who were enrolled in the second cohort of the study of family experience and outcome in bipolar disorder, but who were not enrolled in our study, demonstrated that the patients in our study were more frequently outpatients at baseline (χ2 with continuity correction=5.84, df=1, p=.016) and that their caregivers were more frequently parents or other, nonspousal relatives than spouses of the patient (χ2 with continuity correction=3.84, df=1, p=.05).
Data collection
Patients and their identified caregivers were assessed within two weeks of either discharge from the index inpatient admission or initiation of outpatient treatment (baseline assessment). Patients and caregivers were also assessed seven and 15 months after the baseline assessment. Patients and caregivers were assessed by independent interviewers who were blind to the results that were obtained from the other participant in the pair. Interviewers had demonstrated reliability on the research instruments described below.
Rationale for exploratory model
The exploratory model is based on the stress model that was developed by Lazarus and Folkman (10) and on previous research and clinical observation. In our model, family burden during an acute episode was hypothesized to influence clinical outcome, both directly and indirectly, through the family's affective response toward the patient, as represented by expressed emotion (6). Because studies have consistently demonstrated that higher levels of expressed emotion predict relapse among patients who have either affective illness or schizophrenia (11,12) and have found that expressed emotion and its components are positively correlated with measures of family burden (13,14), we examined the relationship of these two constructs in relation to patient outcome. Consistent with the stress and coping theory (10), which suggests that cognitive and affective evaluation of the degree of threat posed by the stressor precedes the individual's response, we placed family burden ratings, which consist of both a cognitive and an affective appraisal of the degree of problems posed by the patient's illness (15), antecedent to expressed emotion scores, which reflect the family's behavior toward the patient (6). Because some studies have shown differential associations of the main expressed emotion components—critical comments and emotional overinvolvement—with burden (13), we represented these dimensions separately in our model. However, we hypothesized that higher levels of burden would be associated with higher levels of both critical comments and emotional overinvolvement.
We included an evaluation of medication adherence at baseline and at the seven-month follow-up in our model because adequate pharmacotherapy is an important predictor of clinical outcome among patients with bipolar disorder (16,17,18,19). Because clinical observation suggests that medication adherence is a frequent object of disagreement between patient and family, we hypothesized that burden, critical comments, and emotional overinvolvement would affect clinical outcome both directly and indirectly through an effect on medication adherence. Specifically we hypothesized that higher levels of burden would be associated with higher levels of both critical comments and emotional overinvolvement.
Finally, we included as covariates variables that previous studies have found to predict burden (symptom severity, whether the patient lives with the caregiver, and caregiver stigma) (4,5,20,21,22) or critical comments and emotional overinvolvement (the caregiver's relationship to the patient) (23). However, we did not hypothesize direct effects of these variables on clinical outcome because we did not believe that these variables would have a direct effect on outcome. Higher levels of symptom severity and caregiver stigma as well as living with the patient and being a spouse were hypothesized to be related to higher levels of burden, critical comments, or emotional overinvolvement. Clinical outcome was indexed by whether or not the patient met diagnostic criteria for a current affective episode of either pole at the 15-month follow-up point. Because our study was exploratory and had a limited sample size, we did not include all possible paths but selected those with primary theoretical relevance or previous research associations.
Measures
Burden. The Social Behavior Assessment Scale (SBAS) (1), a semistructured interview for caregivers, was used to evaluate the caregiver's experience of objective and subjective burden in three domains that covered the patient's problem behaviors (for example, violence and unpredictability), the patient's social role dysfunction, and the impact of the illness on caregivers' work, social, and leisure time. The SBAS was given at baseline and measured caregivers' experience of burden for the previous seven months. To measure objective burden, caregivers were asked to rate the degree to which each of 56 problems was present on a 3-point scale ranging from 0, none, to 2, severe. To measure subjective burden caregivers rated the degree of distress that they experienced in relation to each item that they had rated as objectively present, using the same scale. Because the intercorrelation between the two scales was very high (Pearson's r=.76), they were combined into a single scale, which demonstrated adequate internal consistency (Cronbach's alpha=.82).
Expressed emotion. The CFI is a semistructured interview that pertains to the caregiver's experience of the patient's illness, which assesses expressed emotion (6). The CFI was administered to the caregiver during the index inpatient admission, within two weeks of discharge (for inpatients), or within two weeks of the initial evaluation (for outpatients). Interviews were audiotaped and coded by raters who had completed the standard expressed emotion training with a minimum reliability of .80 (intraclass correlation) with a criterion rater. Interrater reliability between the two raters was evaluated on a subset of 17 audiotapes and yielded intraclass correlation coefficients of .82 for critical comments and .68 for emotional overinvolvement. Because emotional overinvolvement ratings were negatively skewed, possibly reflecting the lower proportion of parent caregivers who were studied relative to studies of schizophrenia, we recalculated interrater reliability for emotional overinvolvement by using Finn's r, a method applicable when skewed distributions of ratings and associated reductions in variance can deflate the coefficient even when agreement between raters is relatively high (24,25). The coefficient that was found by using this method for two raters was .81.
Medication adherence. The Treatment and Medication Compliance Data Sheet (TMCDS) (26), an anchored, 6-point Likert-type scale, was administered to both caregivers and patients at baseline and the seven-month follow-up to assess patient adherence with the prescribed medication regimen. Responses ranged from 6, excellent compliance: "Takes all medicine as prescribed at essential times," to 1, noncompliance: "Has not taken any of prescribed medicines since discharge from hospital." Agreement between two independent raters on the patient version of this scale for a subsample of 25 was .87 (Pearson's r). Because agreement between the caregiver and patient ratings was good (Pearson's r=.83), the mean of the caregiver and patient ratings of medication compliance was used as the measure of medication compliance in the analyses below (Cronbach's alpha=.85).
Patient outcome. The SADS-L determined whether or not the patient met criteria for a major episode of affective illness of either pole. The questions on the Schedule for Affective Disorders and Schizophrenia- Lifetime Version (SADS-L) (8) pertaining to affective illness were modified to include all symptoms that occurred during the three-month period before the 15-month follow-up. The three-month time frame was chosen to maximize the likelihood of identifying recent but transitory episodes of illness, while defining a time interval that was relatively current (4).
Covariates. The 24-item version of the Brief Psychiatric Rating Scale (BPRS) (27) was used to rate the severity of patients' affective and psychotic symptoms at baseline. The measure used a 7-point scale, ranging from 1, none, to 7, severe. To check reliability, an intraclass correlation coefficient was calculated for the four trained raters, based on two videotaped interviews, by using all 24 scales. Coefficients were .96, .85, .82, and .83 for the first tape and .9, 1, .87, and .88 for the second tape. Caregivers' perceptions of stigma at baseline were evaluated by using a 15-item scale described by Struening and colleagues (22); the scale demonstrated good internal consistency in our study (Cronbach's alpha=.83). Higher values reflect a greater perception of stigma toward consumers and their families. To evaluate the effect of residing in the same household as the patient, caregivers who did so were coded as 1 on this variable, and those living apart from the patient were coded as 0.
Statistical analysis
Structural equation modeling was used to evaluate the hypothesized direct and indirect effects of the specific measures of caregiver burden and affective response on patient treatment adherence at seven months and on patient clinical outcome at 15 months. The statistical methods employed were consistent with those described in established texts (28,29,30,31) and were implemented in SAS by using PRO CALIS (32). The overall model fit was assessed by its model chi square, its goodness of fit index adjusted for degrees of freedom (AGFI), and its root mean square error of approximation (RMSEA). T statistics were used to assess the significance of individual path coefficients. Five measures were specified as exogenous variables: baseline caregiver stigma, patient symptom level (BPRS), medication adherence, whether the caregiver lived with the patient, and caregiver's relation to the patient (spouse versus others) Five additional variables were specified as endogenous variables: baseline caregiver burden, criticism and emotional overinvolvement, seven-month medication adherence, and 15-month affective episode status.
Results
Sample characteristics
The characteristics of the patients and their caregivers are presented in Table 1.
Structural equation model
Results associated with our path model are presented in Figure 1. The indexes of overall model fit were excellent (χ2=8.03, df=17, p=.97; AGFI= .95; RMSEA<.01), indicating that our model provided a reasonable fit to the observed data.
Figure 1 indicates that caregiver burden at baseline did not have a direct effect on clinical outcome at the 15-month follow-up. Instead, the effects of burden on the clinical outcome were mediated by caregivers' emotional overinvolvement at baseline and medication adherence at the seven-month follow-up. Similarly, caregivers' emotional overinvolvement at baseline did not have a direct relationship to the clinical outcome at the 15-month follow-up. Instead, the effects of emotional overinvolvement on clinical outcome were mediated by medication adherence. Mediating variables were found to be associated with clinical outcome in the predicted directions. Caregivers who reported higher levels of burden had significantly higher levels of emotional overinvolvement. Higher levels of emotional overinvolvement at baseline were related to lower levels of medication adherence at the seven-month follow-up, and poorer medication adherence was associated with a greater risk of sustaining a major affective episode at the 15-month follow-up. By contrast, the baseline level of caregiver critical comments—the other parameter of expressed emotion evaluated—did not significantly mediate the effects of caregiver burden at baseline on medication compliance at the seven-month follow-up, nor did it demonstrate either a direct effect on clinical outcome at the 15-month follow-up or an indirect effect through its effect on medication adherence.
Of the covariates measured, only caregiver stigma had a significant direct effect on caregiver burden—that is, greater perceptions of stigma were related to higher levels of burden—and a significant indirect effect on emotional overinvolvement that was mediated by burden. The caregiver's relation to the patient was significantly related to caregivers' emotional overinvolvement in the expected direction, with parents having higher levels.
Because previous research has suggested that expressed emotion predicts relapse only if assessed when the patient is acutely symptomatic (33), we examined the bivariate associations between expressed emotion parameters at baseline and outcome at the 15-month follow-up within three subgroups of patients: those who were an inpatient, those who met criteria for a major affective episode at baseline, and those who were an inpatient and met criteria for a major affective episode at baseline. These analyses did not demonstrate a significant association between either critical comments or emotional overinvolvement and outcome at the 15-month follow-up. Even when the sample was limited to these more acute subgroups of patients, expressed emotion parameters did not have a significant direct effect on outcome in this study. To evaluate a potential effect of medication on our outcome model, the associations of medication adherence at the seven-month follow-up, outcome at the 15-month follow-up, and use (compared with nonuse) of mood stabilizers or any one of three classes of adjunctive medications (antipsychotics, antidepressants, and minor tranquilizers) were examined with Pearson r correlation coefficients. None of these associations approached statistical significance.
Discussion
This study suggests that families' experiences of burden in caring for relatives with bipolar illness influence the courses of illness indirectly through the effect of burden on the family's affective response and the patient's medication adherence. Families who reported experiencing higher levels of burden displayed higher levels of emotional overinvolvement, and patients whose caregivers were more emotionally overinvolved were less adherent to medication. As a result, these patients were more likely to have a major affective episode over time. Although observational methods—such as structural equation modeling—cannot prove causality, these data are consistent with the hypothesis that families who experience distress in relation to the patient's illness behave differently toward the patient than caregivers who evaluate these factors as less distressing and that this differential response and its sequelae influence clinical outcome among patients with bipolar disorder. Although a previous study of schizophrenia outcome found a positive association between expressed emotion and medication nonadherence (34), the study reported here is, to our knowledge, the first to demonstrate an association between these variables for bipolar disorder. It is of interest that the previous study by Perlick and colleagues (4) found that caregivers' attitudes and behavior toward patients were significantly associated with medication adherence at the seven-month follow-up, when the patients showed reduced symptoms overall, but not at baseline, during the acute phase of the episode. It is possible that when patients are admitted for treatment of an acute episode of bipolar illness, they are relatively adherent to their medication. However, as patients' symptoms remit—which is associated with increased instances of nonadherence (16) and more variability in adherence in the cohort overall—family factors may exert a greater influence.
It is noteworthy that although neither the severity of patients' symptoms nor whether they lived with the caregiver contributed significantly to the caregivers' burden, caregivers' perceptions of stigma in relation to their relatives' bipolar disorder did. This finding suggests that perceived stigma may represent a greater source of distress to caregivers than has previously been recognized.
Because previous research has shown critical comments to be a more consistent predictor of relapse than emotional overinvolvement (35), the finding that only emotional overinvolvement was indirectly predictive of clinical outcome was unanticipated and cannot be fully explained. Because research has found that parents tend to be more emotionally overinvolved than spouses (23) and that emotional overinvolvement among mothers is the best predictor of patients' relapse (36), the higher proportion of parents relative to spouses included in this substudy may have contributed to our findings.
Consistent with previous studies (13,14,37), family burden was positively associated with both emotional overinvolvement and critical comments. However, only the association with emotional overinvolvement was significant. Recent work has suggested that critical comments and emotional overinvolvement may reflect different aspects of a family's affective response or may identify subgroups of family members with differing adaptations. For example, one study found that high burden ratings four months after hospital discharge were related to persistently high levels of emotional overinvolvement but not to persistently high levels of critical comments (38), suggesting that high emotional overinvolvement alone may reflect a relatively enduring adaptation among caregivers who experience chronically high burden. Other studies have indicated that emotional overinvolvement, but not critical comments, is related to the use of avoidance coping (39), which has been associated with depression (40,41) and appraisals of hopelessness (39,42).
The study sample was relatively small. Because the CFI is especially labor intensive, Perlick and colleagues (4) decided to administer this measure to only those caregivers who were enrolled in the first nine months of the study. Therefore, although participation in the CFI and in the study described here did not reflect a selection bias, it is possible that our findings might differ with a larger study cohort. Because our measure of adherence relies on self-report, it may be unreliable because of deception, insufficient information, insufficient understanding of the regimen, or faulty recall. However, studies have shown that patients' self-reports of adherence correspond highly with pill counts (43,44). In addition, the medication adherence measure used in this study has demonstrated high concordance with chart records of steady-state plasma drug concentrations (45).
Conclusions
This study suggests that the burden experienced by family members who are attempting to cope with the behavioral manifestations and social consequences of bipolar disorder does not affect family members alone. Rather, the experience of burden appears to initiate a sequence of caregiver and patient behaviors that adversely affects clinical course and outcome, in part by reducing medication adherence. Recent meta-analyses of schizophrenia studies have demonstrated that family interventions result in reduced burden and increased medication adherence (46,47). Our findings underscore the need for additional research on interventions to reduce burden among caregivers of patients with bipolar disorder. Initial reports of such interventions are promising (48). Finally, our findings suggest that research on factors influencing patient outcome, such as managed care or new pharmacotherapies, should consider the impact of these policies and treatments on family members as well.
Acknowledgment
This study was supported by grant MH-51348 from the National Institute of Mental Health.
Dr. Perlick, Dr. Rosenheck, and Dr. Maciejewski are affiliated with the department of psychiatry at the Yale University School of Medicine in New Haven, Connecticut. Dr. Perlick and Dr. Rosenheck are also with the Veterans Affairs Connecticut Healthcare System, Northeast Program Evaluation Center, 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]). Dr. Clarkin and Dr. Sirey are with the Westchester Division of the New York Presbyterian Hospital in White Plains, New York, and with the department of psychiatry of Weill Medical College of Cornell University in White Plains. Dr. Struening and Dr. Link are with the department of epidemiology of mental disorders at New York State Psychiatric Institute and with the School of Public Health at Columbia University in New York.
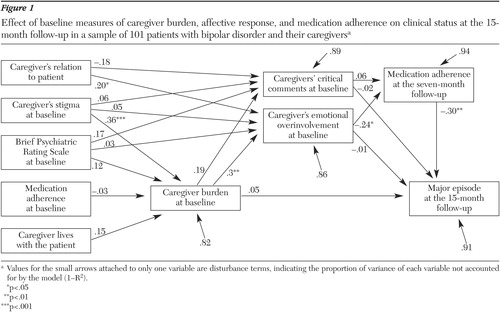
Figure 1. Effect of baseline measures of caregiver burden, affective response, and medication adherence on clinical status at the 15-month follow-up in a sample of 101 patients with bipolar disorder and their caregiversa
a Values for the small arrows attached to only one variable are disturbance terms, indicating the proportion of variance of each variable not accounted for by the model (1-R2).
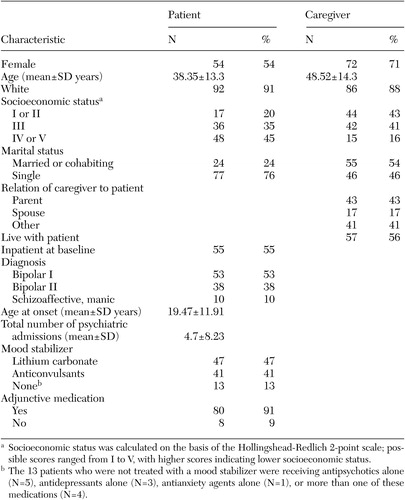 |
Table 1. Characteristics of 101 patients with bipolar disorder and their family caregivers
1. Platt S, Weyman A, Hirsch A, et al: The social behavior assessment schedule (SBAS): rationale, contents, scoring, and reliability of a new interview schedule. Social Psychiatry 64:43–55, 1978Google Scholar
2. Perlick D, Stastny P, Mattis S, et al: Contribution of family, cognitive, and clinical dimensions to long-term outcome in schizophrenia. Schizophrenia Research 6:257–265, 1992Crossref, Medline, Google Scholar
3. Falloon IRH: Family Management of Schizophrenia: A Study of Clinical, Social, Family, and Economic Benefits. Baltimore, Johns Hopkins University Press, 1985Google Scholar
4. Perlick D, Rosenheck RA, Clarkin JF, et al: Impact of family burden and patient symptom status on clinical outcome in bipolar affective disorder. Journal of Nervous and Mental Disease 189:31–37, 2001Crossref, Medline, Google Scholar
5. Perlick D, Clarkin JF, Sirey J, et al: Burden experienced by care-givers of persons with bipolar affective disorder. British Journal of Psychiatry 175:56–62, 1999Crossref, Medline, Google Scholar
6. Vaughn CE, Leff J: The influence of family and social factors on the course of psychiatric illness: a comparison of schizophrenic and depressed neurotic patients. British Journal of Psychiatry 129:127–137, 1976Crossref, Google Scholar
7. Spitzer RL, Endicott J, Robins E: Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry 35:773–782, 1978Crossref, Medline, Google Scholar
8. Endicott J, Spitzer RL: A diagnostic interview: schedule for affective disorders and schizophrenia. Archives of General Psychiatry 35:837–844, 1978Crossref, Medline, Google Scholar
9. Pollak CP, Perlick D: Sleep problems and institutionalization of the elderly. Journal of Geriatric Psychiatry and Neurology 4:204–210, 1991Crossref, Medline, Google Scholar
10. Lazarus RS, Folkman S: Stress, Appraisal, and Coping. New York, Springer, 1984Google Scholar
11. Hooley JM, Rosen LR, Richters JE: Expressed emotion: toward clarifications of a critical construct, in The Behavioral High-risk Paradigm in Psychopathology. Edited by Miller G. New York, Springer, 1996Google Scholar
12. Vaughn CE: Annotation: expressed emotion in family relationships. Journal of Child Psychology and Psychiatry 30:13–22, 1989Crossref, Medline, Google Scholar
13. Jackson HJ, Smith N, McGorry P: Relationships between expressed emotion and family burden in psychotic disorders: an explanatory study. Acta Psychiatrica Scandinavica 82:243–249, 1991Crossref, Google Scholar
14. Scazufca M, Kuipers E: Links between expressed emotion and burden of care in relatives of patients with schizophrenia. British Journal of Psychiatry 168:580–587, 1996Crossref, Medline, Google Scholar
15. Lawton MP, Kleban MH, Moss M, et al: Measuring caregiving appraisal. Journal of Gerontology 44:61–71, 1989Crossref, Medline, Google Scholar
16. Goodwin FK, Jamison KR: Manic-Depressive Illness. New York, Oxford University Press, 1990Google Scholar
17. Connelly CE, Davenport YB, Nurenberger JI: Adherence to treatment regimen in lithium carbonate clinic. Archives of General Psychiatry 39:585–588, 1982Crossref, Medline, Google Scholar
18. Miklowitz DJ: Longitudinal outcome and medication noncompliance among manic patients with and without mood-incongruent psychotic features. Journal of Nervous and Mental Disease 180:703–711, 1992Crossref, Medline, Google Scholar
19. Strober M, Morrell W, Lampert C, et al: Relapse following discontinuation of lithium maintenance therapy in adolescents with bipolar I illness: a naturalistic study. American Journal of Psychiatry 147:457– 461, 1990Link, Google Scholar
20. Gallagher SK, Mechanic D: Living with the mentally ill: effects on the health and functioning of other household members. Social Science and Medicine 42:1691–1701, 1996Crossref, Medline, Google Scholar
21. Carpentier N, Lesage A, Goulet J, et al: Burden of care of families not living with young schizophrenic relatives. Hospital and Community Psychiatry 43:38–43, 1992Abstract, Google Scholar
22. Struening EL, Perlick D, Link BG, et al: The extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services 52:1633–1638, 2001Link, Google Scholar
23. Goldstein MJ, Rea M., Miklowitz DJ: Family factors related to the course and outcome of bipolar disorder, in Interpersonal Factors in the Origin and Courses of Affective Disorder. Edited by Mundt MJ, Goldstein K, Hahlweg K, et al. Washington, DC, American Psychiatric Press, 1996Google Scholar
24. Finn RH: A note on estimating the reliability of categorical data. Educational and Psychological Measurement 30:71–76, 1970Crossref, Google Scholar
25. Whitehurst GJ: Inter-rater agreement for journal manuscript reviews. American Psychologist 39:22–28, 1984Crossref, Google Scholar
26. Glick ID, Chen C: The Treatment Compliance Medication Data Sheet. Cornell University Medical College, 1984Google Scholar
27. Lukoff D, Nuechterlein KH, Ventura J: Manual for expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594–602, 1986Google Scholar
28. Hoyle RH: Introduction to the special section: structural equation modeling in clinical research. Journal of Consulting and Clinical Psychology 62:427–428, 1994Crossref, Medline, Google Scholar
29. Bollen KA: Structural Equations with Latent Variables. New York, John Wiley and Sons, Inc, 1989Google Scholar
30. Loehlin JC: Latent Variable Models: An Introduction to Factor, Path, and Structural Analysis, 3rd ed. Mahwah, New Jersey, Lawrence Erlbaum Associates, 1998Google Scholar
31. Hayduk LA: Structural Equation Modeling with Lisrel. Baltimore, Md, Johns Hopkins University Press, 1987Google Scholar
32. SAS/STAT User's Guide Version 6, 4th Edition, Volume 2. Cary, NC, SAS Institute, Inc, 1990Google Scholar
33. Simoneau TL, Miklowitz DJ, Saleem R: Expressed emotion and interactional patterns in the families of bipolar patients. Journal of Abnormal Psychology 107:497–507, 1998Crossref, Medline, Google Scholar
34. Sellwood W, Tarrier N, Quinn J, et al: The family and compliance in schizophrenia: the influence of clinical variables, relatives' knowledge, and expressed emotion. Psychological Medicine 33:91–96, 2003Crossref, Medline, Google Scholar
35. Hooley JM, Hiller JB: Family relationships and major mental disorder: risk factors and preventive strategies, in Personal Relationships: Implications for Clinical and Community Psychology. Edited by Sarason BR, Duck S. England, John Wiley and Sons, Ltd, 2001Google Scholar
36. King S, Dixon MJ: Expressed emotion and relapse in young schizophrenia outpatients. Schizophrenia Bulletin 25:377–386, 1999Crossref, Medline, Google Scholar
37. Barrowclough C, Parle M: Appraisal, psychological adjustment, and expressed emotion in relatives of patients suffering from schizophrenia. British Journal of Psychiatry 171:26–30, 1997Crossref, Medline, Google Scholar
38. Boye B, Bentsen T, Notland TH, et al: What predicts the course of expressed emotion in relatives of patients with schizophrenia or related psychoses? Social Psychiatry and Psychiatric Epidemiology 34:35–43, 1999Google Scholar
39. Scazufca M, Kuipers E: Coping strategies in relatives of people with schizophrenia before and after psychiatric admission. British Journal of Psychiatry 74:154–158, 1999Crossref, Google Scholar
40. Stephens MAP, Norris VK, Kinney JM, et al: Stressful situations in caregiving: relations between caregiver coping and well-being. Psychology and Aging 3:208–209, 1998Crossref, Google Scholar
41. Powers DV, Gallagher-Thompson D, Kraemer HC: Coping and depression in Alzheimer's caregivers: longitudinal evidence of stability. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 57:P205-P211, 2002Google Scholar
42. Chakrabarti S, Gill S: Coping and its correlates among caregivers of patients with bipolar disorder: a preliminary study. Bipolar Disorders 4:50–60, 2002Crossref, Medline, Google Scholar
43. Myers ED, Brathwaite A: Outpatient compliance with antidepressant medication. British Journal of Psychiatry 160:83–86, 1992Crossref, Medline, Google Scholar
44. Myers ED, Calvert EJ: Information, compliance, and side effects: a study of patients on antidepressant medication. British Journal of Clinical Pharmacology 17:21–25, 1984Crossref, Medline, Google Scholar
45. Sirey J, Bruce ML, Alexopoulos GS, et al: Perceived stigma and patient-related severity of illness as predictors of antidepressant drug adherence. Psychiatric Services 52:1615–1620, 2001Link, Google Scholar
46. Pilling S, Bebbington P, Kuipers E, et al: Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychological Medicine 32:763–782, 2002Medline, Google Scholar
47. Cuijpers P: The effects of family interventions on relatives' burden: a meta-analysis. Journal of Mental Health 8:275–285, 1999Crossref, Google Scholar
48. Colom F, Eduard V, Sanchez-Moreno J, et al: Psychoeducation in bipolar patients with comorbid personality disorders. Bipolar Disorders 6:294–298, 2004Crossref, Medline, Google Scholar



