Treatment Retention Among Children Entering a New Episode of Mental Health Care
Abstract
OBJECTIVE: This study examined use of mental health services among children and adolescents with private insurance who were entering treatment. Variations in service use were examined by age, gender, diagnosis, recent psychiatric hospitalization, and type of insurance. Differences between children who received treatment from mental health professionals and those who were treated by primary care physicians were also examined. METHODS: Drawn from a large database, the sample comprised 11,659 new users of mental health services. Service use was defined as the total number of days children were retained in treatment and the total number of mental health contacts recorded. RESULTS: The overall mean number of visits within a six-month period was 3.9. The average duration of treatment was 75.36 days. Children who were treated by a mental health specialist were less likely to drop out of treatment and had a larger number of visits. Severity of illness, psychiatric hospitalization, and managed care insurance coverage were also associated with lower risk of dropout and greater intensity of care. CONCLUSIONS: Children's access to services does not guarantee sustained involvement in treatment. To more fully address the nature of service use among children, a closer look at specific barriers to continued involvement in services is needed.
Providing mental health services to children and adolescents is increasingly recognized as a priority area for mental health service delivery and research (1). Almost 20 years ago a report by the U.S. Office of Technology Assessment (2) expressed concern that approximately 70 percent of children and adolescents who need treatment do not receive mental health specialty services. More recently, Burns and colleagues (3) and Leaf and colleagues (4) documented continuing problems in the delivery of mental health services to children.
Even when children do receive services, 40 to 60 percent of those who enter outpatient treatment drop out relatively quickly and make only a small number of visits to their providers (3,5,6,7,8,9,10). Although several studies have examined the barriers involved, most of these studies have been limited to narrow diagnostic groups (11,12,13,14,15,16,17,18,19). In a large study of children and adolescents who received outpatient mental health services in the Fort Bragg project, Andrade and associates (20) found that only 39 percent remained in treatment for more than six months.
It has also been documented that children have only limited access to mental health specialists. Farmer and associates (21) found that of the children who received mental health services in the Great Smoky Mountains study, only 8 percent received services from a specialist. In view of these results it is important to determine whether retention improves when treatment is provided by such specialists.
The study reported here examined the use of mental health services among both children and adolescents who were entering a new episode of treatment and used a national database that compiles claims from private insurance companies. Service use was measured as both the total amount of time children remained in treatment and the number of mental health services they received. We were especially interested in variations in service use by age, gender, diagnosis, recent psychiatric hospitalization, and type of insurance and between children who received their mental health treatment from a mental health professional (a psychiatrist or a psychologist) and those who were treated exclusively by a primary care physician. We thus sought to evaluate base levels of retention in treatment and the number of services received as well as individual patient and provider characteristics associated with receipt of continued treatment.
Methods
Data and sample
The data for this study were obtained from MarketScan database. This database compiles claims from private health insurance plans nationwide and includes information about adults and dependents who are insured through the benefit plans of large employers. For confidentiality reasons, information about the specific firms participating in the national database is not available. Because this study was based on anonymous administrative data that included no personal identifying information, the approval of an institutional review board was not sought.
In calendar year 2000, of a total of 642,428 children who were covered by plans contributing to the database, 40,639 (6.3 percent) received some mental health services, and 11,659 of these were identified as new users of mental health services—that is, children who had no claims for any mental health services during the first 60 days of the year. Only children who began treatment between March 1 and June 30, 2000, were included in the analysis, to allow a full six-month tracking period.
Of the 11,659 children, 5,053 were treated exclusively by a primary care physician for a mental disorder, 5,731 were treated exclusively by a mental health specialist, and 875 were treated by both types of provider. All children who saw both a primary care physician and a mental health specialist started their mental health treatment with the primary care physician.
Measures
Number of days in treatment. For each study participant we calculated the total number of days between the initial visit and the last visit. If a participant remained in treatment for more than the observed six-month period, his or her retention was recorded as 180 days.
Number of visits (dose). We aggregated the total number of direct mental health visits by the type of provider during the six-month period. Other visits during this time—for example, referral for further psychological assessment or laboratory visits—were not counted.
Diagnosis. We defined mental health diagnosis as the presence of any ICD-9 code between 290.00 and 319.99. The primary diagnosis for each child was defined as the diagnosis associated with the largest number of outpatient visits for each child.
Diagnostic groups. We defined ten mental health diagnostic groups: attention-deficit hyperactivity disorder (ADHD) (ICD-9 codes 314.00 to 314.99), adjustment reaction (codes 309.00 to 309.09 and 309.11 to 309.99), depression (codes 296.20 to 296.39, 300.40, 309.10, and 311.00), bipolar disorder (codes 296.00 to 296.19 and 296.40 to 296.89), schizophrenia (codes 295.00 to 295.99), substance abuse (codes 291.00, 292.00, and 303.00 to 305.99), anxiety disorders (codes 300.00 to 300.09, 300.20 to 300.39, 313.00 to 313.09, and 308.00 to 308.99), eating disorders (codes 307.10, 307.50, 307.51, and 307.54), disruptive behavior disorders (codes 312.00 to 312.99), and other (codes 290.00 to 319.99, not elsewhere defined).
Hospitalization. Of the 11,659 children who entered treatment in 2000, we identified 262 who received inpatient psychiatric care during this period.
Insurance plans. We defined two major types of insurance plan: indemnity and managed care. The managed care category included both preferred provider organizations (PPOs) and point-of-service (POS) plans. Indemnity insurance plans include all programs in which there is no incentive for the patient to use a particular provider or providers but which may include deductibles or coinsurance payments. The PPO and POS plans are similar in that both establish financial incentives—through lower copayments—to use a particular list of providers. POS programs require that a designated primary care physician make a referral to a specialist.
Comorbidity index. Because we were concerned that children who were treated by mental health specialists would have more severe illness than children treated by primary care physicians, we aggregated the total number of secondary mental health diagnoses received by each participant to control for severity.
Statistical analysis
We used Cox proportional hazards regression to model the risk of early dropout from treatment and its association with gender, age, primary diagnosis, insurance plan, severity of illness, psychiatric hospitalization, and provider type. We further used Cox regression models to identify the interaction of diagnosis and provider type (primary care physician versus mental health specialists) in predicting likelihood of treatment termination. We also modeled the total number of mental health visits by using multivariate linear regression. Finally, we used logistic regression to model dropout from treatment within the first 30 days. The first model examined main effects of gender, age, diagnosis, provider, insurance plan, psychiatric hospitalization, and severity on continuation in treatment. A second model was designed to examine the effect of the interaction of diagnosis and treating provider.
Results
Sample characteristics
The sample included 11,664 children, of whom 7,168 (61.5 percent) were boys and 4,496 (38.5 percent) were girls. Their mean±SD age was 11.51±4.02 years. The sample's diagnostic mix was as follows: ADHD, 4,348 (37.3 percent); adjustment disorder, 2,306 (19.8 percent); depression, 1,829 (15.7 percent); bipolar disorder, 163 (1.4 percent); schizophrenia, 14 (.1 percent); substance use disorders, 175 (1.5 percent); anxiety disorders, 782 (6.7 percent); eating disorders, 81 (.7 percent); and disruptive behavior disorders, 676 (5.8 percent). The overall mean number of visits within a six-month period was 3.9±4.48, with an average duration of stay of less than three months (75.36±76.65 days out of 180).
Survival analysis
With severity of illness controlled for, Cox proportional hazards regression models of the risk of dropping out of treatment showed that adolescents had a greater risk of dropout than school-age children (Table 1). With the exception of schizophrenia and eating disorders, all diagnoses were associated with a significantly higher risk of termination of treatment compared with ADHD. Children who had more comorbid illnesses associated with their primary diagnosis and children who were hospitalized were significantly less likely to terminate treatment than other children, presumably because they were more severely ill.
Children who were treated by a mental health specialist or by both a mental health specialist and a nonspecialist had a significantly lower risk of dropout (hazard ratios of .69 and .71, respectively). When we examined the interaction of diagnosis and treatment provider we found that children who were treated by a mental health professional for depression, bipolar disorder, substance use disorders, eating disorders, anxiety disorders, and disruptive behavior disorders were at a significantly lower risk of dropping out of treatment within six months compared with those who were treated for these disorders by a primary care physician.
Children who were covered by PPO or POS insurance plans had a significantly lower risk of dropping out of treatment than children who were covered by indemnity insurance plans.
The results of multivariate regression analysis of the total number of mental health visits during the six-month period were generally similar to those of the survival analysis (Table 2). Adolescents, who had a higher risk of terminating treatment than school-age children, had significantly less use of mental health services during the observed six-month period. Although no significant difference was observed in the duration of treatment between boys and girls, girls had more visits during the six-month period. A summary of means is shown in Table 3.
Compared with children who had a diagnosis of ADHD, children with a diagnosis of adjustment disorder, depression, substance use disorder, anxiety disorder, eating disorder, or disruptive behavior disorder had a greater number of visits. Among the diagnostic groups, children who were treated for eating disorders had the highest number of outpatient psychiatric visits (7.54 visits), whereas children who were treated for ADHD had the fewest visits (2.43 visits). Excluding these two diagnostic groups, children attended an average of 5±.5 mental health visits during the six-month period—less than one visit per month, with little variation (Table 3).
Children who had a more severe mental illness or who had been hospitalized received significantly more outpatient services. We also found that children who were treated by a primary care physician had fewer visits than those who were treated by a mental health professional. Children covered by PPO or POS insurance plans had significantly more outpatient mental health visits than children covered by indemnity plans (Table 2).
Altogether, 45 percent of patients left treatment within 30 days. Logistic regression assessing the risk of dropout during the first 30 days of treatment showed that school-age children were less likely to terminate treatment than adolescents. Children with more severe illness or children who were hospitalized for psychiatric disorders had a lower risk of leaving treatment within the first 30 days. Compared with children who had a diagnosis of ADHD, children with a diagnosis of adjustment disorder, bipolar disorder, substance use disorder, or disruptive behavior disorder were more likely to discontinue their treatment in the first 30 days.
Children who were treated for their mental illness by a primary care physician were again at greater risk of dropping out of treatment in the first 30 days. Interactions showed that children who were treated by a mental health specialist for adjustment, depression, bipolar, substance use, anxiety, eating, or disruptive behavior disorders were significantly less likely to leave treatment within the first 30 days than those who were treated for these disorders by their primary care physician (Table 4).
Finally, children who were covered by PPO or POS insurance plans were also less likely to drop out in the first 30 days than children with indemnity insurance coverage.
Discussion
We found a low rate of continued use of outpatient mental health services among children who were fully covered by a private medical insurance plan. Children who entered outpatient mental health services remained in treatment for an average of less than three months (75.36 days) of a possible 180 treatment days and had a total of less than one mental health visit per month. Only 22 percent of children remained in treatment longer than six months, and 45 percent were treated for less than 30 days. Thus, in this sample of privately insured children, access to services did not guarantee sustained involvement in treatment.
A number of patient and service system characteristics were associated with retention and intensity of service use. In all analyses, severity of illness measured by the comorbidity index was a significant determinant of service use. Although gender was not associated with the amount of time children remained in treatment or the risk of early termination, the total number of mental health visits was greater among girls than among boys, perhaps because parents spend significantly more time talking to their daughters than to their sons and may be more attentive to their daughters' emotions (22,23,24,25).
Adolescents were more likely to drop out of treatment than school-age children. It has been suggested that parents exercise more control over young adolescents than older ones and that adolescents have more negative attitudes toward mental health treatment than younger children (6,26).
Children who were hospitalized were at a significantly lower risk of early treatment termination and received a significantly higher dose of outpatient treatment, with 41.2 percent continuing in treatment for more than six months. When severity of illness was controlled for, on all three of our measures children who were treated by a mental health specialist received more intensive services than children who were treated exclusively by a primary care physician. It is possible that these findings are accounted for by mental health specialists' ability to provide psychotherapy.
Although this study found, as did studies by Goldston and colleagues (6) and Wu and colleagues (27), that depression was associated with a higher risk of dropout before six months of outpatient treatment, when we adjusted for the type of treatment provider, depressed children who were treated by a mental health specialist were especially more likely to continue their treatment beyond six months.
Children with diagnoses of substance use disorders had the highest risk of discontinuing treatment before six months. Although the average number of days in treatment (50.91) was relatively low compared with that of children who had other mental health disorders, the number of visits among children with substance use disorders was relatively high (5.04). When we calculated the intensity of visits, measured as the average number of visits per month while in active treatment, children with diagnoses of substance use disorders received the most intensive treatment (2.7 visits per month on average). Children with substance use disorders may thus begin their treatment under intensive care for detoxification but may be at a higher risk of dropping out of treatment because of relapse.
Children with diagnoses of eating disorders had the greatest number of mental health visits in this sample. Among psychiatric disorders, anorexia nervosa is associated with one of the highest risks of mortality and is highly visible, is very physical, and requires constant interaction between the parents and the child (28,29). Parents of children with eating disorders, as opposed to disruptive behavior disorders, are highly aware of the potentially fatal nature of the disorder and are therefore likely to make greater efforts to ensure that their children continue to receive services.
We were surprised to find that both duration of involvement and the number of visits were lower among children who were covered by the presumably less restrictive indemnity insurance plans as opposed to PPO and POS plans. These differences were consistent across all three measurement domains. We can only speculate that greater deductibles and copayments under indemnity plans discourage service use more than the provider restriction of PPO and POS plans.
Comparison of our results with those of a study of children covered by an HMO suggests that the mean number of visits in private plans is somewhat greater than in HMOs (8). DeBar and colleagues (8) reported that during a 12-month period adolescents with diagnoses of mood disorders had an average of only 5.4±6.28 visits, whereas we found that children with a diagnosis of depression had an average of 5.5±5.44 visits over only six months.
This study had several limitations. The sample was limited to children and adolescents with private insurance, and it is unclear whether it was epidemiologically representative. Furthermore, it was impossible to determine from the data set whether study participants left treatment prematurely or had recovered and no longer needed services. Finally, the criterion of 60 days without an insurance claim does not fully guarantee that all the children were entering a new episode of treatment. Although the practice is illegal in some states, children who were stabilized on ADHD medications may receive a prescription that would cover more than 60 days. In such cases we may have misidentified new entrants into treatment.
Conclusions
In conducting this study we had access to one of the largest samples of children who were newly entering mental heath treatment that have been studied thus far, and we found that even full coverage by medical insurance did not guarantee sustained service use. It may have been the case that the relatively short time children spend in treatment reflects the fact that their parents are more interested in or accepting of crisis intervention than longer-term therapy. To more fully understand the nature of these patterns of service use, one would need to look more closely at the children's motivation and experience, their parents' beliefs and attitudes toward mental illness and treatment, and their capacity for understanding the emotional and physical needs of their child.
The authors are affiliated with the department of psychiatry of Yale University School of Medicine, 25 Park Street, Suite 617, New Haven, Connecticut 06519 (e-mail, ilan. [email protected]).
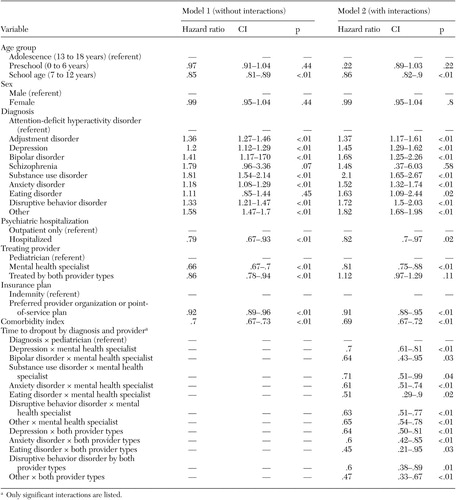 |
Table 1. Cox proportional hazards regression models of time to treatment dropout in a sample of 11,659 children and adolescents newly entering mental health services
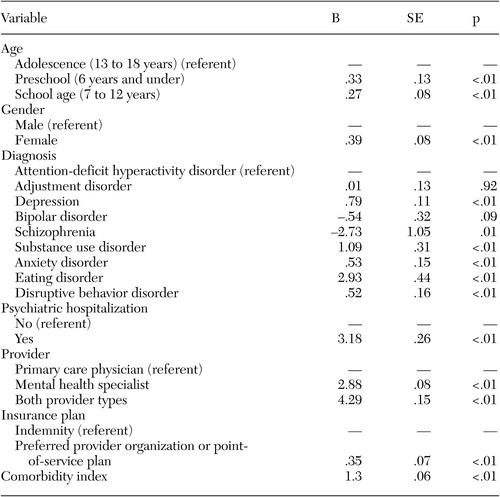 |
Table 2. Multivariate regression of number of visits within a six-month period in a sample of 11,659 children and adolescents newly entering mental health services
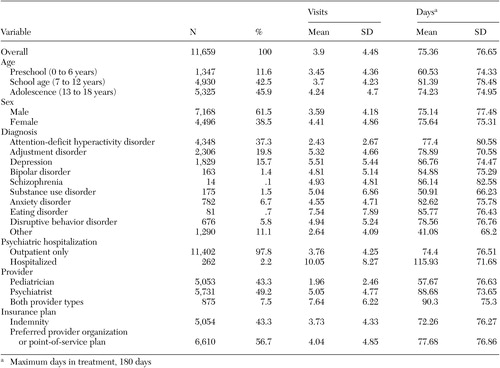 |
Table 3. Unadjusted mean number of visits and number of days in treatment within six months among children and adolescents newly entering mental health services
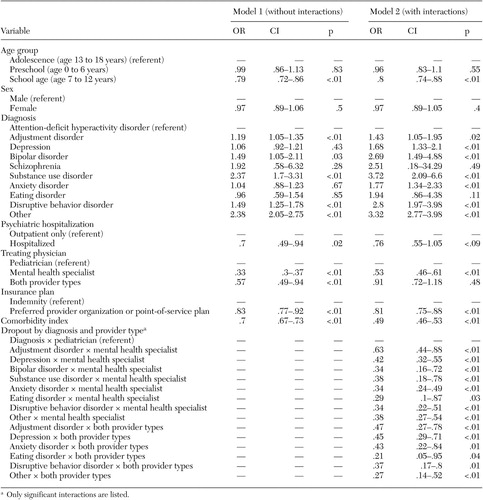 |
Table 4. Logistic regression of early dropout from treatment (?30 days) in a sample of 11,659 children and adolescents newly entering mental health services
1. Mental Health: A Report of the Surgeon General. Washington, DC, US Department of Health and Human Services, 1999Google Scholar
2. US Office of Technology Assessment: Children's Mental Health: Problems and Service: A Background Paper. Washington, DC, US Government Printing Office, 1986Google Scholar
3. Burns BJ, Costello EJ, Angold A, et al: Children's mental health service use across service sectors. Health Affairs 14(3):147–159, 1995Google Scholar
4. Leaf PJ, Alegria M, Cohen P, et al: Mental health service use in the community and schools: results from the four-community MECA study: methods for the epidemiology of child and adolescent mental disorders study. Journal of the American Academy of Child and Adolescent Psychiatry 35:889–897, 1996Crossref, Medline, Google Scholar
5. Arnold EM, Goldston DB, Ruggiero A, et al: Rates and predictors of rehospitalization among formerly hospitalized adolescents. Psychiatric Services 54:994–998, 2003Link, Google Scholar
6. Goldston DB, Reboussin BA, Kancler C, et al: Rates and predictors of aftercare services among formerly hospitalized adolescents: a prospective naturalistic study. Journal of the American Academy of Child and Adolescent Psychiatry 42:49–56, 2003Crossref, Medline, Google Scholar
7. Kazdin AE, Mazurick JL: Dropping out of child psychotherapy: distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology 62:1069–1074, 1994Crossref, Medline, Google Scholar
8. DeBar LL, Clarke GN, O'Connor E, et al: Treated prevalence, incidence, and pharmacotherapy of child and adolescent mood disorders in an HMO. Mental Health Service Research 3:73–89, 2001Crossref, Medline, Google Scholar
9. Lavigne JV, Arend R, Rosenbaum D, et al: Mental health service use among young children receiving pediatric primary care. Journal of the American Academy of Child and Adolescent Psychiatry 37:1175–1183, 1998Crossref, Medline, Google Scholar
10. Lavigne JV, Gibbons RD, Christoffel KK, et al: Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child and Adolescent Psychiatry 35:204–214, 1996Crossref, Medline, Google Scholar
11. Kazdin AE, Wassell G: Predictors of barriers to treatment and therapeutic change in outpatient therapy for antisocial children and their families. Mental Health Service Research 2:27–40, 2000Crossref, Medline, Google Scholar
12. Kazdin AE, Holland L, Crowley M, et al: Barriers to Treatment Participation Scale: evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry 38:1051–1062, 1997Crossref, Medline, Google Scholar
13. Kazdin AE, Holland L, Crowley M: Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology 65:453–463, 1997Crossref, Medline, Google Scholar
14. Levinson MC, Druss BG, Dombrowski EA, et al: Barriers to primary medical care among patients at a community mental health center. Psychiatric Services 54:1158–1160, 2003Link, Google Scholar
15. McKay MM, McCadam K, Gonzales JJ: Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal 32:353–361, 1996Crossref, Medline, Google Scholar
16. Morrissey-Kane E, Prinz RJ: Engagement in child and adolescent treatment: the role of parental cognitions and attributions. Clinical Child Family Psychology Review 2:183–198, 1999Crossref, Medline, Google Scholar
17. Owens PL, Hoagwood K, Horwitz SM, et al: Barriers to children's mental health services. Journal of the American Academy of Child and Adolescent Psychiatry 41:731–738, 2002Crossref, Medline, Google Scholar
18. Perlick DA, Rosenheck RA, Clarkin JF, et al: Stigma as a barrier to recovery: adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatric Services 52:1627–1632, 2001Link, Google Scholar
19. Wells KB, Miranda J, Bauer MS, et al: Overcoming barriers to reducing the burden of affective disorders. Biological Psychiatry 52:655–675, 2002Crossref, Medline, Google Scholar
20. Andrade AR, Lambert EW, Bickman L: Dose effect in child psychotherapy: outcomes associated with negligible treatment. Journal of the American Academy of Child and Adolescent Psychiatry 39:161–168, 2000Crossref, Medline, Google Scholar
21. Farmer EM, Stangl DK, Burns BJ, et al: Use, persistence, and intensity: patterns of care for children's mental health across one year. Community Mental Health Journal 35:31–46, 1999Crossref, Medline, Google Scholar
22. Block JH: Differential premises arising from differential socialization of the sexes: some conjectures. Child Development 54:1335–1354, 1983Crossref, Medline, Google Scholar
23. Cherry L, Lewis M: Mothers and two-year-olds: a study of sex-differentiated aspects of verbal interaction. Developmental Psychology 12:278–282, 1976Crossref, Google Scholar
24. Masur EF, Gleason JB: Parent-child interaction and the acquisition of lexical information during play. Developmental Psychology 16:404–409, 1980Crossref, Google Scholar
25. Reese E, Fivush R: Parental styles of talking about the past. Developmental Psychology 29:596–606, 1993Crossref, Google Scholar
26. Garland AF, Zigler EF: Psychological correlates of help-seeking attitudes among children and adolescents. American Journal of Orthopsychiatry 64:586–593, 1994Crossref, Medline, Google Scholar
27. Wu P, Hoven CW, Bird HR, et al: Depressive and disruptive disorders and mental health service utilization in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 38:1081–1090, 1999Crossref, Medline, Google Scholar
28. Harris EC, Barraclough B: Excess mortality of mental disorder. British Journal of Psychiatry 173:11–53, 1998Crossref, Medline, Google Scholar
29. Keel PK, Dorer DJ, Eddy KT, et al: Predictors of mortality in eating disorders. Archives of General Psychiatry 60:179–183, 2003Crossref, Medline, Google Scholar



