Comparing the Quality of Antidepressant Pharmacotherapy in the Department of Veterans Affairs and the Private Sector
Abstract
OBJECTIVE: Comparing quality of care between large health care systems is important for health systems management. This study compared measures of the quality of pharmacotherapy for patients with major depression across a sample of patients from the Department of Veterans Affairs (VA) and the private sector. METHODS: In this observational study, all patients who were given a new prescription for an antidepressant and a diagnosis of major depression in the VA during fiscal year 2000 were identified by using administrative data (N=27,713). In the private sector, a similar sample of patients were identified by using Medstat's MarketScan database (N=4,852). For both groups, measures of the quality of antidepressant pharmacotherapy were constructed. These measures were compared across the two groups by using logistic regression models. Controls for age, gender, comorbid disorders, and initial antidepressant drug prescribed were included in some models. RESULTS: Although the populations had different demographic and clinical characteristics, differences in the quality measures between the two systems were few, with the VA slightly outperforming the private sector in the prescription of antidepressants during the acute phase of treatment, the first 84 days (84.7 compared with 81 percent) and during the maintenance phase of treatment, the first 181 days (53.9 compared with 50.9 percent). Patient characteristics that were associated with quality measures included being older, being female, and having a comorbid diagnosis of substance use disorder, bipolar disorder, or anxiety or adjustment disorder. CONCLUSIONS: Both systems had relatively high rates of adherence to pharmacotherapy guidelines. Even though the populations in the two systems were different, adjusting the analyses for clinical characteristics did little to change the measured differences between the two systems.
As pressure mounts to reduce the costs of health care, there is increasing emphasis on measuring and preserving the quality of care delivered. An important component of quality evaluation and management is the ability to compare quality measures across health care systems. It is difficult to determine whether a particular measure is "too low" or "too high" unless it can be placed in the context of other systems' performance on the measure. Although comparing quality across health care systems can be difficult because the populations served can be very different, this approach may be less of a problem when comparing pharmacotherapy quality measures (1). If one system treats patients with more severe illness, one might expect readmission rates or lengths of stay to be higher in that system than in other systems, but one might not necessarily expect rates of adherence to pharmacotherapy guidelines to differ.
Previous research has considered this issue for schizophrenia pharmacotherapy. Leslie and Rosenheck (2) compared treatment for schizophrenia across two health care systems. Overall, the study found relatively low rates of adherence to antipsychotic pharmacotherapy recommendations. Across the two systems, quality results were mixed, with the Department of Veterans Affairs (VA) outperforming the private sector on some measures and doing worse on others. In other work, these researchers have compared length of stay, readmission rates, and access to outpatient services across these two sectors. Although the private sector modestly outperformed the public sector on most quality measures, the authors attribute these differences to differences in populations; the VA treats a more severely ill population (3). A more common illness, major depression, has yet to be studied. Depressive disorders are highly prevalent and have a substantial impact on functioning and quality of life (4,5,6). Treatment guidelines indicate that antidepressant medication and psychotherapy are effective treatments (7,8,9,10,11). Other research suggests that adherence to these treatment guidelines improves functioning (12).
This study quantified the quality of antidepressant use so that quality of care can be compared across systems. The goals of this study were to build on measures of the quality of pharmacotherapeutic care for depression that had been developed elsewhere (13) and to use these measures to compare the quality of care in the VA with that in the private sector for fiscal year 2000. Specifically, the goals of the study were to determine the extent to which patients in conjunction with their providers met several widely used quality targets and to investigate whether significant differences exist between the two systems on these measures.
Methods
Sources of data
VA data for this study came from national VA administrative databases. By using the outpatient encounter file, all VA outpatients who were given a diagnosis of major depression in fiscal year 2000 (October 2000 to September 2001) were identified. Patients were classified as having major depression if they had at least one outpatient encounter in which they were given a primary or secondary diagnosis of major depression (ICD-9 diagnostic codes 296.2 and 296.3) (14). Information on other comorbid mental disorders, age, and gender were also collected from the encounter file. Next, all outpatient prescription drug records for an antidepressant medication for these patients during this period were obtained from the VA drug benefit management system. Although patients could receive medications outside the VA system, our final sample included only those outpatients who received antidepressant medications from VA pharmacies.
Data for the private sector came from Medstat's MarketScan database, which contains claims information for a national sample of more than 2.6 million enrollees in fiscal year 2000. The claims data cover employees and retirees of approximately 45 large corporations and their dependents. The claims data are collected from more than 100 different insurance plans, including Blue Cross and Blue Shield, and third-party administrators. We used the same algorithm to construct the two samples: patients with one or more outpatient visits with a diagnosis of major depression were identified, the sample was limited to patients with corresponding antidepressant prescription pharmacy information, and only patients with at least one claim for antidepressant medication were included in the final sample. Because of the use of secondary data, informed consent was waived by the VA Connecticut institutional review board.
Measures
For each patient, the first prescription for an antidepressant medication during the year was identified. To make sure we were considering the index prescription, we considered only episodes in which the individual had no record of antidepressant medication for eight weeks before the initial prescription. We considered care received within six months of initial treatment. By using this algorithm, we identified 27,713 new episodes of antidepressant drug treatment for major depression with the VA data and 4,852 new episodes with the Medstat data (15,16,17).
To develop quality measures, we first examined the clinical guidelines available for the treatment of depression (7,8,9). We sought measures that were consistent with available clinical guidelines and that could be compared across health systems and populations. Thus we considered the Health Plan Employer Data and Information Set (HEDIS) 2002 antidepressant medication management measure. The HEDIS measure has three components (13). The first is optimum practitioner contact: the percentage of members who received at least three follow-up office visits in the 12 weeks after a diagnosis of depression and prescription of antidepressant medication. The second is the percentage of members who received effective acute-phase treatment in the 12 weeks after a new episode of depression. The third component is the percentage of members who received effective continuation-phase treatment in the six months after a new episode of depression.
Because we were interested primarily in pharmacotherapy, we focused on the latter two components of the HEDIS measure, which are clearly measurable with administrative data. We also looked at the American Psychiatric Association (APA) guidelines, which suggest that patients should be maintained on antidepressants for 16 to 20 weeks after remission to prevent relapse (9). For each individual in the study sample, we computed whether the patient remained on any antidepressant—regardless of the initial antidepressant prescribed—for at least 84 days (acute treatment phase), 140 days (APA guideline), and 181 days (continuation phase).
The APA guidelines also suggest that patients should be evaluated at eight weeks, and, if they are not responding, the medication should be reconsidered. Thus we also calculated the number of patients who switched to a new antidepressant in both groups.
Statistical analysis
Data analysis proceeded in several steps. First, the proportion of patients with the following characteristics was determined: patients who received at least 84, 140, and 181 days of antidepressants and those who switched to a different type of antidepressant. Chi square tests were used to assess differences in quality measures, the presence of comorbid psychiatric disorders, and the initial antidepressant prescribed between the VA and the private sector.
Next, we considered the effect of service system and patient characteristics on the quality measures described above. Because the quality measures are dichotomous, logistic regression was used to estimate the models. We were interested in whether the addition of certain variables to the model would mitigate the association of the specific health care system with the quality measures. Thus our model building strategy was to do sequential analyses. We began with our simplest model. This model included an indicator variable that equaled one if the patient was from the VA system and age and gender. Because patients with comorbid mental disorders may be more severely ill and difficult to treat, in the next model we added a set of dichotomous variables that described whether the patient had a primary or secondary diagnosis of mental illness, in addition to the diagnosis of major depression, during fiscal year 2000. Table 1 notes the specific diagnoses considered. Note that in some cases patients had more than one comorbid mental disorder. In the final model, we added another set of dichotomous variables that indicated the initial antidepressant prescribed. This final model would determine whether system differences were potentially caused by a different mix of antidepressant medications used, perhaps because of formulary restrictions. In all cases, SAS 8.0 was used to estimate models.
Results
Table 1 indicates characteristics of the study sample, stratified by health care system. The VA sample was overwhelmingly male (89.1 percent), which is characteristic of the VA population. The private sector was more evenly divided across genders (32.1 percent male). Patients in the VA were significantly older than those in the private sector (53 years compared with 40 years). In almost all cases, rates of comorbid conditions were significantly different across the two populations, with the VA population having more comorbid mental disorders: alcohol use disorder (23 percent in the VA compared with 1.7 percent in the private sector), drug use disorder (17.9 percent compared with 1.8 percent), posttraumatic stress disorder (28.5 percent compared with 1.6 percent), and personality disorder (8.2 percent compared with .4 percent, p<.001 for all).
Table 2 reports the quality measures of antidepressant pharmacotherapy for the two systems. In all cases, the VA did better in the raw quality scores. For example, 84.7 percent of patients in the VA received 84 days of treatment, compared with 81 percent in the privately insured population. This difference remained about the same in absolute terms when maintenance treatment was considered (181 days), with 53.9 percent of patients in the VA and 50.9 percent of those in the private sector receiving guideline-level treatment.
We also considered the number of episodes of treatment for which a patient began treatment with one antidepressant and over the course of treatment was switched to a different antidepressant. Somewhat surprising, given the significant differences between the two populations, was our finding of no difference in rates of switching medication in the two populations. In both cases, 29 percent of patients were switched to a different antidepressant during treatment.
Table 3 indicates the logistic regression results. We present results only for the 84- and 181-day quality measure; results for the 140-day measure were qualitatively similar to results for the 84- and 181-day measures. Table 3 presents odds ratios that indicate the association between the system of care and the quality measures when age and gender were controlled for. As model 1 shows, when the analysis controlled for these patient characteristics, VA patients were still more likely to receive 84 days of antidepressant treatment, with an odds ratio of 1.145 (p<.01). However, for the 181-day quality measure, patients were not significantly more likely to receive antidepressant treatment in the VA system. The association of age was statistically significant across all the models; older patients were more likely to receive antidepressant medication at guideline levels at both the 84- and 181-day quality measure (p<.001 for both). Females were significantly more likely to receive guideline-level treatment at both the 84- and 181-day quality measure (p<.001 for both).
Table 3 also presents the results when we controlled for age, gender, and the presence of comorbid conditions (model 2). Even though the two populations differed significantly in the presence of comorbid mental disorders, adding these variables to the model did not significantly affect the measured association between the health care system and quality measures. For the 84-day measure, the odds ratio decreased slightly and was no longer significant; no differences were found between the two systems of care for the 181-day quality measure. The comorbid conditions did affect the likelihood that a patient received guideline-level antidepressant treatment. For the 181-day quality measure, patients with an alcohol use disorder were less likely to receive guideline-level care (odds ratio=.871, p<.001), as were patients with a comorbid drug use disorder (odds ratio=.788, p<.001). Patients with bipolar disorder, posttraumatic stress disorder, or anxiety or adjustment reaction were all significantly more likely to receive guideline-level treatment.
Model 3 (Table 3) includes a set of dummy variables that indicate the initial pharmacologic agent prescribed. Although many of the individual drug dummy variables were significant, the model showed few changes to the estimated differences between the VA and the private sector. For the 84-day measure, when the analyses controlled only for age and gender (model 1), patients were significantly more likely to reach guideline-level care in the VA system (odds ratio=1.145; Table 3). Once model 3 controlled for comorbid diagnoses and specific pharmacologic agents, this odds ratio was 1.11. As with the other models, the 181-day measure showed that patients were not significantly more likely to be treated in the VA system.
Finally, we assessed whether switching from the initial antidepressant to a new antidepressant was associated with the 181-day quality indicator. We found that these two variables were correlated at the individual level (rho=.125, p<.001). In these data, we found that 29 percent of patients switched medications. Given that 25 to 50 percent of patients are not expected to respond to the initial antidepressant, this overall rate seems reasonable.
Discussion
This study compared the quality of pharmacotherapy for major depression among patients in the VA and the private sector. We found that VA patients were significantly more likely to receive an antidepressant at guideline levels. However, the difference between the two health care systems was small—about 3 percentage points. It was surprising that, given two groups that differ substantially, the quality results were so similar. One potential explanation is that pharmacotherapy adherence may be determined by physician characteristics rather than patient characteristics. Patient characteristics that were significantly associated with some of the quality measures included being older, being female, and having a comorbid mental disorder. Because antidepressants are an important component of treatment for major depression, it was heartening to find that many of the patients who were given prescriptions for antidepressants in fiscal year 2000 received these prescriptions for the length of time that the guidelines recommend.
Developers of treatment guidelines recognize that actual practice may differ from guidelines under special clinical circumstances. Hence, an important component of quality evaluation is to be able to benchmark quality measures across systems of care. This study is the first that we are aware of to assess the quality of pharmacotherapy for depression in this way. Few studies have compared quality measures across health care delivery systems. A previous study by Leslie and Rosenheck (2) found that differences between the VA and the private sector in quality of inpatient and outpatient care for patients with schizophrenia were modest and that these differences were likely attributed to the fact that VA patients are generally more severely ill than patients in the private sector. Our results are similar to those of this earlier study in that there were small or no differences in overall quality. Pharmacotherapy appears to be less affected by differences in patient characteristics across service systems than by measures of quality based on patterns of service use.
The calculation of our measure differed in several notable ways from the official HEDIS measure. For example, we followed individuals only for 181 days, whereas HEDIS requires a 245-day follow-up. To identify new episodes, we looked back eight weeks for an antidepressant prescription, whereas the HEDIS measures consider a 13-week history. We considered only patients with a diagnosis of major depression. In contrast, the HEDIS measures allow for a wider array of diagnoses. Finally, the HEDIS measures excludes patients with inpatient stays for psychiatric or substance use disorders.
Demographic variables were significant predictors of adherence to treatment recommendations. Younger patients and males were less likely to receive guideline-level treatment. Patients with a comorbid psychiatric disorder were more likely to adhere to treatment recommendations. The exception was that patients with a comorbid substance use disorder were significantly less likely to adhere to treatment. Of course, comorbid disorders may not be reliably measured in administrative data, because some providers may be less likely to record certain diagnoses.
These data have several limitations. Previous research suggests that many individuals with depression are never identified in a clinical setting (and thus would not be included in our study). In one national sample, only 81 percent of individuals with a probable anxiety or depressive disorder saw a primary care physician. Among individuals with a probable disorder, only 26 percent received an antidepressant or anxiolytic medication (18). The accurate identification of disorders is an aspect of quality that could not be considered because of the limitations of our data. If one system is more likely to correctly identify individuals with major depression, this selection may lead to a bias in our measures.
Because we considered only the ICD-9 codes 296.2 and 296.3, we may have limited our analyses to individuals with the most severe symptoms. Thus, although these health care systems may be providing high-quality care for those with the most severe symptoms, we cannot make statements about the care for the large number of patients who were given a diagnosis of other types of depression. It is also possible that patients may have been given a diagnosis of depression initially and later had their diagnosis changed to another psychiatric diagnosis.
Another important consideration is that we attempted to mimic HEDIS measures to the extent these data would allow, and it is possible that some providers were aware of the specific HEDIS measures and were specifically targeting these criteria for the period considered. This fact may be particularly true of the Medstat data, because these data come from a private system that may be reporting HEDIS measures. Unfortunately, we do not have any specific information on whether these plans were reporting HEDIS measures for the period considered here. However, we do know that for VA providers, during this period, no specific initiatives were in effect that suggest providers were specifically targeting these measures.
Other limitations include those relating to the use of administrative databases to measure quality. For example, because of limitations of these data and the complexity of identifying high-quality care, we considered all filled prescriptions to be taken and we did not consider the dosage of the antidepressant or the number of outpatient mental health visits associated with a new depression diagnosis. These may be important components of high-quality care that were overlooked in this study.
Conclusions
This article presents a rare comparison of the quality of pharmacologic care for depression across public and private service systems. Although it treats a more socially disadvantaged population, the VA performed about the same as the private sector on the measures examined here. More than 80 percent of patients who began antidepressant treatment achieved guideline-level acute-phase treatment in both the private and the VA system.
The authors are affiliated with the department of health policy at Yale School of Medicine, P.O. Box 208034, Suite 300, New Haven, Connecticut 06520-8034 (e-mail, [email protected]). Dr. Leslie and Dr. Rosenheck are also with the New England Mental Illness Research Education and Clinical Center in the Department of Veterans Affairs in West Haven, Connecticut.
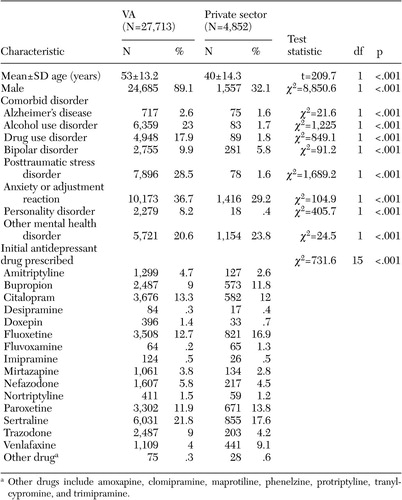 |
Table 1. Characteristics of patients from the Department of Veterans Affairs and the privatesector who were given a diagnosis of major depression and a new prescription for antidepressants in fiscal year 2000
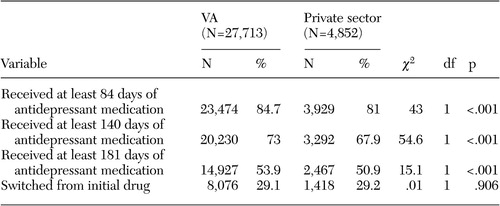 |
Table 2. Quality measures for the treatment of depression among patients from the Department of Veterans Affairs and the private sector
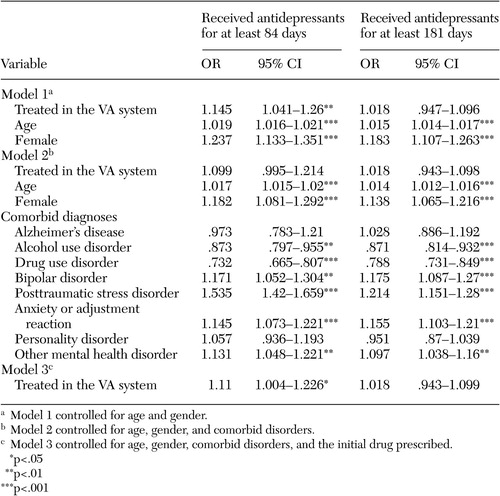 |
Table 3. Logistic regression analyses to determine the association of health care system and demographic and clinical characteristics with antidepressant pharmacotherapy quality indicators among patients in the Veterans Affairs (VA) system and in private-sector health plans (N=32,565)
1. Leslie DL, Rosenheck RA: Comparing quality of mental health care in public sector and privately insured populations: first efforts and methodological challenges. Psychiatric Services 51:650–655, 2000Link, Google Scholar
2. Leslie DL, Rosenheck RA: Benchmarking the quality of schizophrenia pharmacotherapy: a comparison of the Department of Veterans Affairs and the private sector. Journal of Mental Health Policy and Economics 6:113–121, 2003Medline, Google Scholar
3. Leslie DL, Rosenheck RA: Inpatient treatment of comorbid psychiatric and substance abuse disorders: comparison of public sector and privately uninsured populations. Administration and Policy in Mental Health 26:253–268, 1999Crossref, Medline, Google Scholar
4. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and twelve-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the national comorbidity survey. Archives General Psychiatry 51:8–19, 1994Crossref, Medline, Google Scholar
5. Wells KB, Stewart A, Hays RD, et al: The functioning and well-being of depressed patients: results from the medical outcomes study. JAMA 262:914–919, 1989Crossref, Medline, Google Scholar
6. Wells KB, Stewart A, Hays RD, et al: Functioning and well-being outcomes of patients with depression compared with chronic general medical illness. Archives General Psychiatry 2:11–19, 1995Google Scholar
7. Depression Guideline Panel: Depression in Primary Care: Vol 2. Rockville, Md, Department of Health and Human Service, Agency for Health Care Policy Research, 1993Google Scholar
8. Mulrow CD, Willias JW, Trivedi M, et al: Treatment of Depression: Newer Pharmacotherapies: Evidence Report/Technology Assessment No 7. AHCPR pub no 99–014. Rockville, Md, Agency for Health Care Policy and Research, 1999Google Scholar
9. Practice guidelines for major depressive disorder in adults: American Psychiatric Association. American Journal of Psychiatry 150:1–26, 1993Link, Google Scholar
10. Snow V, Lascher S, Mottur-Pilson C: Pharmacologic treatment of acute major depression and dysthymia. Annals of Internal Medicine 132:738–742, 2000Crossref, Medline, Google Scholar
11. Schulberg HC, Marjorie S, McClelland M, et al: Assessing depression in primary medical and psychiatric practices. Archives of General Psychiatry 42:1164–1170, 1985Crossref, Medline, Google Scholar
12. Sherbourne CD, Wells KB, Duan N, et al: Long-term effectiveness of disseminating quality improvement for depression in primary care: randomized controlled trial. Archives of General Psychiatry 58:696–703, 2001Crossref, Medline, Google Scholar
13. The State of Health Care Quality, 2002. National Committee for Quality Assurance. Available at www.ncqa.org/sohc2002Google Scholar
14. International Classification of Diseases 9th Revision, Clinical Modification, 2nd ed. Washington, DC, DHHS pub no PHS-80–1260. Washington, DC, Public Health Service, Department of Health and Human Services, 2004Google Scholar
15. Wingert TD, Kralewski JE, Lindquist TJ, et al: Constructing episodes of care from encounter and claims data: some methodological issues. Inquiry 32:430–443, 1995Medline, Google Scholar
16. Keeler EB, Wells KB, Manning WG, et al: The demand for episodes of mental health services. RAND report no R-3432-NIMH. Santa Monica, Calif, RAND, 1986Google Scholar
17. Wells KB, Roland S, Sherbourne CD, et al: Caring for Depression: A RAND Study. Cambridge, Harvard University Press, 1996Google Scholar
18. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Crossref, Medline, Google Scholar



