Use of Medical and Behavioral Health Services by Adolescents With Bipolar Disorder
Abstract
OBJECTIVE: This study compared use of medical and behavioral health care by adolescents with bipolar disorder and other adolescents and identified areas in need of more clinical attention. METHODS: Medical and behavioral health insurance claims from 1996 for 100,880 adolescents were examined and categorized. Differences between and among various categories of disease were explored by using multivariate analyses. RESULTS: Among the 10,970 adolescents who used at least one behavioral health service, adolescents with bipolar disorder (N=326) had significantly higher behavioral health costs than those with mood or non-mood disorders, a result driven by these adolescents' significantly higher hospital admission rates for behavioral health care. Adolescents with bipolar disorder also had significantly higher medical admission rates compared with adolescents who had other behavioral health diagnoses. More than half of the 14 medical admissions for adolescents with bipolar disorder were due to drug overdose. CONCLUSIONS: Reallocation of medical and behavioral health resources to improve ambulatory treatment of bipolar disorder among adolescents has the potential to decrease the use and costs of health care while improving the welfare of these adolescents and their families.
Bipolar disorder in adolescence is increasingly being recognized as a significant public health problem. It is a relatively common illness with a community prevalence of approximately 1 percent (1). Teenagers with bipolar disorder face major health risks from the disorder through its association with suicide, drug and alcohol abuse, and high-risk sexual situations (2,3,4,5,6,7,8,9,10). Adults with bipolar disorder incur higher behavioral health care costs and have significantly higher medical admission rates than those with other behavioral health diagnoses (11).
We retrospectively examined the cost and use of behavioral health and medical services by adolescents with a diagnosis of bipolar disorder and compared those costs between adolescents who had other behavioral health diagnoses and those who did not. The purpose of this analysis was to quantify how much of a fiscal and medical burden this disorder represents among adolescents. Given the high morbidity rate associated with adolescent bipolar disorder and the high burden of bipolar disorder found in studies of adults, we hypothesized that adolescents with bipolar disorder would have higher rates of use of behavioral health and medical services and higher costs associated with that use.
Methods
Data source
The data for the study came from all insurance claims submitted for medical or surgical and behavioral health care services (mental health and substance abuse) in 1996 by a group of approximately 1.3 million individuals enrolled in one of a group health insurance plans through an employer. This national database includes 862 employers with enrollees in all 50 states. These insurance plans all have similar benefit structures, which are described in detail elsewhere (12).
The data were from claims-level billing records. Each claim contains a plan identifier, a patient identifier (scrambled to protect patient confidentiality), the patient's relationship to the employee (self, spouse, or child), the patient's sex, the patient's date of birth, dates of the service incurred, primary diagnosis by standard ICD-9-CM code, charges, and payments. The data contain information from all processed claims, including claims that were filed but for which no insurance payments were made because the patients had not yet met their plan's deductible or had exceeded their available benefit. Pharmacy claims were not available; hence no information was available on the use or cost of medications.
Identification of adolescents
The insurance plans from which the data were extracted are all employer-offered plans. Individuals are enrolled either as an employee or as a dependent of the employee (spouse or child). Under the eligibility rules of a majority of these plans, individuals enrolled as children of employees are dropped from the plan on their 19th birthday unless they meet some continuation criteria, such as full-time student or full disability. Because we could not determine whether a child enrollee was dropped from the plan on his or her 19th birthday, we defined adolescents as those aged 12 to 18 years, inclusive, during the study year. On the basis of enrollees' birth dates, all individuals who reached at least their 12th birthday but not their 19th birthday or a later birthday at any time during the study year were identified in the data set. It is important to note that the study population consisted only of adolescents who filed at least one insurance claim, not all adolescents enrolled in the insurance plans.
Expenditures
Each claim contained the full amount of the bill, the amount covered by the insurance plan, and the amount paid by the insurance plan. For the purposes of this study, behavioral health expenditures were defined as the actual amount of behavioral health care-related charges covered and paid for by the plan. Insurance reimbursements are payments paid by the insurance plan for covered health care services (excluding pharmacy). These amounts included payments for outpatient and inpatient services from licensed providers, including payments for home care, hospital care, and other health care-related facilities and materials. They did not include any payments for medications, copayments made by patients, or patient deductible payments.
Behavioral health care services
Claims were identified by the insurance plans as behavioral health care services on the basis of primary ICD-9-CM codes as recorded by the provider on submitted claims and included both mental health and substance abuse services. Claims for behavioral health services in these insurance plans are managed separately by a large managed behavioral health care organization. These insurance plans define medical and surgical claims as all claims not classified as behavioral health claims.
Identification of patient diagnoses
Bipolar disorder and other behavioral health disorders, including substance use disorders, were identified on the basis of primary ICD-9-CM codes recorded in insurance billing claims. The codes used are available from the first author. Individuals were assigned a diagnosis if they had at least one claim involving a primary ICD-9-CM code for that diagnosis during the study year. Because an individual may have had multiple claims with different primary diagnoses, we categorized adolescents into one of four tiered, distinct, and mutually exclusive categories of diagnoses. First, we identified those who had any diagnosis of bipolar disorder and categorized them into the group with bipolar disorder. Of the remaining adolescents, we identified all those who had a diagnosis of a mood disorder and placed them into the mood disorder group. Adolescents who had any other behavioral health care diagnosis were categorized into the non-mood disorder behavioral health group. The remaining adolescents, who did not have any behavioral health diagnoses, were classified as "no behavioral health diagnosis."
Admission rates
We defined an inpatient hospital admission as one that generated a room-and-board charge by a medical facility and lasted for at least 24 hours. A readmission to the same facility within 48 hours of discharge was considered a continuation of the original admission, not a separate admission. Admission rates were defined as the total number of admissions in a year divided by the total number of patients. These admission rates apply only to the population of adolescents who filed at least one insurance claim, not to all adolescents enrolled in the insurance plan.
Analysis
We performed descriptive analysis by person, claim, and group. For categorical variables we used chi square tests to determine significance in differences between groups of adolescents. None of the continuous variables were normally distributed. Logistic regression was used to control for age and sex in all comparisons of service use between groups. For comparisons of expenditure and inpatient stays between groups, we used standard log transformations of the data before using N-way analysis of variance models to adjust for age and sex. All analyses were conducted with SAS, version 8. Data access and handling was approved by the University of Pittsburgh's institutional review board.
Results
The source data included 100,880 adolescents aged 12 to 18 years for whom at least one medical or behavioral health claim was filed at some time during 1996. Among these adolescents, 10.9 percent (10,970 adolescents) used at least one behavioral health service. Of these, .3 percent (N=326) used behavioral health services in conjunction with a diagnosis of bipolar disorder.
The composition of the four mutually exclusive diagnostic categories was as follows: any bipolar disorder diagnosis, 326 adolescents; any mood disorder but not bipolar disorder, 2,982 adolescents; any behavioral health diagnosis other than bipolar or mood disorder, 7,662 adolescents; and no behavioral health diagnosis, 89,910 adolescents. Age and sex differences among adolescents in these categories are shown in Table 1. Given that there were significant differences among some of the groups by age and sex, we controlled for those variables in the analyses described below.
Inpatient behavioral health care admissions
The overall inpatient admission rate for adolescents with bipolar disorder in this study was strikingly high, at 55.5 percent (181 of 326). Although some adolescents in the group with bipolar disorder had multiple admissions during the year, the high rate was attributable to the large number of individuals admitted. A total of 128 adolescents with bipolar disorder in this study (39.3 percent) had at least one behavioral health admission during the year. When age and sex were controlled for, adolescents with bipolar disorder were 3.4 times as likely to have a behavioral health care admission (95 percent confidence interval [CI]=2.66 to 4.42, p<.001) as those with mood disorders and 30.6 times as likely (CI=22.75 to 41.12, p<.001) as those with non-mood disorders.
Adolescents with bipolar disorder had a median duration of behavioral health care admission of eight days, which was not significantly different from that of other adolescents in this study (Table 2).
Use of emergency department services
Approximately 20 percent of adolescents who used services for bipolar disorder (66 of 326) filed a medical claim for emergency department services. After adjustment for age and sex, adolescents with bipolar disorder were 1.4 times as likely to have an emergency department claim (CI= 1.03 to 1.85, p=.03) as adolescents with other mood disorders and 1.7 times as likely (CI=1.29 to 2.28, p<.001) as adolescents with non- mood behavioral health diagnoses and 2.8 times as likely (CI=2.12 to 3.69, p<.001) as adolescents who did not use behavioral health care.
The primary reason for an emergency department claim merits attention in this population. Among adolescents with bipolar disorder, 21.4 percent of emergency department visits (18 of 84) were for drug overdose. Among adolescents who had any claims for an emergency department visit (with age and sex controlled for), those with bipolar disorder were 1.8 times as likely (CI=1.03 to 3.26, p=.039) to have an emergency department visit for drug overdose as their counterparts with mood disorders, 8.8 times as likely (CI=4.62 to 16.79, p<.001) as those with non-mood disorders, and 45.4 times as likely (CI=25 to 82.32, p<.001) as those with no behavioral health care use.
Inpatient medical care admissions
In sharp contrast with the 55.5 percent behavioral health admission rate, 4.3 percent of adolescents with bipolar disorder (14 of 326) had at least one medical admission. It is interesting to note that six of these 14 medical admissions were followed within 48 hours by a behavioral health care admission.
When age and sex were controlled for, this result was not significantly different from the rate for other adolescents who used behavioral health services during the year. However, adolescents with bipolar disorder were 2.6 times as likely (CI=1.51 to 4.62, p=.001) to experience a medical admission as adolescents with no behavioral health care use.
Among adolescents with bipolar disorder, 42.9 percent of medical admissions (six of 14) were for drug overdose. When age and sex were controlled for, adolescents with bipolar disorder were 94.9 times as likely (CI=27.53 to 326.81, p<.001) to have a medical admission for drug overdose as adolescents who used no behavioral health services and 16.3 times as likely (CI=4.63 to 57.18, p<.001) as those who used behavioral health services for a diagnosis other than bipolar disorder and mood disorder. The high proportion of medical admissions for drug overdose among adolescents with bipolar disorder was congruent with the high percentage of adolescents who presented to the emergency department with drug overdose.
The median duration of medical admissions among adolescents with bipolar disorder was two days. When age and sex were controlled for, this finding represented a significantly shorter stay than the three days for those with non-mood behavioral health diagnoses (F=5.46, df=1, 272, p=.02) but was not significantly different from that of other comparison groups in the study (Table 2).
Expenditures for care
Expenditures for care were calculated from covered charges on bills. Adolescents with bipolar disorder incurred median annual behavioral health expenditures of $2,046. When age and sex were controlled for, this expenditure was significantly higher than the median of $635 for adolescents with mood disorder (F=106.33, df=1, 2,834, p<.001) or the median of $210 for those with non-mood behavioral health disorders (F=532.90, df=1, 6,594, p<.001).
Again, when age and sex were controlled for, the pattern held for annual median medical expenditures, with $357 for adolescents with bipolar disorder, compared with $268 for those with mood disorders (F=4.19, df=1, 2,834, p=.04), $202 for those with non-mood behavioral health care use (F=13.03, df=1, 6,594, p< .001), and $175 for those with no behavioral health care use (F=90.02, df=1, 90,199, p<.001).
Discussion
Our analysis showed that in this group of health plans, a significantly higher percentage of adolescents with bipolar disorder had a behavioral health inpatient admission compared with adolescents who had other mental health diagnoses. Adolescents with bipolar disorder also used medical emergency department services at a significantly higher rate. Their medical admission rate was significantly higher than that of adolescents who did not have a mental health diagnosis, and 43 percent of their medical admissions were for drug overdose. This rate is significantly higher than that of adolescents who had other mental health diagnoses or who did not have a mental health diagnosis.
However, the medical length of stay among adolescents with bipolar disorder was shorter than that of adolescents with non-mood behavioral health disorders. One possible explanation is that adolescents with bipolar disorder use the emergency department for more acute injuries or illnesses—possibly related to overdose, injury, substance use, and high-risk sexual behavior—which could be related to active symptoms of bipolar disorder and may not require long inpatient medical stays. However, we did not explicitly assess the association of symptoms of bipolar disorder with emergency department use.
Adolescents with bipolar disorder had significantly higher median expenditures for annual behavioral health care than those in any of the other diagnostic categories; this finding was directly related to the high percentage of behavioral health admissions in this group. The medical expenses of adolescents with bipolar disorder were also significantly higher than those of other adolescents. The combination of high behavioral health expenditures and high medical care expenditures resulted in adolescents with bipolar disorder having significantly higher total annual expenditures on health services compared with adolescents who used behavioral health resources but had other diagnoses and adolescents who did not use behavioral health resources. This finding has important implications for these adolescents' insured parents, employers, and insurance plans. These costs appear to be reflective of a high number of behavioral health care inpatient admissions, a high level of use of emergency department services (possibly related to symptoms of bipolar disorder), and high medical admission rates for drug overdose.
Existing evidence indicates that pediatric bipolar disorder is a severe illness associated with high rates of impairment and a chronic or relapsing clinical course (13,14,15). Direct comparisons with other pediatric psychiatric disorders have highlighted the relative severity of pediatric bipolar disorder. Children and adolescents with bipolar disorder had two or three times the rate of significant psychosocial problems as youths with a diagnosis of attention-deficit hyperactivity disorder and had significantly higher rates of comorbid diagnoses, suicidality, and psychosis (16). In a community sample in Oregon, adolescents with bipolar disorder had twice the rate of suicide attempts and significantly more global impairment than adolescents with unipolar major depression (15). Thus it is not surprising that adolescents with bipolar disorder consumed relatively more overall medical resources than youths with other behavioral health diagnoses.
Limitations
The plans included in this study were not a representative sample of health plans but, rather, a convenience sample. The data used in this study were administrative insurance billing claims, and using administrative claims has certain inherent limitations. First, reported costs are exclusive of pharmacy costs, and hence health care expenditures reported here are underestimates. Second, only expenditures associated with filed claims were captured in this study. Thus the total amount of service use may be underreported. Third, identifying individuals who have a specific disorder by using insurance billing claims is not the same as making a clinical diagnosis. The differential diagnosis of bipolar disorder among adolescents is potentially difficult at times, and adolescents with bipolar disorder can receive misdiagnoses of other psychiatric disorders (7). The high rate of inpatient psychiatric admissions of the adolescents with bipolar disorder afforded a comprehensive evaluation of a large percentage of the group with bipolar disorder. In addition, bipolar disorder had to be the primary diagnosis in order for adolescents to be included in the group with bipolar disorder. These two factors may have reduced the possibility of overcounting individuals with bipolar disorder. Diagnostic coding errors and medical visits related to screenings for various disorders can result in erroneous identification; in addition, clinicians may be reluctant to assign a diagnosis of bipolar disorder to adolescents, given that it is such a difficult and troubling diagnosis. These claims contain only the primary diagnosis listed for the health service use, which may have resulted in an undercount of persons with bipolar disorder. Finally, the data were from 1996, and care practices may have changed since then.
Clinical implications
These significant findings highlight the urgent need for a better understanding of the diagnosis and treatment of bipolar disorder in this population. In particular, the high rate of use of emergency department services—and the high number of overdose-related emergency department visits—along with the high behavioral health admission rate among adolescents with bipolar disorder raises the question of whether hospitalization is the preferred mode of treatment for stabilizing these youths or whether improved or more intensive outpatient treatment is needed. If improved or more intensive outpatient treatments could decrease the need for hospitalization, then such an investment could provide a cost savings for insurers while potentially increasing the quality of life for this population of adolescents. Unfortunately, many behavioral health insurance plans, including most of the plans in this sample, limit the number of outpatient visits to 20 per year, which may pose the biggest barrier to improving treatment for adolescents with bipolar disorder (17).
Conclusions
We hope this study highlights to clinicians, researchers, and health insurance providers the tremendous fiscal and medical burden associated with bipolar disorder among adolescents. This often chronic, debilitating illness not only is associated with significant morbidity and suffering for patients and their families but also consumes a substantial amount of resources simply in direct medical costs to health plans. Because the bulk of the overall costs for adolescents with bipolar disorder are from inpatient psychiatric treatment, it may be cost-effective for health plans to devote additional resources to the improvement of ambulatory treatment of youths with bipolar disorder so that the need for inpatient hospitalization could be reduced. Given the paucity of studies examining treatment efficacy among adolescents with bipolar disorder, these findings highlight the need for research, development, and dissemination of effective treatments for bipolar disorder among youths. Such efforts have the potential to reduce the high overall medical costs associated with bipolar disorder in adolescence.
Dr. Peele and Ms. Xu are affiliated with the University of Pittsburgh Graduate School of Public Health. Dr. Peele is also with the department of psychiatry of the University of Pittsburgh School of Medicine, with which Dr. Axelson and Dr. Malley are affiliated. Send correspondence to Dr. Peele at 130 DeSoto Street, GSPH: A610, University of Pittsburgh, Pittsburgh, Pennsylvania (e-mail, [email protected]).
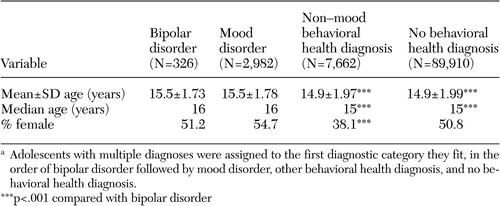 |
Table 1. claim for emergency departmentservices. After adjustment for age andCharacteristics of 12- to 18-year-olds enrolled in group health insurance plans in 1996 (N=100,880), by mutually exclusive diagnostic categoriesa
a Adolescents with multiple diagnoses were assigned to the first diagnostic category they fit, in the order of bipolar disorder followed by mood disorder, other behavioral health diagnosis, and no behavioral health diagnosis.
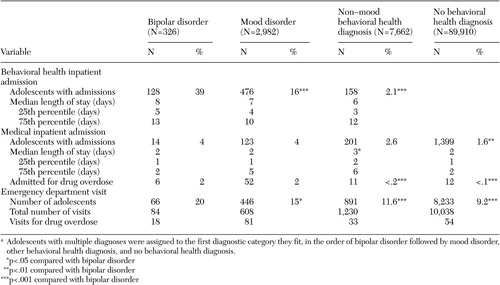 |
Table 2. Medical and behavioral health admissions and use of emergency department services among 12- to 18-year-olds in group health insurance plans in 1996 (N=100,880), by mutually exclusive diagnostic categoriesa
a Adolescents with multiple diagnoses were assigned to the first diagnostic category they fit, in the order of bipolar disorder followed by mood disorder, other behavioral health diagnosis, and no behavioral health diagnosis.
1. Lewinsohn PM, Klein DN, Seeley JR: Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. Journal of the American Academy of Child and Adolescent Psychiatry 34:454–463, 1995Crossref, Medline, Google Scholar
2. Borchardt CM, Bernstein GA: Comorbid disorders in hospitalized bipolar adolescents compared with unipolar depressed adolescents. Child Psychiatry and Human Development 26:11–18, 1995Crossref, Medline, Google Scholar
3. Brent DA, Perper JA, Goldstein CE, et al: Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Archives of General Psychiatry 45:581–588, 1988Crossref, Medline, Google Scholar
4. Brent DA, Perper JA, Moritz G, et al: Psychiatric risk factors for adolescent suicide: a case control study. Journal of the American Academy of Child and Adolescent Psychiatry 32:521–529, 1993Crossref, Medline, Google Scholar
5. Brent DA, Perper JA, Mortiz G, et al: Suicide in affectively ill adolescents: a case-control study. Journal of Affective Disorders 31:193–202, 1994Crossref, Medline, Google Scholar
6. Carlson GA: Child and adolescent mania: diagnostic considerations. Journal of Child Psychology and Psychiatry 31:331–342, 1990Crossref, Medline, Google Scholar
7. McClellan JM, Werry JS, Ham M: A follow-up study of early onset psychosis: comparison between outcomes diagnoses of schizophrenia, mood disorders, and personality disorders. Journal of Autism and Developmental Disorders 23:243–262, 1993Crossref, Medline, Google Scholar
8. Rich CL, Young D, Fowler RC: San Diego suicide study: I. young vs old subjects. Archives of General Psychiatry 43:577–582, 1986Crossref, Medline, Google Scholar
9. Rich CL, Sherman M, Fowler RC: San Diego suicide study: the adolescents. Adolescence 25:856–865, 1990Google Scholar
10. Welner A, Welner Z, Fishman R: Psychiatric adolescent inpatients: eight to ten year follow-up. Archives of General Psychiatry 36:698–700, 1979Crossref, Medline, Google Scholar
11. Peele PB, Xu Y, Kupfer DJ: Insurance expenditures on bipolar disorder: clinical and parity implications. American Journal of Psychiatry 160:1286–1290, 2003Link, Google Scholar
12. Peele PB, Lave JR, Kelleher JK: Exclusions and limitations in children's behavioral health care. Psychiatric Services 53:591–594, 2002Link, Google Scholar
13. Geller B, Craney JL, Bolhofner K, et al: Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. American Journal of Psychiatry 159:927–933, 2002Link, Google Scholar
14. Strober M, Schmidt-Lackner S, Freeman R, et al: Recovery and relapse in adolescents with bipolar affective illness: a five year naturalistic, prospective follow-up. Journal of the American Academy of Child and Adolescent Psychiatry 34:724–731, 1995Crossref, Medline, Google Scholar
15. Lewinsohn PM, Klein DN, Seeley JR: Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disorder 2:281–293, 2000Crossref, Medline, Google Scholar
16. Geller B, Bolhofner K, Craney JL, et al: Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. Journal of the American Academy of Child and Adolescent Psychiatry 39:1543–1548, 2000Crossref, Medline, Google Scholar
17. Peele PB, Lave JR, Xu Y: Benefit limits in managed behavioral health care: do they matter? Journal of Behavioral Health Service and Research 24:430–441, 1999Google Scholar



