Blood-Borne Infections and Persons With Mental Illness: Substance Abuse and the Transmission of Hepatitis C Among Persons With Severe Mental Illness
Abstract
OBJECTIVES: The authors sought to better understand the relationship of substance abuse to higher rates of transmission of hepatitis C among persons with severe mental illness. METHODS: The authors assessed 668 persons with severe mental illness for HIV, hepatitis B, and hepatitis C infection through venipuncture. Demographic characteristics, substance abuse, and risk behaviors for blood-borne infections were assessed through interviews and collection of clinical data. RESULTS: Eighty-two percent of the assessed persons were not infected, and 18 percent had hepatitis C. Among those with hepatitis C infection, 546 (82 percent) tested negative for all viruses. Of the 122 (18 percent) who had hepatitis C, 53 (8 percent) had only hepatitis C, 56 (8 percent) had both hepatitis C and hepatitis B, three (1 percent) had hepatitis C and HIV, and ten (2 percent) had all three infections. More than 20 percent of the sample reported lifetime intravenous drug use, and 14 percent reported lifetime needle sharing. Fifty-seven percent had sniffed of snorted cocaine, and 39 percent had smoked crack. A stepwise regression model was used to identify interaction effects of these behaviors and risk of hepatitis C infection among persons with severe mental illness. Use of needles and of crack cocaine were associated with a large increase in the likelihood of hepatitis C infection. CONCLUSIONS: The high rates of co-occurring substance use disorders among persons with severe mental illness, coupled with the role of substance abuse as the primary vector for hepatitis C transmission, warrants special consideration.
Hepatitis C is the most common chronic blood-borne infection in the United States; approximately four million people are infected with the virus (1). A majority of persons who become infected will develop chronic active hepatitis and be infectious to others. About one-fifth of infected individuals will develop cirrhosis or hepatocellular carcinoma if they do not receive intervention. Although approximately 1.8 percent of the general population is infected with hepatitis C (1), recent data collected by a multisite study funded by the National Institute of Mental Health suggests that 19.6 percent of adults with severe mental illness are infected (2). Moreover, most people with severe mental illness are unaware that they are infected with the hepatitis C virus. In addition, access to and use of hepatitis C-related somatic care among persons with severe mental illness is deficient (2).
Understanding the reasons for the high prevalence of hepatitis C among persons with severe mental illness is critical to the design of effective prevention and intervention strategies. Studies of both the general population and of persons with severe mental illness show a strong relationship between substance use disorders and HIV, hepatitis B, and hepatitis C infection (3,4,5,6). An estimated 60 percent of hepatitis C transmission in the United States is attributed to injection drug use (7). The most efficient routes of transmission of hepatitis C are transfusion of contaminated blood products and the use of contaminated drug paraphernalia (4,8). These routes are even more efficient for hepatitis C than for HIV. Base rates of hepatitis C infection will affect the incidence of new infections among drug users. In urban areas, where hepatitis C base rates are high, transmission patterns are alarming.
Studies of hepatitis C and injection drug use have shown prevalence rates between 65 percent and 90 percent (8,9,10). In a Baltimore study of persons who had used intravenous drugs for less than a year, 64.7 percent of participants were hepatitis C positive (11). In the Five-Site Health and Risk Study (2), significant associations were found between hepatitis C infection and lifetime intravenous drug use (p<.001), use of drugs intravenously in the previous six months (p<.001), and sharing needles during intravenous drug use (p<.001). Although the risk factors operant for hepatitis infection among persons with severe mental illness are identical to those in the general population, understanding the higher rates of transmission among persons with severe mental illness is of paramount importance.
The high rates of co-occurring substance use disorders among persons with severe mental illness, coupled with the role of substance abuse as the primary vector for hepatitis C transmission, warrant special consideration. Studies of persons with severe mental illness consistently demonstrate high prevalence rates of co-occurring substance use disorders. Persons with schizophrenia are 4.6 times as likely to meet substance use disorder criteria as the general population, and persons with affective disorders are 2.6 times as likely (12). Half of persons with a diagnosis of schizophrenia meet lifetime criteria for a substance use disorder (13). The most direct route of hepatitis C transmission is through intravenous injection. However, the knowledge that the rates of injection drug use among persons with severe mental illness are higher than among control subjects (14) is cause for concern.
People with severe mental illness also appear to have a higher risk of blood-borne infections through routes of transmission other than injection drug use. Use of intranasal and crack cocaine, having multiple sexual partners, having high-risk partners, failure to use condoms on a regular basis, homosexual activity among males, high rates of sexually transmitted diseases, trading sex for material gain, and engaging in sex while using psychoactive substances have all been documented as risk behaviors frequently found in the various populations studied (15,16,17). The use of cocaine in and of itself has been associated with riskier drug and sexual practices (11). These factors were also associated with hepatitis C infection in a 2001 study by Rosenberg and associates (2). Thus substance abuse can serve as a precursor for behaviors that act as direct vectors of infectious disease transmission.
In this study we examined the substance use and abuse patterns and correlates to hepatitis C infection among persons with severe mental illness who participated in a multisite study (2). A significant relationship has already been established between substance use disorders and hepatitis C infection (2,18). We looked at specific substance abuse behaviors and their associated risk of hepatitis C.
Methods
The study was conducted between June 1997 and December 1998 at four participating sites. Sampling and main research procedures for this study have been reported previously (2,18). Briefly, all 777 study participants were tested for hepatitis C infection. All were aged between 18 and 60 years and had severe mental illness, including diagnosis of a major mental disorder, duration of illness of at least one year, and disability in at least two life domains. Approximately 42 percent of the participants had a concurrent substance use disorder, and all were receiving inpatient or outpatient care in the public mental health systems of Connecticut, Maryland, or New Hampshire or treatment through the Department of Veterans Affairs Medical Center in Durham, North Carolina.
After providing informed consent, the study participants responded to standardized interview questions, including questions on sociodemographic characteristics, substance use, and specific risk behavior for blood-borne infections. Current alcohol and drug use disorders were identified by using the Dartmouth Assessment of Lifestyle Instrument (19). Risky drug practices were assessed with items from the AIDS Risk Inventory (20,21). The participants also received pretest counseling about HIV and AIDS and provided blood specimens through venipuncture. Details of the laboratory analyses of blood samples can be found in the earlier article by Rosenberg and colleagues (2). All participants were paid a participation fee of $35 and were provided with test results, posttest counseling, and (when appropriate) referral for treatment with medical providers. These procedures and the informed consent forms were approved by the participating institutions' institutional review boards.
Of the 777 study participants who were tested for hepatitis C, 672 individuals who were hepatitis C positive or hepatitis C negative for any tested viral infections were selected for the analyses. We chose to eliminate participants who were hepatitis C negative but who were positive for either hepatitis B or HIV in order to highlight differences between participants who were hepatitis C positive and a relatively low-risk group. Four participants for whom there was insufficient substance abuse information were dropped from the analyses, leaving 668 participants. Of these, 546 (81.7 percent) tested negative for all viruses. Of the 122 (18.3 percent) who had hepatitis C, 53 (7.9 percent) had only hepatitis C, 56 (8.4 percent) had both hepatitis C and hepatitis B, three (.5 percent) had hepatitis C and HIV, and ten (1.5 percent) had all three infections.
Site, ethnicity (dichotomized as white versus minority), age (42 or older versus 41 and younger), and gender were the covariates of interest. There were nine substance use variables of interest: alcohol or drug use disorder, lifetime history of needle use, needle use in the previous six months, lifetime history of needle or "works" sharing, needle or works sharing in the previous six months, needle or works sharing with someone who had AIDS, needle use without cleaning in the previous six months, lifetime history of intranasal cocaine use, and lifetime history of crack cocaine use.
Models were constructed by using stepwise regression analyses as exploratory tools for identifying important predictors of hepatitis C infection among persons with severe mental illness. Little is known about routes of transmission through substance abuse behavior among persons with severe mental illness, and stepwise analyses were used to reduce the number of predictors to a subset of potentially important variables (22).
The procedure was conducted in three stages. In the first stage, site, ethnicity, age, and gender were entered as covariates into the regression equation. These covariates were not subject to the stepwise selection algorithm and remained in the equation at all times. In the second stage, substance use variables were entered in forward selection with an inclusion p value of .10. A backward selection procedure was also applied by using a more liberal exclusion p value of .15. Predictors were retained in the model if they were identified by both forward and backward selection procedure variables (22).
Two substance use variables remained in the equation after both selection algorithms: lifetime history of needle use and lifetime history of crack cocaine use. In the final stage, interactions among the covariates, between the covariates and the two retained substance use variables, and between the two retained substance abuse variables were submitted to both forward and backward selection procedures. Interaction effects that remained after application of both forward and backward selection procedures were retained for the final model.
Results
The frequency of specific substance use behaviors endorsed by the study participants is shown in Table 1. The high rates of high-risk substance use behavior across all sites are consistent with high rates of substance use disorders among persons with severe mental illness. More than 20 percent of our sample endorsed lifetime needle use, of whom almost three-quarters had shared needles with another drug user. High rates of cocaine use were also notable and were far in excess of rates in the general population (23).
Bivariate relationships between all substance abuse variables and hepatitis C infection were examined. The results are summarized in Table 2. Odds ratios (ORs) are presented both unweighted and on the basis of case weights. Case weights were derived in order to equate samples on substance use diagnosis and age (24). Site ORs were calculated with reference to the Connecticut site, which had the highest prevalence of hepatitis C infection (55 percent). Confidence intervals (CIs) above 1 indicate a significant positive effect at p<.05, whereas CIs below 1 indicate a significant negative effect at p<.05. Site differences in infection rates suggest that base rates of infection in the general population affect the risk of infection. Participants from ethnic minorities, older persons, and men were more likely to test positive for hepatitis C than their counterparts. All substance abuse behaviors were associated with hepatitis C infection.
Stepwise logistic regression analyses were used to arrive at a limited number of substance use variables that predicted hepatitis C infection. Case weights to equate samples on substance use diagnosis and age (24) were used in estimating parameters for all regression models. Because the data analyzed were collected cross-sectionally, the models proposed cannot demonstrate causal relationships. As such, the terms "prediction" and "predictors" refer here to statistical analytic techniques.
The results of significance tests for the interaction effects in the model predicting hepatitis C infection from substance use behaviors are shown in Table 3. Age was the only demographic covariate that was significantly associated with hepatitis C infection. Older persons were more likely to have a diagnosis of hepatitis C infection. Age may not be a risk factor in and of itself but may reflect a complicated cohort effect involving the Vietnam War era. Gender differences in this sample are reported in the article by Butterfield and colleagues in this special section (25). Lifetime crack use, although initially significant as a main effect, turned out to be related to hepatitis C infection in a more complicated way through its relationship with lifetime needle use and site.
Table 4 displays predicted probabilities from the final model for each of the cells created by the interaction of lifetime crack use and lifetime needle use as well as lifetime crack use and interview site. In these cells, the impact of the interactions can be described as follows. The effect of needle use and crack cocaine use was to greatly increase the likelihood that a person in the sample had hepatitis C. For participants who used crack cocaine in addition to being intravenous drug users, the probability of being hepatitis C positive increased from 23 percent to 78 percent. This suggests that although needle use is risky on its own, adding crack use substantially magnifies the risk of infection among persons with severe mental illness.
The observed interaction between site and crack use may identify more than cross-site differences in the prevalence of hepatitis C infection. All sites demonstrated higher predicted rates of hepatitis C infection in the crack-use cells than in the no-use cells. Nonusers in Maryland and Connecticut had slightly higher probabilities of hepatitis C infection than nonusers in New Hampshire and North Carolina. However, the interaction was apparent with Maryland and Connecticut participants who reported crack use. These participants had higher predicted probabilities of hepatitis C infection than nonusers. The significant interaction between site and lifetime crack use disproportionately predicted risk of hepatitis C infection across sites.
Discussion and conclusions
Our study showed that the high prevalence of hepatitis C among persons with severe mental illness is related to drug use. Because of the efficiency of hepatitis C transmission through parenteral routes, any history of needle use among persons with severe mental illness is of particular concern. Our model also identified the use of crack cocaine as a particularly risky behavior for this population. The use of crack among persons from sites with high base rates of hepatitis C infection—that is, urban areas in Connecticut and Maryland—was associated with hepatitis C infection. Although the relationship between hepatitis C infection and intravenous drug use was direct, the association between crack use and hepatitis C infection among persons with severe mental illness requires closer inspection.
It is possible that the use of crack cocaine decreases the usual precautions that intravenous drug users take when they inject drugs, acts as a gateway to intravenous cocaine use, or increases other high-risk behavior. Drug injection does not necessarily transmit the hepatitis C virus, but the use of contaminated equipment greatly increases the risk (4). Persons with severe mental illness may not be able to afford their own equipment or the ingredients to clean their equipment and may not be able to learn techniques for sterilizing their needles effectively or to participate in risk-reduction needle exchange programs. Although the impact of eliminating contaminated syringes could be substantial, more recent findings suggest that even with a sterile syringe, "backloading"—using a syringe to divide doses between users—from contaminated cookers or cotton and other nonsterile practices may pose a substantial risk of transmission (8).
The elevated risk of hepatitis C infection associated with crack use among our study participants suggests that crack use may be an intermediate marker of intravenous cocaine use. Previous research has identified the use of intravenous cocaine as being associated with riskier injecting practices among heroin users (11,26). Risk-reduction education messages should include these facts and harm-reduction strategies.
The recent epidemic of smoking crack cocaine has been associated with high-risk sexual behavior, because the abuser either is disinhibited and less likely to practice safe sex or trades sex to obtain drugs. Elevated rates of hepatitis C infection among female sex workers who do not have a mental illness and who abuse crack cocaine have been documented (27). The behaviors of practicing unprotected sex in exchange for drugs or gifts and trading sex for money were all correlated with hepatitis C infection among persons with severe mental illness (2). Co-occurring high-risk substance abuse behavior is apparently driving risky sexual practice in a group of individuals who have few economic resources. Risk-reduction strategies and effective treatment interventions for co-occurring substance use disorders are critical for reducing the incidence of hepatitis C among persons with severe mental illness and should be tailored specifically for persons with severe mental illness. The exceptional risk associated with the use of crack cocaine and intravenous needles is a finding that warrants further study.
Our study had several limitations. Retrospective questioning about substance use behaviors has its limitations when used in the general population, and these limitations may be magnified in a population of persons with severe mental illness. Behavioral data were self-reported, and study participants may have consciously or unconsciously answered questions to project a certain impression. Because the original study was not specifically designed to focus on intravenous drug use behaviors, questions about injection practices were limited and did not allow us to disentangle questions about the use of sterile needles and equipment, ways in which drugs were "cooked" and filtered, and specific combinations of intravenous drug use—for example, heroin combined with cocaine as "speedballs."
Without a comparison group of persons who did not have mental illness, nothing can be said about the unique contributions of mental illness to risk behaviors. It is possible that prevalence rates and risk behaviors among the study participants simply reflect the practice patterns of the communities in which clients live and interact. Nonetheless, the unique needs of persons with severe mental illness, in terms of their high rates of substance abuse and associated cognitive impairment, have important implications for public health prevention strategies.
Given the high rates of substance use disorders among people with severe mental illness (28), as well as the newly documented risk of hepatitis among those with severe mental illness, both treatment and the secondary prevention of drug use disorders take on added import. Given the findings of our risk model, additional psychoeducational interventions focused on the use of crack cocaine are also warranted.
Dr. Osher, Dr. Goldberg, and Dr. McNary are with the Center of Behavioral Health, Justice, and Public Policy at the University of Maryland School of Medicine, 3700 Koppers Street, Suite 402, Baltimore, Maryland 21227 (e-mail, [email protected]). Dr. Swartz is with the services effectiveness research program in the department of psychiatry and behavioral sciences at Duke University in Durham, North Carolina. Dr. Essock is with the department of psychiatry at Mount Sinai School of Medicine in New York City. Dr. Butterfield is with the Health Services Research and Development Service of the Department of Veterans Affairs Medical Center in Durham, North Carolina. Dr. Rosenberg is with the New Hampshire-Dartmouth Psychiatric Research Center of Dartmouth Medical School in Hanover, New Hampshire. This article is part of a special section on blood-borne infections among persons with severe mental illness.
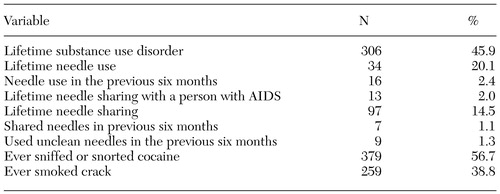 |
Table 1. Prevalence of risky drug behaviors among persons with severe mental illness at four sites (pooled N=668)
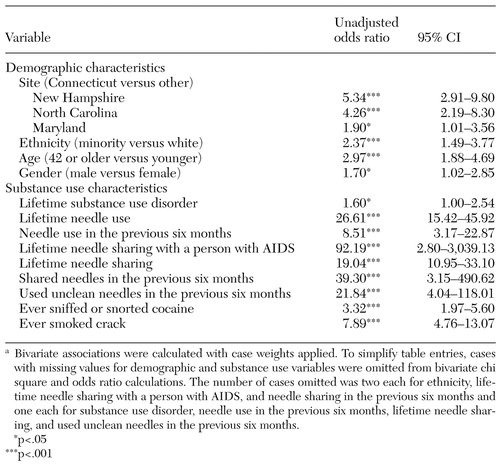 |
Table 2. Bivariate associations between predictors and hepatitis C infection among persons with severe mental illness at four sites (N=668)a
a Bivariate associations were calculated with case weights applied. To simplify table entries, cases with missing values for demographic and substance use variables were omitted from bivariate chi square and odds ratio calculations. The number of cases omitted was two each for ethnicity, lifetime needle sharing with a person with AIDS, and needle sharing in the previous six months and one each for substance use disorder, needle use in the previous six months, lifetime needle sharing, and used unclean needles in the previous six months.
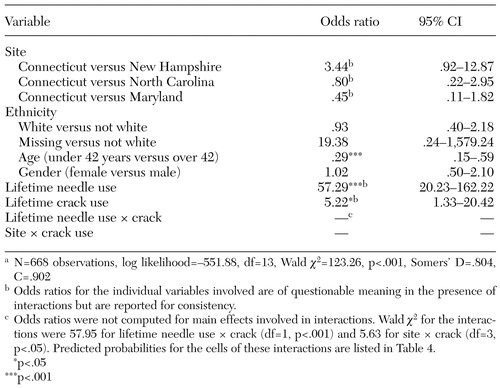 |
Table 3. Predictors of hepatitis C infection from the final model after stepwise selectiona
a N=668 observations, log likelihood=−551.88, df=13, Wald χ2=123.26, p<.001, Somers' D=.804, C=.902
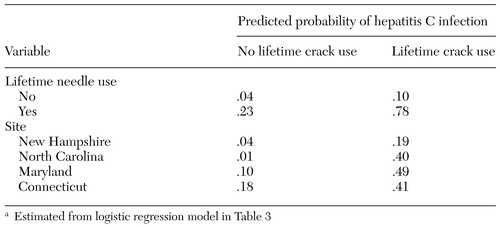 |
Table 4. Predicted probabilities of hepatitis C infection for interaction termsa
a Estimated from logistic regression model in Table 3
1. Centers for Disease Control and Prevention: Recommendation for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Morbidity and Mortality Weekly Report 47(RR-19):1-33, 1998Google Scholar
2. Rosenberg SD, Goodman LA, Osher FC, et al: Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health 91:31-37, 2001Crossref, Medline, Google Scholar
3. Caetano RK, Hines L: Changes in drinking patterns among whites, blacks and Hispanics, 1984-1992. Journal of Studies on Alcohol 56:558-565, 1995Crossref, Medline, Google Scholar
4. Diaz T, Des Jarlais DC, Vlahov D, et al: Factors associated with prevalent hepatitis C: differences among young adult injection drug users in lower and upper Manhattan, New York City. American Journal of Public Health 91:23-30, 2001Crossref, Medline, Google Scholar
5. Ericksen KP, Trocki KF: Sex, alcohol, and sexually transmitted diseases: a national survey. Family Planning Perspectives 26:257-263, 1994Crossref, Medline, Google Scholar
6. McKinnon K, Carey MP, Cournos F: Research on HIV, AIDS, and severe mental illness: recommendations from the NIMH National Conference. Clinical Psychology Review l17:327-331, 1997Google Scholar
7. Alter MJ: Epidemiology of hepatitis C. Hepatology 26(3 suppl 1):62S-65S, 1997Google Scholar
8. Hagan H, Thiede H, Weiss NS, et al: Sharing of drug preparation equipment as a risk factor for hepatitis C. American Journal of Public Health 91:42-45, 2001Crossref, Medline, Google Scholar
9. Garfein RS, Doherty MC, Monterresso ER, et al: Prevalence and incidence of hepatitis C virus infection among young adult users. Journal of Acquired Immune Deficiency Syndromes 18(suppl 1):S11-S19, 1998Google Scholar
10. Rezza G, Sagliocca L, Zaccarelli M, et al: Incidence rate and risk factors for HCV seroconversion among injection users in an area with low HIV seroprevalence. Scandinavian Journal of Infectious Disease 28:27-29, 1996Crossref, Medline, Google Scholar
11. Garfein RS, Vlahov D, Galai N, et al: Viral infections in short-term injection drug users: the prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphocyte viruses. American Journal of Public Health 86:655-661, 1996Crossref, Medline, Google Scholar
12. Mueser KT, Bennett M, Kushner MG: Epidemiology of substance use disorders among persons with chronic mental illnesses, in Double Jeopardy: Chronic Mental Illness and Substance Use Disorders. Edited by Lehman AF, Dixon LB. Chur, Switzerland, Harwood Academic, 1995Google Scholar
13. Regier D, Farmer M, Rae D, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area study. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
14. Schneier S, Siris G: A review of psychoactive substance use and abuse in schizophrenia: patterns of drug choice. Journal of Nervous and Mental Disease 175:641-52, 1987Crossref, Medline, Google Scholar
15. Carey MP, Carey KB, Kalichman SC: Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illnesses. Clinical Psychology Review 17:271-291, 1997Crossref, Medline, Google Scholar
16. Kalichman SC, Kelly JA, Johnson JR, et al: Factors associated with risk for HIV infection among chronic mentally ill adults. American Journal of Psychiatry 151:221-227, 1994Link, Google Scholar
17. McKinnon K: Sexual and drug risk behavior, in AIDS and People With Severe Mental Illness: A Handbook for Mental Health Professionals. Cournos F, Balakar N, eds. New Haven, Conn, Yale University Press, 1996Google Scholar
18. Rosenberg SD, Swanson JW, Wolford GL, et al: The Five-Site Health and Risk Study of blood-borne infections among persons with severe mental illness. Psychiatric Services 54:827-835, 2003Link, Google Scholar
19. Rosenberg SD, Drake RE, Wolford GL, et al: Dartmouth Assessment of Lifestyle instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155:232-238, 1998Abstract, Google Scholar
20. Chawarski MC, Baird JC: Comparison of two instruments for assessing HIV risk in drug abusers, in Social and Behavioural Science: Proceedings of the 12th World AIDS Conference, Geneva, Switzerland, June-July 1998. Bologna, Italy, Monduzzu Editore, 1998Google Scholar
21. Chawarski MC, Pakes J, Schottenfeld RS: Assessment of HIV risk. Journal of Addictive Diseases 17:49-59, 1998Crossref, Medline, Google Scholar
22. Hosmer DW, Lemeshow S: Applied Logistic Regression, 2nd ed. New York, Wiley, 2000Google Scholar
23. Epstein JF: Substance Dependence, Abuse, and Treatment: Findings From the 2000 National Household Survey on Drug Abuse. NHSDA series A-16, DHHS pub (SMA) 02-3642. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2002Google Scholar
24. Swartz MS, Swanson JW, Hannan MJ, et al: Regular sources of medical care among persons with severe mental illness at risk of hepatitis C infection. Psychiatric Services 54:854-859, 2003Link, Google Scholar
25. Butterfield MI, Bosworth HB, Meador KG, et al: Gender differences in hepatitis C infection among persons with severe mental illness. Psychiatric Services 54:848-853, 2003Link, Google Scholar
26. Greenfield L, Bigelow GE, Brooner RK: HIV risk behavior in drug users: increased blood booting during cocaine injections. AIDS Education Prevention 4:95-107, 1992Medline, Google Scholar
27. Ward H, Pallecaros A, Green A, et al: Health issues associated with increasing use of "crack" cocaine among female sex workers in London. Sexually Transmitted Infections 76:292-293, 2000Crossref, Medline, Google Scholar
28. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:77-31, 1996Crossref, Medline, Google Scholar



