Consumers' Perceptions of the Fairness and Effectiveness of Mandated Community Treatment and Related Pressures
Abstract
OBJECTIVE: Little research has been conducted on the attitudes of persons with psychiatric disorders toward the potentially adverse or beneficial effects of involuntary outpatient commitment and other forms of mandated community treatment. This study examined mental health consumers' appraisals of the fairness and effectiveness of mandated community treatment and related pressures to promote treatment adherence. METHODS: A total of 104 consumers who had been in treatment for schizophrenia or related disorders were interviewed in person to assess their perceptions of mandated community treatment and other legal pressures. RESULTS: Approximately 62 percent of the consumers regarded mandates as effective, and 55 percent regarded them as fair. Perceptions of the effectiveness and fairness of mandates were highly correlated. Consumers who regarded schizophrenia as a biopsychosocial disorder and who viewed themselves as ill and in need of treatment also tended to endorse the fairness and effectiveness of mandates. Those who rejected mandates as ineffective and unfair were more symptomatic and rejected a view of themselves as being ill. CONCLUSIONS: Consumers with schizophrenia who adopt a biopsychosocial view of their own illness, who are less symptomatic, and who have better insight also tend to believe that they benefit from a range of formal and informal sanctions to adhere to treatment and believe that they are imposed in the consumers' best interests and out of concern for their well-being. In contrast, consumers who reject treatment mandates tend to have more psychotic symptoms yet are less likely to perceive themselves as ill.
The use of legal mandates to improve adherence to community-based treatment among persons with serious mental illness is a controversial issue in mental health policy (1). Proponents of legal mandates such as involuntary outpatient commitment argue that this approach can improve treatment adherence, reduce relapse, and increase consumers' personal autonomy in the long run. To some consumers and other stakeholders, these gains may be a fair trade-off for the attendant short-term loss of certain personal liberties (2,3,4,5). However, others fundamentally oppose the use of coercion, arguing that it infringes on civil liberties, is largely ineffective, and may scare people away from treatment (6,7,8,9,10,11,12).
A report by Monahan and colleagues (13) concluded that mental health consumers' perceptions of coercion in the hospital admission process are largely affected by whether consumers believe they are being treated fairly. Thus even "involuntary" patients may not perceive a great deal of coercion if they are treated with respect and given a chance to express their preferences—that is, are afforded "procedural justice" (14,15,16,17). These and other studies of inpatients have generally concurred that when consumers feel that they have been treated with fairness, concern, and respect, perceived coercion is greatly mitigated (18,19,20).
Research on the use of outpatient commitment suggests that the adverse impact of coercion may be outweighed by potential benefits. A controlled study of outpatient commitment among consumers with serious mental illness in North Carolina showed that when outpatient commitment is sustained for at least six months and combined with frequent services, adherence to medication and other treatment is significantly improved, leading to significantly reduced hospital readmissions and reduced violence (21). However, another study suggested that a court order for community treatment may have no measurable effects (22).
A study of preferences for outpatient commitment relative to its perceived benefits for patients with schizophrenia showed that patients' perceptions of the adverse effects of mandated community treatment were small relative to the potential benefits of outpatient treatment (3). In a related study, persons who underwent sustained outpatient commitment reported significantly higher subjective quality of life, and a substantial proportion of patients who were subjected to extended outpatient commitment later endorsed the personal benefits of outpatient commitment—but only if they had obtained good outcomes (3,4).
Many mental health consumers who have been subjected to legally mandated treatment have experienced a variety of formal, legal, and informal pressures intended to improve treatment adherence. No study has examined consumers' own appraisals of the fairness and effectiveness of these mandates. The study reported here examined potential factors associated with the appraisal of the fairness and benefits of mandated community treatment and related pressures by using data from a survey of persons with schizophrenia-spectrum disorders.
Methods
Sample
To examine how mental health consumers appraise the fairness and effectiveness of treatment mandates, we conducted in-person interviews with a sample of 104 persons with schizophrenia-spectrum disorders in the Piedmont region of North Carolina between March 2001 and April 2002.
The study participants had recently completed a 36-month observational study of schizophrenia treatment under usual care conditions. Eligible participants included all adult patients in a defined geographic region who began the longitudinal study under treatment for recently documented DSM-IV diagnoses of schizophrenia, schizoaffective disorder, or schizophreniform disorder. For the longitudinal study, participants were randomly selected from treatment records at several regional public mental health clinics. Participants remained eligible even if they discontinued treatment. The sample for the study reported here comprised any individuals who at the completion of the longitudinal study were willing to enter a new study. The sample was closely comparable to the population of persons with psychotic disorders who were being served in the public sector in the Piedmont of North Carolina (3). Written informed consent was obtained according to a protocol approved by the institutional review board of Duke University Medical Center.
Instruments
Demographic information, including gender, race, marital status, age, and number of years of education, was obtained through self-report. Consumers were queried for their age at onset of their psychiatric disorder; whether they perceived finances, convenience, or trust as barriers to treatment; whether they perceived their neighborhood to be dangerous to live in; and whether they had ever been victims of physical or sexual abuse. Consumers were also asked whether they had committed any violent acts, including hitting others, or had used threats with weapons in the previous six months.
The symptom severity section of the Schizophrenia Outcomes Module baseline consumer assessment (23) was used to assess self-reported symptoms. On this instrument, respondents report the severity of symptoms of psychosis and depression during the previous week on a 4-point scale ranging from not at all bothered to greatly bothered. An overall symptom scale is calculated from the mean of all items (potential range, 0 to 33) and the subset of items related to depression (potential range, 0 to 9) (alpha=.88 for the current sample). Insight was assessed by using the Insight and Treatment Attitudes Questionnaire (ITAQ) (24), an 11-item scale (potential range, 0 to 22) that elicits respondents' views about their mental health problems and need for mental health treatment in the past, currently, and in the future (alpha=.82 for our sample).
To elicit their views on the etiology of schizophrenia, consumers were presented with a series of vignettes describing a hypothetical person with schizophrenia (25) and were asked whether the person's situation could be attributed to bad character, upbringing, God's will, a chemical imbalance in the brain, genetics, or stress. Each item was coded on a 4-point scale ranging from not at all likely to very likely. Responses attributing the illness to a chemical disorder, genetic vulnerability, or stress were summed and scored as an endorsement of a biopsychosocial model of illness (potential range, 3 to 12). Responses that attributed the cause to poor upbringing, bad character, or God's will were regarded as an endorsement of a nonmedical model view of illness (potential range, 3 to 12). Correlation between these scales was low (.115) and nonsignificant.
Respondents reported their experience with formal and informal forms of treatment mandates and pressures and were asked whether they had ever been on court-ordered outpatient commitment, had ever been subjected to involuntary hospitalization, had ever been required to obtain treatment as a result of legal or court-related requirements (to avoid having legal charges filed or serving time in jail), or had ever been required to stay in treatment or away from drugs and alcohol to retain housing, including nonofficial pressure from family members or others who may provide housing. Respondents were also asked whether they currently had a representative payee who managed their entitlements or other finances. With the exception of representative payeeship, few respondents were currently under legal mandates.
The participants were also asked whether they had been reminded or warned that noncompliance with medications or missing mental health appointments could result in hospitalization, involuntary commitment, notification of police, loss of spending money, or loss of housing. Responses to these questions were combined into dichotomous variables of "any" or "no" medication adherence or appointment adherence reminders.
The MacArthur Admission Experiences Scale, modified for outpatient use (26), was used to assess participants' experience of coercion in outpatient treatment. Scale items elicited participants' experiences of forced threats and other pressures to seek treatment. The scale includes 15 true or false items and is calculated as the sum of responses indicative of coercive experiences (potential range, 0 to 15) (alpha=.85 for our sample).
Several interview items concerning the fairness and effectiveness of coercion in motivating treatment adherence were used to elicit participants' overall appraisal of the effects of treatment mandates and pressures they had experienced. The index of fairness included summed responses to the following items: overall, the pressures or things people have done to try to get me into treatment or to stay in treatment were done by people who tried to be fair to me, were done for my own good, were not done out of real concern for me (reverse coded), or didn't make me feel respected as a person (reverse coded).
The index of effectiveness included summed responses to the following items: overall, the pressures or things people have done to try to get me into treatment or to stay in treatment made me more likely to keep appointments and take my medications, helped me get well and stay well, helped me gain more control over my life, or should be done again in the future.
Each item was rated on a 5-point scale ranging from strongly agree to strongly disagree. The summed scales for these two measures were coded so that higher scores indicated that the respondent viewed treatment mandates and pressures as fair (potential range, 4 to 20) (alpha=.71) and effective (potential range, 4 to 20) (alpha=.73).
Statistical methods
Two outcome variables for fairness and effectiveness were constructed from the eight questions relating to perceived benefits of treatment mandates. The bivariate magnitude of associations between the fairness and effectiveness measures and a series of putative predictive factors were estimated by using Spearman's rank-order correlation analysis. Multivariate associations were tested with ordinary least-squares regression procedures using the SAS 8.02 statistical package (27). For the ordinary least-squares regression analyses, to achieve initial variable reduction, candidate variables in one of four domains were tested by using backward stepwise selection procedures with the inclusion criterion set at p=.10. Each domain was tested separately with the effectiveness or fairness outcome measures.
After testing, variables that had been selected into the model from each domain were combined and resubjected to a second regression process without further variable selection procedures to determine a final model following model estimation procedures that have been discussed by several authors (28,29,30). Results are expressed in standardized regression or beta coefficients. Beta coefficients denote the increase in the dependent variable for each increase in a predictor variable expressed in standard deviation units. To ensure the robustness of this model, an additional model that included all domains simultaneously without selection procedures was estimated.
Results
As can be seen from Table 1, the study participants were predominantly single and African American, and the gender distribution was roughly equal. The average age of the participants was in the mid-40s. Although a majority had been victims of physical or sexual abuse at some time in their lives, only a minority perceived their current neighborhood as dangerous. Approximately a third of the participants reported at least one barrier to help seeking.
The participants on average reported an onset of illness before the age of 16 years, low levels of current symptoms, and low levels of recent violent behavior. About two-thirds of the participants had a lifetime history of involuntary hospital admission. The sample reported experiencing a lifetime average of three types of mandated treatment from the following list: involuntary hospitalization, involuntary outpatient commitment, representative payeeship, housing contingent on treatment adherence, and other criminal justice pressures.
The participants reported relatively low levels of perceived coercion on the MacArthur Admissions Experience Scale, modified for outpatient use, and had relatively high levels of insight into their illness, with most viewing themselves as ill and in need of treatment. Response scores (not shown) were dichotomized so that respondents who averaged a response of agree or strongly agree on either effectiveness or fairness respectively were regarded as endorsing those items (nondichotomized effectiveness mean, 15.7±2.82; fairness mean, 15.1±2.77). According to these criteria, approximately 62 percent of the participants (64 participants) regarded mandates as effective and 55 percent (57 participants) regarded them as fair.
Table 2 presents rank correlations showing the magnitude and statistical significance of bivariate associations between the appraisal of fairness and effectiveness and a series of putative predictive factors, grouped into several domains. In the social environment domain, participants who perceived their daily surroundings as dangerous tended to have lower scores on the indexes of effectiveness and fairness of treatment mandates. Perceptions of fairness also diminished as the total number of perceived barriers to care increased.
In the clinical domain, higher total numbers of symptoms were associated with lower perceived effectiveness and fairness of treatment mandates (marginally so in the case of fairness). No other clinical variables were significantly associated with perceived effectiveness and fairness of mandates.
In the domain of coercive experiences, higher scores on the MacArthur Admissions Experience Scale were associated with significantly lower scores on the indexes of perceived effectiveness of treatment mandates and pressures. However, the number of reported actual episodes of mandated treatment was not significantly associated with perceived fairness and effectiveness of mandates.
In the domain of views of illness, higher scores on the ITAQ and endorsement of items consistent with a biopsychosocial etiology of mental illness were significantly associated with greater perceived effectiveness of treatment mandates and pressures and greater perceived fairness of these pressures. No association was found between endorsement of a nonmedical model of disease etiology and perceived fairness or perceived effectiveness and mandates.
Multivariate associations were tested by using ordinary least-squares regression procedures as described above. The results are summarized in Table 3. Participants who endorsed the effectiveness of treatment mandates and pressures were significantly less likely to report that they lived in a dangerous environment, reported fewer total symptoms, were more likely to endorse a biopsychosocial model of disease etiology, and had higher levels of insight. Each of these four items remained statistically significant when combined in a final model, which suggests that each contributed independently to the association between predictors and the perceived effectiveness of treatment mandates and pressures.
Lower scores on perceived fairness of treatment mandates and pressures were associated with significantly more barriers to care and with higher levels of reported symptoms. Higher perceived coercion, as measured on the MacArthur Admissions Experiences Scale, was also associated with lower perceived fairness. In contrast, consumers with higher levels of insight were significantly more likely to perceive that pressures had been applied fairly and in good faith. In contrast to the bivariate results, endorsement of the biopsychosocial model of illness was marginally associated with more favorable views of treatment mandates. When the latter five selected variables were combined in a final model, only higher levels of insight remained significant as independent predictors of perceived fairness, although the total number of symptoms was marginally significant.
The two outcome variables—fairness and effectiveness—were themselves highly correlated (r=.53). Not surprisingly, consumers who in retrospect associated treatment pressure with improved outcomes also perceived such pressure to have been fair.
Discussion
A surprising 62 percent and 55 percent of consumers with schizophrenia in this cohort endorsed the effectiveness and fairness, respectively, of treatment mandates and related adherence pressures. Consumers who endorsed the effectiveness of treatment mandates tended to accept a biopsychosocial model of the etiology of mental illness, were more likely to view themselves as ill and in need of treatment, and reported fewer psychiatric symptoms compared with their counterparts who considered mandated treatment to be unfair and ineffective.
Of note, we found a strong and significant correlation between perceived effectiveness and fairness of mandates and informal pressures to adhere to treatment. Consumers' appraisal of the fairness of mandates was largely dependent on the mandates' perceived effectiveness. Simply put, in the view of consumers, if mandates do not work, they cannot be fair. However, the converse may also be true: consumers who regard mandates as unfair may also regard them as unlikely to be effective. Consumers who regard their environments as dangerous, who report higher levels of symptoms, and who reject a biopsychosocial view of illness and deny their own illnesses also tend to reject mandates, viewing them as ineffective and unfair.
Actual reported experiences with treatment mandates, coercion, or informal pressures to adhere to treatment played little role in the appraisal of mandates in general. However, it is possible that too few consumers in this study had had recent and salient experiences with mandates to enable any definitive analyses of these attitudes. These results suggest that psychoeducational treatment approaches that attempt to improve understanding of the biopsychosocial nature of these illnesses, when combined with effective symptomatic treatment, may decrease resistance to treatment, including treatment mandates when needed.
The analysis was limited in several important ways. In a cross-sectional survey using a single interview, causal ordering of variables is difficult to determine. As a further caveat, the respondents with psychoses in our study were selected from an established longitudinal research cohort of persons who, at least initially, were in treatment and were willing to consent to participate in a new study. The views of these participants may not be representative of persons who refuse treatment or research participation. Thus the generalizability of the findings is limited, especially generalizability to persons who are more acutely ill. Greater variation in scores on predictor variables may have yielded additional significant relationships between these predictors and appraisals of fairness and effectiveness. As a consequence, the results of this study may understate important relationships. A recently completed multisite study by the MacArthur Foundation Research Network on Mandated Community Treatment will offer an opportunity to replicate these findings (31).
Conclusions
Consumers with psychotic illnesses who regard schizophrenia as a biopsychosocial illness and view themselves as ill seem also to believe that they themselves benefit from a range of formal and informal sanctions regarding treatment adherence and that these sanctions generally are applied in their best interest and out of concern for their well-being. Those who reject this view also tend to reject a view of themselves as ill and in need of treatment. Because this was not a prevalence study, the results do not speak to the prevalence of these views among consumers at large but point to an important relationship between these attitudes.
The authors are affiliated with the services effectiveness program in the department of psychiatry and behavioral sciences, Box 3173, Duke University Medical Center, Durham, North Carolina 27710 (e-mail, [email protected]).
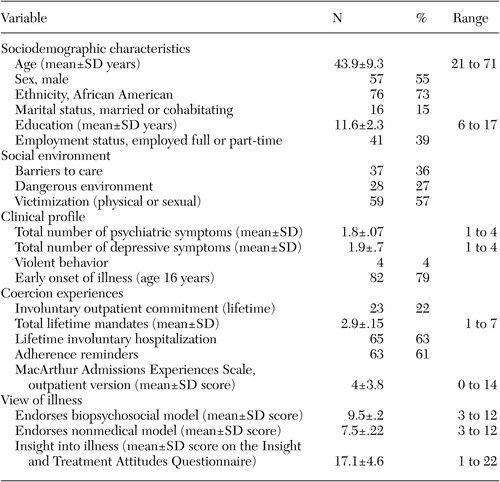 |
Table 1. Sociodemographic and clinical characteristics of a sample of 104 consumers intreatment for schizophrenia and related disorders
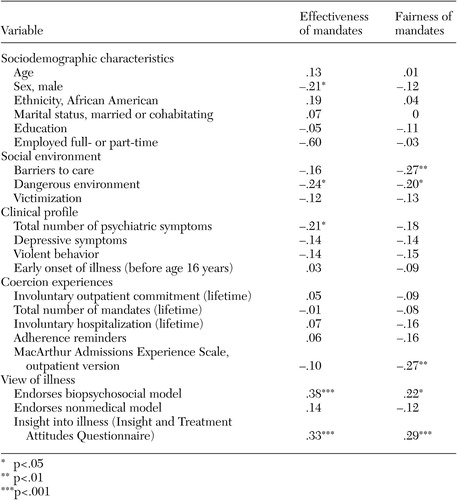 |
Table 2. Associations (r) between sociodemographic and clinical characteristics associated with consumers' appraisal of the effectiveness and fairness of treatment mandates
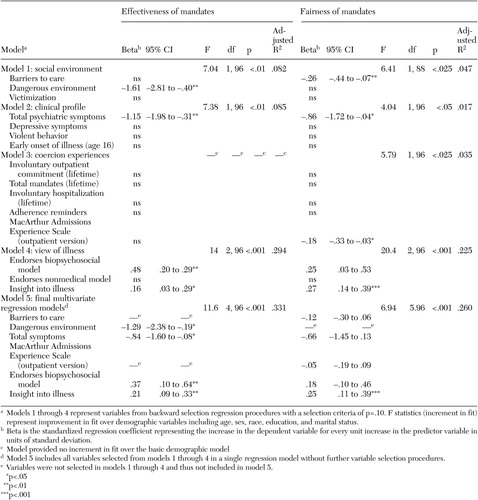 |
Table 3. Multivariate regression models of associations between sociodemographic and clinical predictors of consumers' appraisals of the effectiveness and fairness of treatment mandates
1. Monahan J, Bonnie R, Appelbaum R, et al: Mandated community treatment: beyond outpatient commitment. Psychiatric Services 52:1198–1205, 2001Link, Google Scholar
2. Swartz MS, Swanson JW, Monahan J: Endorsement of personal benefit of outpatient commitment among persons with severe mental illness. Psychology, Public Policy, and Law 9:70–93, 2003Crossref, Medline, Google Scholar
3. Swartz MS, Swanson JW, Wagner HR, et al: Assessment of four stakeholder groups' preferences concerning outpatient commitment for persons with schizophrenia. American Journal of Psychiatry 6:1139–1146, 2003Link, Google Scholar
4. Swanson JW, Swartz MS, Elbogen E, et al: Effects of involuntary outpatient commitment on subjective quality of life in persons with severe mental illness. Behavioral Sciences and the Law 21:473–491, 2003Crossref, Medline, Google Scholar
5. Gerbasi JD, Bonnie RB, Binder RL: Resource document on mandatory outpatient treatment. Journal of the American Academy of Psychiatry and the Law 28:127–144, 2000Medline, Google Scholar
6. Stefan S: Preventive commitment: the concept and its pitfalls. Mental and Physical Disability Law Reporter 11:288–302, 1987Google Scholar
7. Allen M, Smith VF: Opening Pandora's box: the practical and legal dangers of involuntary outpatient commitment. Psychiatric Services 52:342–346, 2001Link, Google Scholar
8. Stein LI, Diamond RJ: A "systems"-based alternative to mandatory outpatient treatment. Journal of the American Academy of Psychiatry and the Law 28:159–164, 2000Medline, Google Scholar
9. Mattison E: The law of unintended consequences. Journal of the American Academy of Psychiatry and the Law 28:154–158, 2000Medline, Google Scholar
10. Hoge MA, Grottole E: The case against outpatient commitment. Journal of the American Academy of Psychiatry and the Law 28:165–170, 2000Medline, Google Scholar
11. Campbell J, Schraiber R: The Well-Being Project: Mental Health Clients Speak for Themselves. Sacramento, Calif, California Network of Mental Health Clients, 1989Google Scholar
12. Swartz MS, Swanson J, Hannon M: Does fear of coercion keep people away from mental health treatment? Behavioral Sciences and the Law 21:459–472, 2003Google Scholar
13. Monahan J, Hoge SK, Lidz C, et al: Coercion and commitment: understanding involuntary mental hospital admission. International Journal of Law and Psychiatry 18:249–263, 1995Crossref, Medline, Google Scholar
14. Lidz CW, Hoge SK, Gardner W, et al: Perceived coercion in mental hospital admission: pressures and process. Archives of General Psychiatry 52:1034–1039, 1995Crossref, Medline, Google Scholar
15. Lind E, Kanfer R, Early P: Voice, control, and procedural justice: instrumental and noninstrumental concerns in fairness judgments. Journal of Personality and Social Psychology 20:1952–959, 1990Google Scholar
16. Lind E, Tyler T: The Social Psychology of Procedural Justice. New York, Plenum, 1988Google Scholar
17. Bennett NS, Lidz CW, Monahan J, et al: Inclusion, motivation, and good faith: the morality of coercion in mental hospital admission. Behavioral Science and Law 11:295–306, 1993Crossref, Medline, Google Scholar
18. Kaltiala-Heino R: Involuntary psychiatric treatment: a range of patients' attitudes. Nordic Journal of Psychiatry 50:27–34, 1996Crossref, Google Scholar
19. Kjellin L, Nilstun T: Medical and social paternalism: regulation of and attitudes towards compulsory psychiatric care. Acta Psychiatrica Scandinavica 88:415–419, 1993Crossref, Medline, Google Scholar
20. Kjellin L, Andersson K, Candefjord I, et al: Ethical benefits and costs of coercion in short-term inpatient psychiatric care. Psychiatric Services 48:1567–1570, 1997Link, Google Scholar
21. Swartz MS, Swanson JW, Hiday VA, et al: A randomized controlled trial of outpatient commitment in North Carolina. Psychiatric Services 52:325–329, 2001Link, Google Scholar
22. Steadman HJ, Gounis K, Dennis D, et al: Assessing the New York City outpatient commitment pilot program. Psychiatric Services 52:330–336, 2001Link, Google Scholar
23. Cuffel BJ, Fischer EP, Owen RR, Jr, et al: An instrument for the measurement of care for schizophrenia: issues in development and implementations. Evaluation and the Health Professions 20:96–108, 1997Crossref, Medline, Google Scholar
24. McEvoy JP, Apperson LJ, Appelbaum PS, et al: Insight in schizophrenia: its relationship to acute psychopathology. Journal of Nervous and Mental Disease 177:43–47, 1989Crossref, Medline, Google Scholar
25. Pescosolido BA, Monahan J, Link BG, et al: The public's view of the competence, dangerousness, and need for legal coercion among persons with mental illness. American Journal of Public Health 89:1339–1345, 1999Crossref, Medline, Google Scholar
26. Swartz MS, Wagner HR, Swanson JW, et al: The perceived coerciveness of involuntary outpatient commitment: findings from an experimental study. Journal of the American Academy of Psychiatry and the Law 30:207–217, 2002Medline, Google Scholar
27. Joyner SP: SAS User's Guide. Cary, NC, SAS Institute, 1985Google Scholar
28. Pedhazur EJ: Multiple Regression in Behavioral Research: Explanation and Prediction. Fort Worth, Tex, Holt, Rinehart & Winston, 1982Google Scholar
29. Mosteller FM, Tukey JW: Data Analysis and Regression: A Second Course in Statistics. Reading, Pa, Addison-Wesly, 1977Google Scholar
30. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, Wiley, 1989Google Scholar
31. Monahan J, Swartz MS, Bonnie R: Mandated treatment in the community for people with mental disorders. Health Affairs 22(5):28–38, 2003Google Scholar



