Trends in Acute Psychiatric Inpatient Care in Massachusetts
Abstract
This report presents the preliminary results of a longitudinal study of acute psychiatric hospitalization in the Commonwealth of Massachusetts for fiscal years 1994 to 2000. The study was a secondary analysis of data obtained through the Commonwealth's mandated case-mix reporting system, covering 42 acute psychiatric facilities and 119,284 patients. Results include a 58.4 percent increase in the patient population, accompanied by declines in both length of stay and readmission rates; increases in the number of diagnoses of depression and in the number of patient deaths; and shifts to an older population increasingly supported by Medicaid and Medicare, especially managed care programs.
The continuing deinstitutionalization of county and state psychiatric patients, as well as similar trends in the Department of Veterans Affairs (VA) (1), have been associated with the privatization of mental health care delivery, including growth in the number of private acute hospitals (2). Yet the expansion of managed health care in both the commercial and public sectors has been reported to have diminished the availability of even acute psychiatric care (2). A federal study indicated that, just as there was a proliferation of mental health organizations between 1970 and 1998, the total number of inpatient and residential psychiatric beds has diminished by about half, from 525,878 to 261,903. Yet the number of beds in general hospitals has more than doubled, from 22,394 to 54,266 (3). These mixed reports reflect the difficulties in tracking services as a result of their increasingly privatized and decentralized nature (4).
However, several nations and states have developed mandated case-mix reporting systems that require that health care facilities provide the state with information about each episode of care, typically inpatient care (5). One of the better developed systems is that of Massachusetts, which annually requires reports on each discharge from the state's acute care health and mental health facilities. This system has been particularly important since its inception in 1992. Massachusetts has taken a lead in implementing a statewide managed care carve-out program to control health care costs, at about the same time that its Department of Mental Health closed several facilities.
This report presents initial results from a longitudinal study based on data from the Commonwealth's case-mix reporting system. It aims to describe trends in the state's 42 acute psychiatric facilities, including readmission rates, and to answer questions about changes in the demographic and diagnostic mix of patients and their discharge dispositions, including changes in the proportion covered under both private insurance and public managed care programs.
Methods
This trend study of a state population of psychiatric patients used a secondary analysis of data collected by the Massachusetts Division of Health Care Finance and Policy (6). The data consist of seven annual data files for fiscal years 1994 to 2000, each with about 750,000 discharge records from 85 medical facilities throughout Massachusetts, including 45 psychiatric units. Not available are those from the VA, single-purpose psychiatric hospitals, state hospitals, or residential services. In addition to information about service use, demographic characteristics, discharge disposition, diagnoses, and insurance, the database includes an encrypted Social Security number that permits the merging of these files and the tracking of individual patients across hospitals and years. The system is considered to be one of the best among the states; details of its data collection and cleaning protocols and tests of its reliability, which have been shown to be moderate to good, have been published elsewhere (6,7,8). Because this was a mandated population enumeration, sampling was not employed.
Results
The total number of facilities remained in the range of 42 to 45 during the period 1994 to 2000, while the mean daily census of the facilities increased by more than a third (35 percent), from 17.5 to 23.6, as can be seen in Table 1. This increase resulted from a 58.4 percent increase in the number of patients seen, which stood at 29,072 in 2000. Although the mean number of episodes per patient each year was virtually unchanged, at 1.39, the mean length of stay declined by about a sixth (-14.8 percent), from 10.6 days in 1994 to nine days in 2000. As a result, the number of bed days increased by less than did the number of patients but still at the considerable level of 35 percent over seven years. During this same period, 90-day readmission rates declined by a fifth (-19 percent), from 20.5 percent in 1994 to 16.6 percent in 2000, despite declining length of stay.
The growth in the patient population appears to be unrelated to the population's gender composition, which remained substantially the same over the seven years (42.6 to 45.3 percent male). However, growth in the proportion of Asian or Pacific Islander (246.4 percent) and Hispanic (221.1 percent) persons has been considerable, and the number of black patients increased moderately (by 13.7 percent). The number of white patients increased substantially, from 15,621 in 1994 to 23,716 in 2000; however, their relative proportion of the total population declined. One of the most dramatic trends was the increase in the patients' mean age, from 42.4 to 50.1 years. Although the size of most of the diagnostic groups examined increased in absolute terms, given the growing patient population, the size of all but one of these groups declined relative to the total population—the exception was the group of patients with depressive disorders, which more than tripled from 542, or 2.9 percent of the population, in 1994 to 1,668, or 5.7 percent, in 2000. Nonetheless, affective disorder was the most prevalent diagnosis, accounting for 44.1 percent of patients by 2000.
Concurrent with the increase in age, there was also an increase in the absolute number of deaths in these acute units, from 14 in 1994 to 214 in 2000. This increase was associated with a crude death rate of 736 per 100,000 in the year 2000, compared with 877.5 in 1999 (9). A decline was also seen in the relative proportion of patients who were sent home without a referral and discharged against medical advice. However, despite a relative improvement in the provision of discharge referrals, 70.3 percent of patients were sent home in 2000 without a recorded referral or transfer or were discharged against medical advice.
The aging of the patient population and the growth in the number of patients took place at the same time as did a shift away from commercial insurance as a primary form of payment (from 29.3 percent to 25.9 percent of the total). In contrast, public insurance—in particular, the state's Medicare and Medicaid managed care programs—saw a six-fold increase (588.7 percent), from supporting 689 (3.8 percent) of the patients in 1994 to 4,745 (16.3 percent) of the patients in the year 2000. Despite contrary state plans, the number of patients who received free care more than doubled (116.1 percent), increasing from 502 (2.7 percent of the total) in 1994 to 1,085 (3.7 percent) in 2000.
Discussion and conclusions
The results of this study suggest that, given the substantial increases in the use of acute psychiatric care in Massachusetts in the 1990s, hospitals have not kept up with increasing demand. One interpretation is that hospitals have progressively shortened the length of stay of these patients to control daily census. Another interpretation is that the increases arise out of providers' responses to changing reimbursement incentives. Associated with this growth has been the increased demand for care for older adults, many from medical and nursing facilities. These results pertain to the Commonwealth's acute medical facilities and are not generalizable to units in the VA, residential services, specialized psychiatric hospitals, or state mental hospitals.
Some of the surge in the aging population occurred between 1999 and 2000, resulting from transfers from New York state nursing homes by the Sunbridge Corporation as a result of favorable reimbursement rates (10). These out-of-state transfers have been largely exempt from review by the 1987 Omnibus Budget Reconciliation Act's (OBRA's) prescreening protocols (PASARR), which were designed to minimize inappropriate transfers between nursing homes and psychiatric units (memo, Vautour K, 2001). The increasing age and associated increase in the death rate may also reflect declines in supported housing and availability of nursing home placements, which has made hospitalization a placement of last resort.
These findings highlight the need to improve screening and assessment techniques for acute psychiatric care to minimize the decline in length of stay that appears to be driven more by financial and larger systemic conditions than by clinical considerations. This is of particular importance for aged persons, given the circumvention of OBRA screening protocols and resulting increase in nursing home transfers.
Dr. Hudson is a professor and the chairperson at the School of Social Work of Salem State College, 352 Lafayette Street, Salem, Massachusetts 01970 (e-mail, [email protected]). At the time of this study he was visiting Fulbright professor in the department of social studies of the City University of Hong Kong.
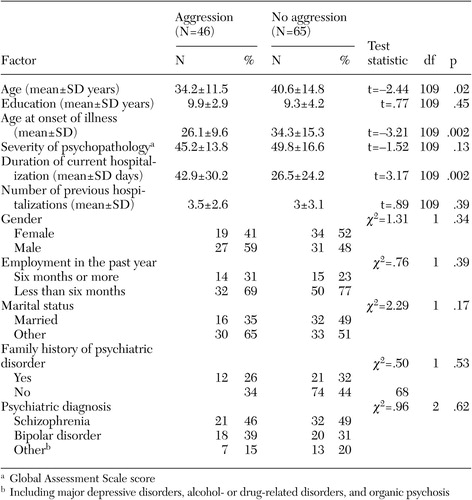 |
Table 1. Trends in acute psychiatric hospitalization in Massachusetts, fiscal years 1994 to 2000 (N=119,284)
1. Desai MM, Rosenheck RA: Trends in discharge disposition, mortality, and service use among long-stay psychiatric patients in the 1990s. Psychiatric Services 54:542–548, 2003Link, Google Scholar
2. Dorwart RA, Schlesinger M, Davidson H, et al: A national study of psychiatric hospital care. American Journal of Psychiatry 148:204–210, 1991Abstract, Google Scholar
3. Manderscheid RW, Atay JE, Hernández-Cartagena M, et al: Highlights of organized mental health services in 1998 and major national and state trends, in Mental Health, United States, 2000. Edited by Manderscheid RW, Henderson MJ. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2001Google Scholar
4. Geller JL, Fisher WH, McDermeit M, et al: The effects of public managed care on patterns of intensive use of inpatient psychiatric services. Psychiatric Services 49:327–332, 1998Link, Google Scholar
5. Lichtenberg P, Kaplan Z, Grinshpoon A, et al: The goals and limitations of Israel's psychiatric case register. Psychiatric Services 50:1043–1048, 1999Link, Google Scholar
6. Hospital Case Mix and Charge Data Base Documentation Manuals, Fiscal Years 1994 Through 2000. Boston, Massachusetts Division of Health Care Finance and PolicyGoogle Scholar
7. Hudson CG: Changing patterns of acute psychiatric hospitalization under a public managed care program. Journal of Sociology and Social Welfare 28:141–176, 2001Google Scholar
8. Case Mix Payer Validation Report. Boston, Massachusetts Division of Health Care Finance and Policy, May 1998Google Scholar
9. Mortality Report, 2000. Boston, Massachusetts Department of Mental Health, 2000Google Scholar



