Cognitive and Symptom Predictors of Work Outcomes for Clients With Schizophrenia in Supported Employment
Abstract
OBJECTIVES: This study examined the relationships of measures of cognitive functioning and psychiatric symptoms with work outcomes and use of vocational services for clients with schizophrenia in a supported employment program. METHODS: Thirty clients who were newly enrolled in a supported employment program were evaluated with cognitive and symptom measures at program entry and two years later. The clients' amounts of competitive work, wages earned, on-job support, and contact with employment specialists during the two-year follow-up period were documented. RESULTS: Predictors of clients' work outcomes included previous work history, amount of government entitlement income received, severity of negative symptoms, involvement in sheltered work activity at baseline, and level of cognitive functioning, including scores on measures of executive functioning and verbal learning and memory. The amounts of on-job support and contact with employment specialists were predicted by the cognitive domains of executive functioning, verbal learning, attention, and psychomotor speed as well as by the severity of psychotic symptoms. CONCLUSIONS: Clients with schizophrenia who have higher levels of cognitive impairment may require greater amounts of vocational support than those with lower levels of impairment. A variety of rehabilitation strategies may be required to improve vocational outcomes and reduce the amount of supported employment services needed by clients with schizophrenia.
Several studies have demonstrated that supported employment for persons with severe mental illness is effective in improving clients' competitive work outcomes (1,2,3,4,5). However, despite the overall success of supported employment programs, many clients who are enrolled in such programs work infrequently or not at all. A review of studies of supported employment programs found that between one-third and two-thirds of clients worked minimally or not at all (6). Additional research is needed to identify the client characteristics that contribute to response to supported employment programs. The identification of such characteristics could lead to changes in the delivery of supported employment services or to the provision of ancillary interventions designed to address characteristics associated with poor response.
Prospective research involving clients with severe mental illness has examined the associations of clinical symptoms and cognitive functioning with employment outcomes. Both positive and negative symptoms have been found to predict employment outcomes in some studies (7,8) but not in others (9,10,11,12). Other studies have suggested that the level of cognitive impairment is predictive of vocational outcomes (13,14,15).
Although previous research has indicated that symptoms and cognitive functioning are related to employment outcomes for clients with severe mental illness, few studies have examined the relationship between these client factors and outcomes in supported employment programs. In a two-year study of supported employment, Mueser and colleagues (9) examined the relationship of positive, negative, and cognitive symptoms as assessed by the Positive and Negative Syndrome Scale (16) with competitive work outcomes for clients with schizophrenia or schizoaffective disorder. The authors found that negative symptoms predicted employment outcomes but that positive and cognitive symptoms did not. A limitation of this study was that cognitive functioning was assessed by using a clinical rating rather than by using a neuropsychological battery. Previous research has indicated that less than half the variance in neuropsychological performance is captured by clinical rating scales for cognitive functioning (17), suggesting that performance-based measures of cognitive impairment might be more strongly related to vocational outcome.
The study reported here was conducted to examine the relationship of cognitive functioning, assessed by a neuropsychological battery, and clinical symptoms with competitive employment outcomes for clients with schizophrenia or schizoaffective disorders in a supported employment program. Cognitive functioning and clinical symptoms were measured at the clients' entry into the program and at two years after enrollment. Comprehensive employment outcomes were assessed over the two-year period. In addition, data on the use of supported employment services were evaluated in relation to clinical symptoms and cognitive functioning. We predicted that greater negative symptoms and cognitive impairment, particularly in executive functioning and verbal learning and memory, would be associated with poorer work outcomes and more intensive job support.
Methods
Subjects
The study participants were 30 clients with schizophrenia (N=16) or schizoaffective disorder (N=14) who were receiving outpatient services at a state hospital. The study protocol was approved by the hospital's institutional review board. After the clients received a full explanation of the study procedures and were given a capacity evaluation by a psychiatrist who was not part of the research team, they provided written informed consent to participate in the study. The clients' diagnoses were made by a member of the research team on the basis of clinical interviews with the Comprehensive Assessment of Symptoms and History (18) and information from the clients' charts.
The characteristics of the study participants are summarized in Table 1. Eight clients (27 percent) had a work history, defined as a minimum of 12 consecutive months of full-time competitive employment. At the time of referral to the supported employment program, none of the clients were working competitively, and 16 (53 percent) were participating in a sheltered work program in which the mean±SD number of hours worked was 10.6±6.4 a week.
Supported employment program
The clients were either self-referred to the supported employment program or referred by their case manager or by another member of the treatment team. The program provided at the hospital's outpatient clinics was based on the individual placement and support employment model (19). The only criterion for program participation was that the client requested competitive work. At entry into the program, each client was assigned an employment specialist who provided all components of supported employment, including assessment, assistance with job search, and job support. The employment specialists' duties consisted only of providing supported employment services, and they each had a caseload of about 20 clients. Each employment specialist functioned as a member of the client's interdisciplinary treatment team. They attended all treatment team meetings and updated team members on the client's vocational activities.
A client's job search commenced after a brief assessment that included identification of the client's job preferences. No prevocational skills training was provided. After the client obtained employment, the supported employment program provided follow-along supports as needed for an unlimited time, including both on- and off-site support, depending on the client's needs or preferences.
Assessments
The Positive and Negative Syndrome Scale (16) was used to assess the severity of psychiatric symptoms. The predictor variables assessed in relation to clients' work outcomes were measured by using five subscales based on the factor structure of the Positive and Negative Syndrome Scale reported by White and associates (20). The five subscales measured positive, negative, activation, dysphoria, and autistic preoccupation symptoms.
Premorbid academic achievement was assessed with the Wide Range Achievement Test 3 reading subtest (21), which measures word recognition and reading performance. Performance on this test has been shown to be relatively well preserved among persons who develop schizophrenia (22). The Wide Range Achievement Test 3 provides a total score for words read correctly that is converted to a grade-equivalent score.
Immediate attention was measured with the digit span test of the Weschler Adult Intelligence Scale- Revised (23). Study participants are given a number string and asked to repeat it in the same order of presentation (digit span forward) or backward (digit span backward). The score consists of the numbers of digits correctly repeated in each condition.
Psychomotor speed was measured with the Trail Making Test, Part A and Part B (24). Part A is a timed measure of visual scanning ability and psychomotor speed that requires the subject to connect numbers in order. The score is the time, in seconds, required to complete the task. Part B of the Trail Making Test is similar to Part A but is more challenging because it requires subjects to connect consecutively numbered and lettered circles by alternating between the two sequences.
Executive functioning was assessed with the Wisconsin Card Sorting Test (25), a commonly used test that measures cognitive flexibility and problem-solving skills. Participants are asked to match a series of cards to a set of four target stimuli, which are also cards. They are provided with feedback on each item after they sort each of the cards. After they determine one of the correct dimensions, referred to as "categories," ten correct responses are required before the category is shifted to the next one. Continued matching to a category that is no longer correct is considered a perseverative error. The variables of interest were the number of categories achieved and the percentage of perseverative errors.
Verbal learning and memory were assessed with the California Verbal Learning Test (26). The California Verbal Learning Test involves the repeated presentation of a word list that consists of names of common items that are semantically related to four conceptual categories—food, clothing, spices, and tools. The variables of interest were acquisition, which is determined by the total number of words recalled in the most productive of five learning trials minus the total number of words recalled in the first trial, and retention, which is determined by the total number of words recalled in the most productive of five learning trials minus the total number of words recalled in a free-recall condition after a delay of 20 minutes.
Results
In this section we first provide a brief description of the work outcomes for clients in the supported employment program. Next we present the analysis of demographic and other background predictors of work outcomes. We then examine the degree of change in clients' symptom severity and cognitive functioning over the two-year follow-up period. Next we present the analysis of symptom and cognitive predictors of work outcomes. Finally, we examine the relationship of symptoms and cognitive functioning with utilization of supported employment services by the clients who obtained competitive employment.
Work outcomes
Fifteen clients (50 percent) worked competitively during the two-year follow-up period. For the clients who worked, the mean±SD number of hours worked competitively during the two-year period was 867±843, with a range from four to 2,800 hours. The mean amount of wages earned over the two years was $6,007± $5,770, with a range from $20 to $16,800, and the mean hourly wage was $7.20±$1.60, with a range from $5.00 to $10.49. The mean length of competitive employment (cumulative) was 140±131 days, with a range from one to 361 days. The clients held a mean of 1.4±.63 jobs during the two-year period, with a range from one to three jobs.
Demographic and background predictors of work outcomes
For clients who obtained competitive employment, we examined two aspects of work outcome in the two-year period—the total number of hours worked and the total amount of wages earned. Pearson correlations were computed to examine the relationships between work outcomes and the continuous demographic and background variables, including age, number of years of education, duration of illness, age at first hospitalization, age at last hospitalization, amount of entitlement income per month, Wide Range Achievement Test 3 reading subtest score, and amount of involvement in sheltered work. T tests were used to examine the relationships between work outcomes and categorical variables such as gender, diagnosis, Caucasian ethnicity versus other ethnicity, presence or absence of a history of one or more years of continuous competitive work, and use of typical antipsychotic medication versus use of novel antipsychotic medication.
Greater monthly entitlement income was associated with fewer hours worked (r=.54 p<.05) and smaller amounts of wages earned (r=.48, p<.05). Clients who had a history of one or more years of continuous competitive employment (N=8) worked more hours (mean±SD=1,624±897 hours) and earned more wages (mean±SD=$10,634±$2,167) than clients who had previously worked less than one year (mean±SD=489±208 hours and mean±SD=$3,693±$1,532) (t=3.5, df=28, p<.01; and t=2.7, df=28, p<.05, respectively). Working more hours in sheltered work at study entry was associated with working more hours competitively (r=.94, p<.001) and with earning more wages (r=.88, p<.001) during the two-year follow-up period.
Changes in symptoms and cognitive functioning
To evaluate whether symptoms or cognitive functioning changed significantly in the group as a whole over the two-year follow-up period, paired t tests were computed to compare the scores on the study measures from the baseline and two-year assessments. None of the t tests were statistically significant, indicating that neither the level of symptoms nor the level of cognitive functioning increased or decreased uniformly over the follow-up period.
The stability of these measures was examined by comparing the scores from the baseline and two-year assessments with use of Pearson correlation. All the correlations were significant, with r values ranging from .40, for the California Verbal Learning Test retention score, to .82, for the Wisconsin Card Sorting Test percent perseveration score (Table 2).
Thus the symptom and cognitive measures demonstrated moderate to high stability over the two-year period. Given the reliability of these measures over the two-year period, we computed mean scores for each measure by using the baseline and two-year scores to provide an index of symptom severity and cognitive functioning over the entire two-year period of the client's participation in the supported employment program.
Symptom and cognitive predictors of work outcomes
To examine whether symptoms and cognitive functioning at baseline and follow-up were related to work outcomes, the baseline score and the mean of the baseline and follow-up scores for the symptom and cognitive measures were examined for correlations with the cumulative amounts of hours worked and wages earned over the two-year follow-up period. Because we hypothesized that higher symptom scores and higher levels of cognitive impairment would be associated with poorer work outcomes, one-tailed significance tests were used. The results of these analyses are summarized in Table 2.
Baseline and mean measures indicating better executive functioning (Wisconsin Card Sorting Test scores) and lower levels of negative symptoms (Positive and Negative Symptom Scale scores) were associated with more wages earned and more hours worked. Higher baseline and mean learning scores (California Verbal Learning Test acquisition scores) were associated with more hours worked.
Symptom and cognitive predictors of service use
Of the 15 clients who obtained competitive employment, 14 received ongoing supported employment services during the study period. To evaluate whether symptoms and cognitive functioning were related to the amount of supported employment services provided to these clients, two measures of support services were examined—the number of hours of on-job support provided per hour of competitive employment worked and the number of contacts between the client and the employment specialist, including face-to-face and telephone contacts. Correlations were computed to examine the relationship between the two measures of use of job services and the measures of symptoms and cognitive functioning at baseline and between the job services use measures and the means of the baseline and two-year scores on the measures of symptoms and cognitive functioning. The results of these analyses are summarized in Table 3.
Measures indicating better executive functioning (Wisconsin Card Sorting Test), better attention (digit span forward), and better psychomotor speed (Trail Making Test) were associated with fewer hours of on-job supports and fewer contacts. A higher mean score on the measure of learning (the California Verbal Learning and Memory Test, acquisition subscale) was associated with fewer hours of on-job supports, and a higher level of positive symptoms (Positive and Negative Syndrome Scale) was associated with more hours of on-job supports and more contacts.
Discussion and conclusions
The work outcomes of clients participating in this supported employment program, including the percentage of clients who worked as well as the number of hours worked and the amount of wages earned, were comparable to those of clients in other supported employment programs (2,4,27), suggesting that the program studied was representative of supported employment programs. The clients' symptoms and cognitive functioning did not change significantly over the two-year study period, with all the symptom and cognitive domains that were measured showing moderate to high stability (Table 2). The stability of the symptoms and cognitive functioning of the clients in this sample is consistent with the findings of other longitudinal studies of schizophrenia (28,29) and suggests that the symptoms and domains of cognitive functioning measured in this study are enduring aspects of the illness. The adequate stability over time of the measures in this study permitted the use of the means of the baseline and two-year scores to reflect the clients' levels of symptoms and cognitive functioning during the overall study period.
Symptoms and cognitive functioning were predictive of work outcomes. Specifically, and as reported in other studies (10,15), negative symptoms were predictive of work outcomes. Furthermore, several measures of cognitive functioning, including the Wisconsin Card Sorting Test and the California Verbal Learning Test, predicted work outcomes. Other researchers have suggested the importance of executive functioning, as measured by the Wisconsin Card Sorting Test, and of verbal learning and memory for the functional outcomes of patients with schizophrenia (30), particularly for employment outcomes (13,31). The findings reported here are consistent with earlier findings and extend them to the prediction of work outcomes for clients in a supported employment program. Problem-solving skills and learning and memory would be expected to be related to work outcomes, because adequate job performance relies to a great extent on these cognitive domains.
Symptoms and cognitive functioning also predicted receipt of supported employment services, but a different pattern of relationships emerged. In contrast to the analysis of work outcomes, in which negative symptoms predicted outcomes, positive symptoms but not negative symptoms predicted the number of hours of work support received and the number of contacts with employment specialists. Compared with clients who have more severe negative symptoms, those who have more severe positive symptoms may require closer monitoring, including more frequent prompts and more redirection, to sustain acceptable job performance.
The areas of cognitive functioning that were predictive of the amount of job supports included areas that were also predictive of work outcomes, such as executive functioning and learning, but did not include memory. Other cognitive domains associated with amount of job support included psychomotor speed and attention. Impairments in problem-solving skills, in the ability to pay attention, and in the ability to learn new information may be reflected in difficulties in learning job tasks and in independent problem solving on the job. Clients with those impairments required more help from employment specialists. Impairment of memory appears not to have led to problems on the job that required a compensatory increase in job supports. To our knowledge, these data are the first to address the relationship between job supports and client characteristics.
Cognitive factors appear to be related to employment outcomes as well as to use of supported employment services, with executive functioning predicting both work outcomes and service use. Cognitive rehabilitation techniques that specifically target executive functioning (32,33,34) hold promise of improving work outcomes and reducing the need for job support services. However, whereas executive functioning predicted both work and service outcomes, verbal learning was associated only with work outcomes, and attention and psychomotor speed, as measured by the Trail Making Test, Part A, were predictive only of service use. These findings suggest that clients with problems related to job maintenance may need different cognitive rehabilitation interventions than those with extensive use of job supports.
Like cognitive functioning, clinical symptoms were differentially related to work outcomes and service use. Poorer work outcomes were predicted by more severe negative symptoms, and more service use was predicted by more severe positive symptoms. The fact that positive symptoms were associated with the need for more services suggests that adjunctive treatment for psychosis, such as cognitive-behavioral therapy (35), could reduce the amount of support required for these clients to sustain work. Thus a variety of interventions may be required to improve vocational outcomes for clients receiving supported employment services and to reduce the number and extent of services provided.
The limitations of this study include the relatively small sample, the lack of participants with diagnoses other than schizophrenia, the predominance of men in the sample, the lack of participants from ethnic minorities, and the fact that most participants had been ill for a substantial period. Further research is needed to replicate the findings reported here and to explore whether client characteristics such as phase of illness, gender, and minority status mediate the observed relationships between cognitive functioning, psychiatric symptoms, and outcomes in supported employment. Despite the limitations of the study, the findings suggest that key dimensions of psychiatric illness—cognition and symptoms—may influence both work outcomes and use of vocational services for clients participating in supported employment.
Dr. McGurk is assistant professor of psychiatry and Dr. Harvey is professor of psychiatry at the Mount Sinai School of Medicine, Box 1230, 1 Gustave L. Levy Place, New York, New York 10029-65764 (e-mail, [email protected]). Dr. Mueser is professor of psychiatry in the departments of psychiatry and community and family medicine at Dartmouth Medical School and the New Hampshire-Dartmouth Psychiatric Research Center in Concord, New Hampshire. Mr. LaPuglia and Ms. Marder are rehabilitation counselors at Pilgrim Psychiatric Center in West Brentwood, New York.
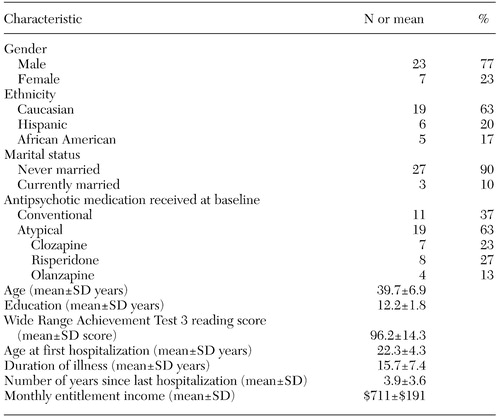 |
Table 1. Characteristics of 30 clients with schizophrenia in a study of cognitive and symptom predictors of work outcomes in a supported employment program
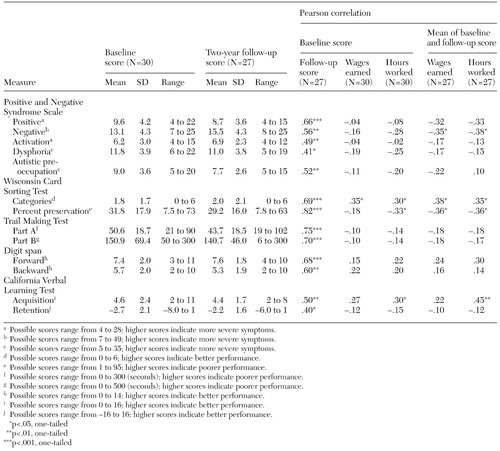 |
Table 2. Scores on symptom and cognitive measures at baseline and two-year follow-up and their relationship with total wages earned and total hours worked over two years for clients with schizophrenia in a supported employment program
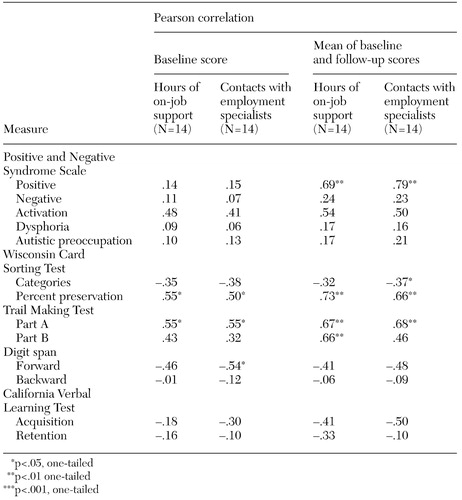 |
Table 3. Relationship of cognitive and symptom measures at baseline and two-year follow-up with hours of on-job support and number of contacts with employment specialists over two years for clients with schizophrenia in a supported employment program
1. Bond GR, Dietzen L, McGrew J, et al: Accelerating entry into supported employment for persons with severe psychiatric disabilities. Rehabilitation Psychology 40:91–111, 1995Crossref, Google Scholar
2. Drake RE, McHugo GJ, Becker DR, et al: The New Hampshire study of supported employment for people with severe mental illness: vocational outcomes. Journal of Consulting and Clinical Psychology 64:391–399, 1996Crossref, Medline, Google Scholar
3. Gervey R, Bedell JR: Supported employment, in Psychological Assessments and Treatment of Persons With Severe Mental Disorders. Edited by Bedell JR. Washington, DC, Taylor and Francis, 1993Google Scholar
4. Lehman AF, Goldberg R, Dixon LB, et al: Improving employment outcomes for persons with severe mental illnesses. Archives of General Psychiatry 59:165–172, 2002Crossref, Medline, Google Scholar
5. McFarlane WR, Dushay RA, Deakins SM, et al: Employment outcomes in family-aided assertive community treatment. American Journal of Orthopsychiatry 70:203–214, 2000Crossref, Medline, Google Scholar
6. Bond GR, Drake RE, Mueser KT, et al: An update on supported employment for people with severe mental illness. Psychiatric Services 48:335–346, 1997Link, Google Scholar
7. Beiser M, Bean G, Erickson D, et al: Biological and psychosocial predictors of job performance following a first episode of psychosis. American Journal of Psychiatry 151:857–863, 1994Link, Google Scholar
8. Daradkeh TK, Karim L: Predictors of employment status of treated patients with DSM-III-R diagnoses: can logistic regression model find a solution? International Journal of Social Psychiatry 40:141–149, 1994Google Scholar
9. Mueser KT: Cognitive impairment, symptoms, social functioning, and vocational rehabilitation in schizophrenia, in Comprehensive Treatment of Schizophrenia: Linking Neurobehavioral Findings to Psychosocial Approaches. Edited by Kashima H, Falloon IRH, Mizuno M, et al. Tokyo, Springer-Verlag, 2002Google Scholar
10. Slade E, Salkever D: Symptom effects on employment in a structural model of mental illness and treatment: analysis of patients with schizophrenia. Journal of Mental Health Policy and Economics 4:25–34, 2001Medline, Google Scholar
11. Strauss JS, Carpenter WT Jr: Prediction of outcome in schizophrenia, III: five-year outcome and its predictors. Archives of General Psychiatry 34:159–163, 1977Crossref, Medline, Google Scholar
12. Racenstein JM, Harrow M, Reed R, et al: The relationship between positive symptoms and instrumental work functioning in schizophrenia: a 10-year follow-up study. Schizophrenia Research 56:95–103, 2002Crossref, Medline, Google Scholar
13. Jaeger J, Douglas E: Neuropsychiatric rehabilitation for persistent mental illness. Psychiatric Quarterly 63:71–94, 1992Crossref, Medline, Google Scholar
14. Suslow T, Schonauer K, Ohrmann P, et al: Prediction of work performance by clinical symptoms and cognitive skills in schizophrenic outpatients. Journal of Nervous and Mental Disease 188:116–118, 2000Crossref, Medline, Google Scholar
15. Mueser KT, Salyers MP, Mueser PR: A prospective analysis of work in schizophrenia. Schizophrenia Bulletin 27:281–296, 2001Crossref, Medline, Google Scholar
16. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin 13:261–276, 1987Crossref, Medline, Google Scholar
17. Harvey PD, Serper MR, White L, et al: The convergence of neuropsychological testing and clinical ratings of cognitive impairment in patients with schizophrenia. Comprehensive Psychiatry 42:306–313, 2001Crossref, Medline, Google Scholar
18. Andreasen NC, Flaum M, Arndt S: The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Archives of General Psychiatry 49:615–623, 1992Crossref, Medline, Google Scholar
19. Becker DR, Drake RE: A Working Life: The Individual Placement and Support (IPS) Program. Concord, NH, New Hampshire-Dartmouth Psychiatric Research Center, 1993Google Scholar
20. White L, Harvey PD, Opler L, et al: Empirical assessment of the factorial structure of clinical symptoms in schizophrenia: a multisite, multimodal evaluation of the factorial structure of the Positive and Negative Syndrome Scale. Psychopathology 30:263–274, 1997Crossref, Medline, Google Scholar
21. Wilkinson GS: Wide Range Achievement Test 3: Administration Manual. Wilmington, Del, Wide Range, 1993Google Scholar
22. Harvey PD, Moriarty PJ, Friedman JI, et al: Differential preservation of cognitive functions in geriatric patients with lifelong chronic schizophrenia: less impairment in reading compared to other skill areas. Biological Psychiatry 47:962–968, 2000Crossref, Medline, Google Scholar
23. Wechsler D: Wechsler Adult Intelligence Scale-Revised. New York, Psychological Corp, 1981Google Scholar
24. Radford LM, Chaney EF, O'Leary MR, et al: Screening for cognitive impairment among inpatients. Journal of Clinical Psychiatry 39:712–715, 1978Medline, Google Scholar
25. Berg EA: A simple objective test for measuring flexibility in thinking. Journal of General Psychology 39:15–22, 1948Crossref, Medline, Google Scholar
26. Delis DC, Kramer JH, Kaplan E, et al: The California Verbal Learning Test Manual. New York, Psychological Corp, 1987Google Scholar
27. Drake RE, McHugo GJ, Bebout RR, et al: A randomized clinical trial of supported employment for inner-city patients with severe mental illness. Archives of General Psychiatry 56:627–633, 1999Crossref, Medline, Google Scholar
28. Heaton RK, Gladsjo JA, Palmer BW, et al: Stability and course of neuropsychological deficits in schizophrenia. Archives of General Psychiatry 58:24–32, 2001Crossref, Medline, Google Scholar
29. Friedman JI, Harvey PD, Coleman T, et al: Six-year follow-up study of cognitive and functional status across the lifespan in schizophrenia: a comparison with Alzheimer's disease and normal aging. American Journal of Psychiatry 158:1441–1448, 2001Link, Google Scholar
30. Green MF, Kern RS, Braff DL, et al: Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophrenia Bulletin 26:119–136, 2000Google Scholar
31. McGurk SR, Meltzer HY: The role of cognition in vocational functioning in s schizophrenia. Schizophrenia Research 45:175–184, 2000Crossref, Medline, Google Scholar
32. Bellack AS, Blanchard JJ, Murphy P, et al: Generalization of effects on training on the Wisconsin Card Sorting Test for schizophrenic patients. Schizophrenia Research 19:189–194, 1996Crossref, Medline, Google Scholar
33. Medalia A, Revheim N, Casey M: The remediation of problem-solving skills in schizophrenia. Schizophrenia Bulletin 27:259–267, 2001Crossref, Medline, Google Scholar
34. Wykes T, Reeder D, Corner J, et al: The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophrenia Bulletin 25:291–307, 1999Crossref, Medline, Google Scholar
35. Gould RA, Mueser KT, Bolton E, et al: Cognitive therapy for psychosis in schizophrenia: an effect size analysis. Schizophrenia Research 48:335–342, 2001Crossref, Medline, Google Scholar



