A Quality Improvement Process for Implementing the Texas Algorithm for Schizophrenia in Ohio
Abstract
Medication algorithms developed in Texas are being implemented in a number of states in the United States and internationally. This report describes a quality improvement process adapted from the Texas Medication Algorithm Project that was used to implement the Texas algorithm for schizophrenia in Ohio. A total of 38 physicians were surveyed about their perceptions of barriers to implementation of the guidelines. The physicians generally thought that the schizophrenia algorithm was good, current, and applicable. Although they did not perceive barriers to its implementation, they did not seem to alter their practices to a great extent in response to the algorithm. The results of the study may guide other states in their implementation of algorithms.
Unnecessary variability in the quality of health care and the consequent unpredictability of costs have led to the development of numerous guidelines (1,2). However, despite laudable dissemination efforts, the implementation of such guidelines is the primary barrier to improving the quality of care (3,4). A recent systematic review of guideline implementation efforts outlined a number of key barriers—both environmental and physician-specific—to physicians' acceptance of guidelines (5). The six main physician-level barriers are lack of awareness, lack of familiarity, lack of agreement, lack of self-efficacy, lack of outcome expectancy, and inertia. External barriers include patient-related factors, environmental factors, and characteristics of the guidelines themselves. The quality-improvement process developed for the Ohio Medication Algorithm Project attempted to address the physician-level and external barriers to the adoption of and adherence to guidelines.
The Ohio Medication Algorithm Project is a statewide quality-improvement initiative that utilizes the algorithms developed for the Texas Medication Algorithm Project (6,7). The original impetus for considering medication algorithms in Ohio occurred in 1999, when the executive director of a community mental health board struggled with the issue of formulary costs and medication management. This concern led one of the authors (JRS) to seek out assistance from the Texas project, which laid the foundation for the planning process in Ohio and which was funded by the state and by private sources. Simultaneously, initiatives dedicated to patient safety, consumer empowerment, and consumer recovery were under way nationally. All these factors enhanced the atmosphere for the acceptability of change in practice procedures and the eventual implementation of the algorithms (8).
A locally driven process that emphasized the needs and preferences of end users was determined to be crucial for successful implementation of the algorithms (9,10). Brief initial meetings with key leaders in the state and in local settings about barriers and facilitation led to an organizing framework for the eventual implementation of the algorithms. To ensure broad-based participation, leaders from potential implementation sites, board authorities, and consumer advocacy groups selected administrative representatives to participate in a series of planning task forces. Each task force addressed themes raised at initial awareness meetings with representatives from the Texas project about barriers to implementation of the algorithms. The task forces were mandated during the course of three meetings to come up with recommendations to address potential or perceived physician-related or external barriers to implementation.
The first meeting was designed to foster in-principle agreement with the "algorithm technology and the need for it." The second meeting involved specification of objectives, and the third was dedicated to setting dates and priorities for implementation. The task forces recommended that the schizophrenia algorithm be implemented before the two other algorithms—one for bipolar disorder and one for major depression—to avoid the "information overload" associated with implementing all three algorithms simultaneously.
The project was launched in the spring of 2000 at five sites. A half-day training session, easy-to-use laminated diagrams, biweekly teleconferences during which medical directors could interact with an expert on the algorithm (ALM, PEK, or LMC), bimonthly dinner conferences, and consultation with staff of the Ohio project were used to disseminate and maintain knowledge about the schizophrenia algorithm. The initial training and reference tools were used to address the barrier of lack of awareness and familiarity. The ongoing teleconference was used to address the barriers of lack of agreement and lack of outcome expectancy. This latter barrier refers to the fact that some physicians did not believe that improvement in patient outcomes would result by following the algorithm. For example, a physician may go immediately from a monotherapy trial to a combination therapy trial of two second-generation antipsychotics instead of trying monotherapy with an alternative agent as a result of lack of confidence in the outcome expectancy—or successful treatment—associated with monotherapy after the failure of one antipsychotic. Physicians who participated in these teleconference calls were able discuss their level of agreement or disagreement with the algorithm and the perceived benefit of the algorithm in clinical practice.
Bimonthly personal interactions with an expert, with project staff, and with other physicians who were using the algorithms were used to address the barrier of lack of self-efficacy, or self-perception of the ability to perform a task. Some psychiatrists were unfamiliar with the proper discontinuation and titration strategies when switching antipsychotic regimens or second-generation antipsychotics. These meetings allowed physicians to learn, from each other, how to use these algorithms in daily practice. A Web-based decision-support system (www.bstpractice.com) included tools for patients, families, clinicians, and executives. This system was used to support familiarity and awareness of the algorithms.
Unlike the Texas algorithm project, the Ohio project did not mandate the use of rating scales at every clinical visit, the frequency of visits, case manager involvement in algorithm implementation, or a manualized consumer education program. Reducing complexity was determined to be essential for the successful implementation of the algorithms by all task forces. Support from administrative and medical leadership and from the pharmaceutical industry removed any barriers related to access to medication and budgetary constraints on physicians' time. Quality-improvement feedback as a means of supporting internal peer review and regulatory compliance was provided to address any ongoing external barriers. The objective of the study reported here was to assess physicians' attitudes toward the schizophrenia algorithm and barriers to its implementation.
Methods
A survey similar to that used for the Texas Medication Algorithm Project was sent to the physicians participating in the Ohio project. The survey addressed a number of physicians' perceptions about the schizophrenia algorithm and some potential external barriers. Data from nine physicians for the pilot effort in 2000 have been combined with data from 29 physicians who began participation in 2001. All physicians who were involved responded to the survey. The surveys, conducted four months after formal implementation of the project at each site, asked physicians to rate their agreement with various statements on a 5-point Likert scale ranging from 1, strongly disagree, to 5, strongly agree. The five response categories were collapsed into three categories: agreement, neutral, and strong disagreement. Nonapplicable responses were excluded from the analysis.
Results
Of the 38 physicians surveyed, 25 (65 percent) were men, and 13 (35 percent) were women. Eighteen (47 percent) had at least nine years of experience, 20 (53 percent) had at least ten years of postresidency experience, and 12 (32 percent) had more than ten years of experience in the public sector.
Although only 13 physicians (35 percent) agreed that the new knowledge helped with decision making, 28 (74 percent) agreed with the treatment recommendations in the algorithm. And although 27 physicians (73 percent) reported that they had not prescribed new medications as a result of gaining knowledge about the algorithm, 26 (68 percent) agreed that the algorithm was applicable to a majority of their patients (more than 50 percent of patients). A majority of the physicians essentially affirmed the belief that barriers related to awareness, familiarity, and agreement were not a problem.
The second group of questions addressed how each physician felt about the algorithm in terms of his or her own practice—that is, the barriers of lack of self-efficacy and lack of outcome expectancy. A total of 31 physicians (82 percent) thought "the medication algorithms are current and represent good clinical practice" and reported that they "would continue to use them in their practice."
The final set of questions dealt with behavioral and organizational factors that might create barriers to adoption of algorithms. A total of 27 physicians (71 percent) reported that patients could easily obtain medications included in algorithms.
Discussion and conclusions
To our knowledge, this is the first published report on the transportability of the schizophrenia medication algorithm outside the state of Texas. In general, the physicians who participated in this study thought the schizophrenia algorithm was good, current, and applicable. They did not perceive barriers to the implementation of the algorithm, although they did not seem to alter their practices to a great extent in response to the algorithm. It is not clear whether these results reflect an attempt on the part of the physicians to look "good" in the context of the quality-improvement effort or are instead a valid reflection of actual practice. Physicians also may have been using clinical strategies in their practice that were similar to the algorithm. Data on the actual prescribing behavior of clinicians are being collected and will be presented in a future article. The sample of physicians was too small to enable us to determine whether the responses differed by sex or by whether the clinicians worked in rural versus urban settings. These questions will be addressed as the project grows.
A major difference between the Ohio effort and that in Texas is the lack of a systematic attempt by case managers in Ohio to measure symptomatic outcomes at regular intervals by using standardized scales and to provide that data back to physicians as well as the lack of a manualized consumer education program. The agencies that were involved in this effort did not have the resources to implement the Texas Medication Algorithm Project in full. Further research should attempt to determine the true costs and benefits of case manager support, manualized consumer education, and measurement of symptomatic response in public mental health systems.
Some of the peripheral benefits of the project include a uniform documentation form that ensures that patients' psychiatric and medication histories are not lost when the patients move from one provider to another. A foundation-funded manualized consumer curriculum on medication algorithms is being pilot tested. Finally, an effort to address health disparities is under way. The algorithm efforts in Texas have spawned a number of initiatives in other states. Ohio has implemented the Texas schizophrenia algorithm in a quality-improvement manner suitable to local needs and preferences.
Acknowledgments
This project was made possible through grant CQIR-01-CCOE from the Ohio Department of Mental Health, grant 032001-18 from the Health Foundation of Greater Cincinnati, and unrestricted education grants from Astra Zeneca, Eli-Lilly, and Janssen Pharmaceutica, Inc. The authors thank Shaohong Zheng for assistance with data analysis.
Dr. Dewan, Mr. Conley, Dr. Keck, and Dr. Strawkowski are affiliated with the department of psychiatry of the University of Cincinnati, P.O. Box 198048, Cincinnati, Ohio 45219 (e-mail, [email protected]). Dr. Svendsen is with the Ohio Department of Mental Health in Columbus. Dr. Shon is with the Texas Department of Mental Health and Mental Retardation in Austin. Mr. Staup is with the Butler County Mental Health Board in Fairfield, Ohio. Dr. Miller is with the department of psychiatry at the University of Texas Health Sciences Center in San Antonio. Dr. Crismon is with the clinical pharmacy division of the University of Texas College of Pharmacy in Austin. Dr. Rush and Dr. Trivedi are with the department of psychiatry at the University of Texas Southwestern Medical Center in Dallas. Dr. Skale is with the Queen City/Mitchell Community Mental Health Center in Cincinnati.
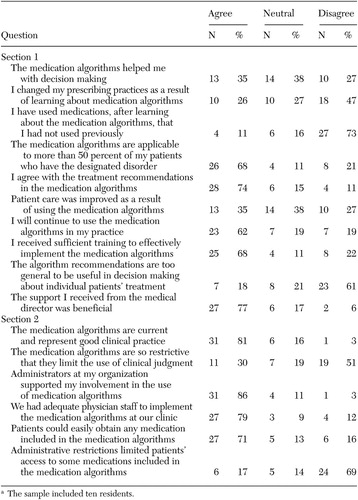 |
Table 1. Survey responses among 38 physicians who responded to a survey on medication algorithmsa
a The sample included ten residents.
1. Lehman AF, Steinwachs DM: Translating research into practice: the schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1–10, 1998Crossref, Medline, Google Scholar
2. Herz MI, Liberman RP, Lieberman JA, et al: Practice Guideline for the Treatment of Patients With Schizophrenia. Washington, DC, American Psychiatric Association, Apr 1997Google Scholar
3. Grimshaw JM, Russell IT: Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 342:1317–1322, 1993Crossref, Medline, Google Scholar
4. Betz Brown J, Shye D, McFarland BH, et al: Controlled trials of CQI and academic detailing to implement a clinical practice guideline for depression. Joint Commission Journal on Quality Improvement 26(1):39–54, 2000Google Scholar
5. Cabana MD, Rand CS, Powe NR, et al: Why don't physicians follow clinical practice guidelines? JAMA 282:1458–1465, 1999Google Scholar
6. Gilbert DA, Altshuler KZ, Rago WV, et al: Texas Medication Algorithm Project: definitions, rationale, and methods to develop medication algorithms. Journal of Clinical Psychiatry 59:345–351, 1998Crossref, Medline, Google Scholar
7. Chiles JA, Miller AL, Crismon ML, et al: The Texas Medication Algorithm Project: development and implementation of the schizophrenia algorithm. Psychiatric Services 50:69–74, 1999Link, Google Scholar
8. Rogers EM: The challenge: lessons for guidelines from the diffusion of innovations. Journal on Quality Improvement 21:324–328, 1995Crossref, Google Scholar
9. Rubenstein LV, Jackson-Triche M, Unutzer J, et al: Evidence-based care for depression in managed primary care practices. Health Affairs 18(5):89–105, 1999Google Scholar
10. Torrey WC, Drake RE, Dixon L, et al: Implementing evidence-based practices for persons with severe mental illnesses. Psychiatric Services 52:45–50, 2001Link, Google Scholar