Mortality of Mental Health Service Recipients in Vermont and Oklahoma
Abstract
The authors compared statewide mortality rates for people with severe mental illness who were served in public mental health systems of care in Vermont and Oklahoma. In both states, mortality rates for younger service recipients, but not for older recipients, were significantly higher than those for the general population. In interpreting cross-region comparisons, several possible causes of variation, including differences in caseload composition and causes outside the control of the public mental health authority, must be considered.
A recent article in this journal (1) illustrated the potential power of large-scale studies of mortality rates for people with mental disorders in the evaluation of systems of care. In that article, Currier reported that national mortality rates for people with mental disorders in six of the seven countries analyzed increased substantially as psychiatric hospitalization rates declined between 1960 and 1995. Similarly, the National Association of State Mental Health Program Directors has endorsed the computation and publication of statewide mortality rates for people served in public mental health systems of care (2).
After publication of mortality rates for public mental health clients in Massachusetts (3), Barreira (4), the state's deputy mental health commissioner, urged caution in interpreting such data. Although Barreira acknowledged the importance of attention to mortality in measuring service system performance, he cited the need to make multistate comparisons focusing on active clients and to consider the impact of other risk factors.
We address these concerns in this report by examining mortality rates for people with severe mental illness who had recently been served by the state mental health systems in Vermont and Oklahoma. The analysis controlled for variation in three of the most important risk factors for mortality: age, gender, and race. On the basis of the findings, we propose standard procedures for measuring and reporting multistate comparisons of mortality rates and suggest directions for further research.
Methods
The study particpants were persons 18 to 79 years of age who had a serious mental illness and were served by community-based public mental health programs for adults with severe and persistent mental illness in either Vermont or Oklahoma between 1992 and 1998. Eligibility criteria for the two states' programs were similar; both included a broad range of diagnoses with similar lists of symptoms and functional criteria. Persons with a diagnosis of primary substance abuse, mental retardation or developmental disabilities, and V code problems and conditions were excluded.
In 1997 a total of 3,362 people who met the study criteria were served in Vermont, and 20,914 were served in Oklahoma. These figures represented .8 percent of adults in the target age group in Vermont and .9 percent in Oklahoma.
Information about individuals served in the public mental health system is maintained in each state mental health agency. Information about deaths of state residents is maintained in each state's vital records mortality database. For our analysis, anonymous person-level data sets were constructed from the mental health and vital records databases. These data sets included only the date of birth, the sex, and the race of each person represented. Because this project involved program evaluation using anonymous data, institutional review board approval was not required.
A two-year mortality rate was determined for individuals served during each year by measuring the overlap between the mental health and mortality databases. Because the data sets did not include person identifiers, probabilistic population estimation was used to determine the number of individuals in each mental health data set who also appeared in each mortality data set. The two-year mortality rates included deaths that occurred during the treatment year and the subsequent year.
Probabilistic population estimation is a statistical procedure that provides valid and reliable measures of the size and overlap of data sets that do not include unique person identifiers. These estimates are based on a comparison of the distribution of dates of birth in the data sets to the known distribution of dates of birth in the general population. More detailed descriptions of this procedure, with verification, have been published elsewhere (5,6). In our analysis, the probabilistic estimates of the number of deaths were, on average, within .9 percent of the true value, and the 95 percent confidence intervals included the true value in 94 percent of the cases.
The six annual mortality rates generated by this procedure were averaged to account for potential year-to-year variation and to increase the precision of the estimates. The averaged mortality rates for service recipients in three age groups and in the two gender groups were compared with the mortality rates for the general population of each state and for the general population of the United States. Because the population of Vermont is almost exclusively white, the results for Oklahoma reported here describe the white population of that state.
Results
As Table 1 shows, relative risk decreased with increasing age for both genders in both states. Among service recipients aged 50 or older, the mortality rates were frequently no different from the rates for other residents of the states. In the youngest age group, women had significantly greater relative risk of mortality than men, but gender differences among the older service recipients were inconsistent and frequently insignificant.
Among service recipients under 50 years of age, the relative risk of mortality (compared with the general population of the same state) was significantly higher in Vermont than in Oklahoma. When relative risks for the two states were standardized with reference to mortality rates for the United States, a very different picture emerged. In three of these four age and gender groups, the relative risk of mortality was not different between the two states. Differences in the mortality rates for the general population in the two states, not differences in the mortality rates for service recipients, accounted for most of the difference in relative risk.
Discussion and conclusions
The relative risks of mortality for people with serious mental illness computed in this study were within the range reported in the literature (7). The patterns of relative risk associated with age and gender groups were also consistent with the literature (8). These earlier studies, however, tended to focus on small, narrowly defined patient populations. This study, by contrast, demonstrated state-level measures of the relative risk of mortality for people served in community-based programs. These measures can be used to compare the performance of public mental health systems of care in a larger number of states.
In response to Barreira's concern, this study focused specifically on a period close to that during which services were received. Earlier studies of mortality among recently discharged psychiatric patients found that most mortality occurred during the first two years after discharge (9) and that there was little elevation in risk of mortality after ten years (7).
Many of these earlier studies used follow-up interviews with family members and other key informants to derive mortality rates (7). More recently, direct linkage between mental health and vital records databases has been used increasingly to study client outcomes (3,9). This study used a method that may be more acceptable in the context of growing concern about confidentiality of medical records (10).
As multistate comparisons of mortality become increasingly available, caution will be needed both in interpreting the findings and in identifying policy implications. A wide range of potential causes of variation must be considered. They include differences in caseload composition and causes outside the control of the state mental health authority, as well as causes over which the state has some control. In addition, it is important to recognize that complex systems of care should not be evaluated on the basis of any single indicator of program performance.
There are substantial differences in caseload composition across states that are related to differences in the scope of authority of state mental health agencies and differences in access to care for people in various risk groups. These differences have important implications for mortality rates. To help adjust for case-mix differences, this study reported mortality rates for specific age and gender groups. Other case-mix variables should be considered as well.
A wide range of potential causes of mortality should be considered in all cross-state comparisons. In this study an apparent cross-state difference in mortality for service recipients was accounted for by differences in the mortality rate of the general population of the two states. Other potential explanations of differences in mortality rates include differences in socioeconomic status, access to health care, and lifestyle factors. Mental health treatment variables, such as the use of psychoactive medication, may also have a role. Future research should test the ability of such factors to explain differences in mortality rates.
Finally, the quality of care provided by a state mental health system should never be judged by a single measure. Several different client outcomes should be monitored to provide a balanced assessment of performance. These outcomes may include change in clinical status and rates of employment and involvement with the criminal justice system. Outcome measures should also be complemented by measures of access to care, including the overall level of access and access for special populations, and measures of adherence to evidence-based practice patterns in the delivery of services to people in need.
Cross-state comparisons of the functioning of mental health service delivery systems (and comparisons across regions within states) can have a beneficial effect on the quality of care. Appropriate attention to case mix and contextual factors as well as consideration of a range of quantitative indicators of service system performance is essential to achieving this goal. We hope this paper contributes to progress in that direction.
Acknowledgments
This project was partly supported by grants to the states of Vermont and Oklahoma from the State Indicator Pilot Project of the Center for Mental Health Services.
Dr. Pandiani and Dr. Bramley are affiliated with the Vermont Department of Developmental and Mental Health Services, 103 South Main Street, Waterbury, Vermont 05671-1601 (e-mail, [email protected]). Dr. Banks is with the Bristol Observatory in Bristol, Vermont. Ms. Moore is with the Oklahoma Department of Mental Health and Substance Abuse Services in Oklahoma City. An earlier version of this paper was presented at the annual Conference on Behavioral Healthcare Evaluation held December 6-8, 2000, in Orlando.
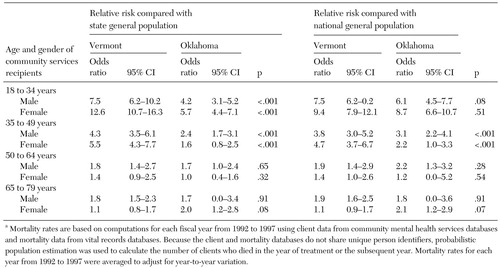 |
Table 1. Risk of mortality among white adults receiving community services for severe and persistent mental illness in Vermont 1992 to 1997, relative to state and national mortality rates for the general population, by age and gendera
a Mortality rates are based on computations for each fiscal year from 1992 to 1997 using client data from community mental health services databases and mortality data from vital records databases. Because the client and mortality databases do not share unique person identifiers, probabilistic population estimation was used to calculate the number of clients who died in the year of treatment or the subsequent year. Mortality rates for each year from 1992 to 1997 were averaged to adjust for year-to-year variation.
1. Currier GW: Psychiatric bed reductions and mortality among persons with mental disorders. Psychiatric Services 51:851, 2000Link, Google Scholar
2. Final Report on the 16-State Study on Mental Health Performance Measures. Arlington, Va, National Association of State Mental Health Directors Research Institute, 2002Google Scholar
3. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036-1042, 1999Link, Google Scholar
4. Barreira P: Reduced life expectancy and serious mental illness. Psychiatric Services 50:995, 1999Link, Google Scholar
5. Banks SM, Pandiani JA, Schacht LM, et al: Age and mortality among white male problem drinkers. Addiction 95:1249-1254, 2000Crossref, Medline, Google Scholar
6. Banks SM, Pandiani JA: Probabilistic population estimation of the size and overlap of data sets based on date of birth. Statistics in Medicine 20:1421-1430, 2001Crossref, Medline, Google Scholar
7. Felker B, Yazel JJ, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356-1363, 1996Link, Google Scholar
8. Martin RL, Cloninger CR, Guze SB, et al: Mortality in a follow-up of 500 psychiatric outpatients: I. total mortality. Archives of General Psychiatry 42:47-54, 1985Crossref, Medline, Google Scholar
9. Black DW, Warrack KR, Winokur G: Excess mortality among psychiatric patients: the Iowa Record-Linkage Study. JAMA 253:58-61, 1985Crossref, Medline, Google Scholar
10. Pandiani JA, Banks SM, Schacht LM: Personal privacy versus public accountability: a technological solution to an ethical dilemma. Journal of Behavioral Health Services and Research 25:456-463, 1998Crossref, Medline, Google Scholar



