Revised Cost Estimates of Medicaid Recipients With Serious Mental Illness and HIV-AIDS
In a previous study some of the authors of the study presented here estimated the 1996 costs for Medicaid-reimbursed health and behavioral health care among persons with co-occurring serious mental illness and HIV infection or AIDS and compared them with the costs among persons with only HIV-AIDS or only serious mental illness ( 1 ). That study provided the first cost estimates for persons with co-occurring serious mental illness and HIV-AIDS. In that report, annual expenditures for medical and behavioral health treatment were found to be $13,800 per person. In comparison, persons with only HIV-AIDS had lower annual expenditures of about $7,400 per person and those with only serious mental illness had treatment costs of about $5,800 per person.
The comprehensive cost of treatment for all groups was, however, underestimated because state Medicaid data were not available at that time for pharmacy, nursing home, outpatient services, home health care, or out-of-pocket expenses. In addition, Medicare costs for persons who were dually eligible for both Medicaid and Medicare benefits were not included in the estimates, even though substantial numbers of people from this group were in the previous sample. Because the previous study did not report the copayment for Medicare costs, our cost estimates were lower than they should have been, especially for the group with co-occurring serious mental illness and HIV-AIDS because they were more likely to be dually eligible for both Medicaid and Medicare and thus have higher costs.
The study presented here updates the authors' previous 1996 cost analysis with a comprehensive data set obtained from the Centers for Medicare and Medicaid Services (CMS). Our revised 1996 estimates provide an important baseline for continual monitoring of utilization and cost of services for persons with co-occurring serious mental illness and HIV-AIDS. Baseline data will be needed as costs change with the introduction of new treatments, such as the implementation of highly active antiretroviral therapy in 1995, as well as novel psychotropic agents and other treatment innovations. In addition, these new estimates will enable us to compare our results with other published studies on populations with serious mental illness where similar data sources were employed ( 3 , 4 ).
Methods
Persons selected for this study were a subset of the previous study cohort who could be linked to the CMS Medicaid files ( 1 ) and met the selection criteria for the study presented here: aged 18–64 years, eligible to receive Medicaid services in Philadelphia, continuously enrolled in the Medicaid program in 1996, and having a claim with a serious mental illness or HIV-AIDS diagnosis between 1985 and 1996. Individuals dually eligible for Medicaid and Medicare were excluded, as were those enrolled in voluntary health maintenance organizations, the majority of whom had no serious physical or mental health problems. All of those with no service claims for serious mental illness or HIV-AIDS service during 1996 were selected as the comparison group.
Persons were deemed to have a serious mental illness on the basis of a claim for treatment that included a diagnosis of schizophrenia ( ICD-9 code 295) or major affective disorder ( ICD-9 code 296) and at least one inpatient or two outpatient treatment contacts with these diagnoses, following a protocol developed by Lurie and colleagues ( 5 ) to ensure accurate diagnoses. ICD-9 codes of 042 (HIV infection with specified conditions), 043 (HIV infection causing other specified conditions), and 044 (other HIV infections) were used to identify an HIV-AIDS-related diagnosis. Psychiatric drugs were classified using therapeutic class codes 74–77 and 80–84 (anticonvulsants; anti-Parkinsonian agents; antidepressants; barbiturates; cerebral stimulants; nonbarbiturates, sedatives, or hypnotics; other psychotherapeutics; and tranquilizers). No direct client contact was involved in the study. This research was approved by the University of Pennsylvania's institutional review board through the Office of Regulatory Affairs, which also provided ongoing oversight for the protection of human subjects.
The 1996 Pennsylvania Medicaid Analytic eXtract data, formerly known as the State Medicaid Research Files, were used for the analysis. The data files from the CMS contain person-level sociodemographic information and service-level information, such as type of service, date of service, provider, diagnostic codes, and cost for the Medicaid recipient ( 6 ). Medicaid claims records were used both to identify diagnostic groups and to construct reimbursement costs by type of service. The Medicaid claims files represent an excellent resource for health services research on vulnerable population groups, given that one in five Americans is enrolled in the Medicaid program, Medicaid is a major payer for mental and substance use disorders, and cost estimates are comprehensive because of the extensive nature of the benefit coverage ( 7 ).
Annual costs were aggregated for the four groups (serious mental illness and HIV-AIDS, serious mental illness only, HIV-AIDS only, and neither condition) using 1996 Medicaid-reimbursed service claims with separate categories for health and psychiatric services including drug and alcohol treatment. Service records were aggregated at the individual level to reflect the total reimbursement costs. A descriptive analysis was employed to compare characteristics and mean expenditures per group using chi square and analysis of variance tests of significance.
Results
The study participants included 23,729 adult Medicaid recipients—196 individuals had a diagnosis of co-occurring serious mental illness and HIV-AIDS, 5,076 had a diagnosis of serious mental illness only, 482 had a diagnosis of HIV-AIDS only, and 17,975 were in the comparison group. Statistically significant differences between groups were found in gender, race, age, and Medicaid eligibility status. Persons with co-occurring serious mental illness and HIV-AIDS constituted 1% of the study population. Compared with the group with only HIV-AIDS, the group with co-occurring illnesses was older and was more likely to be disabled (as measured by receipt of Supplemental Security Income [SSI]), black, and female. Compared with the group with serious mental illness only, the group with co-occurring illnesses was older, more likely to be disabled and male and less likely to be black. The group with co-occurring illnesses was older and more likely than the comparison group to be male and disabled. Because the comparison group for this analysis represented individuals who did not voluntarily enroll in a Medicaid managed care program before it was mandated, they may have been those who were relatively more disabled than the general Medicaid population, as evidenced by the high number of individuals in our sample receiving SSI disability benefits (60%).
Persons selected for this study were a subset of the previous study cohort (N=23,729 of 60,503, or 39%). Only 39% of the original sample was able to be analyzed in the study presented here because of exclusion criteria and matching issues between the CMS data files and the original Medicaid data files that the original sample was drawn from. Compared with the group with comorbid illnesses in the original study, the subset with comorbid illnesses in this analysis had the same median age of 37, was less likely to be male (N=116 of 196, or 59%, versus N=173 of 268, or 65%), was less likely to be black (N=45 of 196, or 23% versus N=136 of 268, or 51%), and was more likely to be disabled (N=184 of 196, or 94% versus N=182 of 268, or 68%). Compared with the group with only HIV-AIDS in the original study, the subset with only HIV-AIDS in this updated study had a slightly younger median age (36 years versus 39 years), was less likely to be black (N=83 of 482, 17%, versus N=265 of 410, 65%), was less likely to be male (N=318 of 482, 66%, versus N=307 of 410, 75%), and was more likely to be disabled (N=414 of 482, 86%, versus N=258 of 410, 63%).
Table 1 shows overall cost patterns for the groups in our sample. The group with co-occurring serious mental illness and HIV-AIDS had the highest annual expenditures, totaling $20,038 per person. In comparison, those with only HIV-AIDS used $14,714 of services per person, and those with only serious mental illness used $9,039 of services per person. The comparison group had a cost of $6,613 per person.
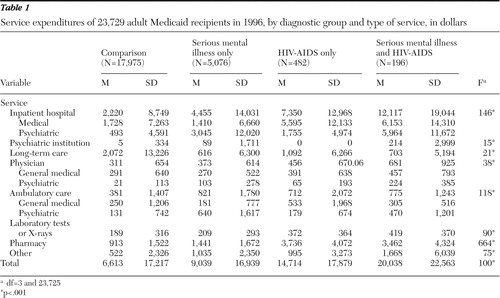 |
Table 1 also provides a detailed breakdown of costs by service category for each study group. Inpatient and other institutional care accounted for 65% of the costs for the group with co-occurring illnesses, 57% of the costs for the group with only serious mental illness, and 65% of the costs for the comparison group. Pharmacy costs were 25% of the costs for the group with HIV-AIDS alone, 17% of the costs for the group with co-occurring illnesses, 16% of the costs for the group with serious mental illness alone, and 14% of the costs for the comparison group. In ranking the costs within each group, psychiatric costs were highest in the group with co-occurring illnesses and costs for medical services were the highest in the group with co-occurring illnesses.
Discussion
This study improved on our previous 1996 cost estimates of treating persons with serious mental illness and HIV-AIDS and provides a baseline for longitudinal comparisons. Results are consistent with our previous study, which also reported that the group with co-occurring serious mental illness and HIV-AIDS was the most costly population and required significant levels of care, compared with the comparison group and the group with serious mental illness alone. Little difference was seen in the medication and cost for treating HIV-AIDS between the group with co-occurring illnesses and the group with HIV-AIDS only. Even though the group with only HIV-AIDS did not have co-occurring serious mental illness, the group still had substantial psychiatric costs for mental health problems resulting from anxiety and other diagnoses. Using the consumer price index to estimate the 1996 cost of HIV-AIDS in 2008 dollars, the mean cost for the group with only HIV-AIDS would be $20,520 and for the group with comorbid illnesses it would be $27,945.
Our findings for the costs for HIV-AIDS care are consistent with the estimates in the Hopkins study of Medicaid AIDS patients ( 3 ), and our costs of care for the population with co-occurring serious mental illness and HIV-AIDS are also similar to those of a four-state Medicaid study that looked at a similar population ( 8 ). When we look at the costs for the HIV-AIDS population groups, regardless of the presence of serious mental illness, the cost was $16,253 per study participant, which is similar to the 1998 costs of $16,008 found by Roberts and colleagues ( 9 ). We found that 7% of the expenditures for those with HIV-HIDS were for nursing home costs. We would expect even smaller percentages in the future with the newer treatment technologies, such as highly active antiretroviral therapy.
It should be noted that a limitation to these estimates is the lack of cost data on Medicaid clients who are dually eligible for Medicare and Medicaid. Now that Medicare Part D is the primary reimbursement source for pharmacy costs, as well as inpatient hospital care, studies of the dually eligible group will need to link Medicaid and Medicare data sets to get comprehensive information. Additionally, it is possible that the severity of illness for HIV-AIDS differs in the population with only HIV-AIDS and the population with comorbid serious mental illness and HIV-AIDS, which might explain the higher medical costs for the participants with comorbid illnesses. Evidence of this was found by study authors showing a higher prevalence of opportunistic infections in the population with comorbid serious mental illness and HIV-AIDS than in the HIV-AIDS-only population ( 10 ).
Conclusions
Although the absolute costs of care are much higher than we reported earlier, these results are consistent with our previous study in that both studies showed that individuals with co-occurring serious mental illness and HIV-AIDS had the highest costs. These improved estimates provide an excellent baseline for follow-up studies examining changes in treatment and cost of care since the advent of newer antipsychotic and antiretroviral drug combinations in the mid-1990s. We expect annual as well as lifetime costs to be higher in the future both for those with HIV-AIDS alone and for those with comorbid serious mental illness and HIV-AIDS, because of potential medical complications associated with aging and some of the side effects of treatment.
Acknowledgments and disclosures
This research was supported by grant 5-RO1-DA-015627-05 from the National Institute on Drug Abuse (HIV Prevention Program among Substance Abusing SMI) and by grant 5-RO1-NR-008851-05 from the National Institute of Nursing Research (Nursing Intervention for HIV Regimen: Adherence among SMI).
The authors report no competing interests.
1. Rothbard AB, Metraux S, Blank MB: Cost of care for Medicaid recipients with serious mental illness and HIV infection or AIDS. Psychiatric Services 54:1240–1246, 2003Google Scholar
2. Fasciano NJ, Cherlow AL, Turner BJ, et al: Profile of Medicare beneficiaries with AIDS: application of an AIDS casefinding algorithm. Health Care Financing Review 19:19–38, 1998Google Scholar
3. Moore RD, Bartlett, JG: Combination antiretroviral therapy in HIV infection: an economic perspective. PharmacoEconomics 10:109–113, 1996Google Scholar
4. Walkup J, Crystal S, Sambamoorthri U: Schizophrenia and major affective disorder among Medicaid recipients with HIV/AIDS in New Jersey. American Journal of Public Health 89:1101–1103, 1999Google Scholar
5. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69–71, 1992Google Scholar
6. Medicaid Data Sources: General Information: Overview. Baltimore, Md, Centers for Medicaid and Medicare Services. Available at www.cms.hhs.gov/MedicaidDataSourcesGenInfo Google Scholar
7. Crystal S, Akincigil A, Bilder S, et al: Studying prescription drug use and outcomes with Medicaid claims. Medical Care 45:S58–S65, 2007Google Scholar
8. Coffey RM, Mark T, King E, et al: National Estimates of Expenditures for Mental Health and Substance Abuse Treatment, 1997. SAMHSA pub no SMA-00-3499. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment, Center for Mental Health Services, July 2000Google Scholar
9. Roberts RR, Kampe LM, Hammerman M, et al: The cost of care for patients with HIV from the provider economic perspective. AIDS Patient Care and STDs 20:876–885, 2006Google Scholar
10. Blank MB, Rothbard AB, Lee S, et al: Opportunistic infections in HIV infected people with co-occurring MI. Presented at the Conference on Complexities of Co-occurring Conditions: Harnessing Services Research to Improve Care for Persons with Mental, Substance Use and Physical/Medical Disorders, Washington, DC, June 23–25, 2004Google Scholar



