Can SSDI and SSI Beneficiaries With Mental Illness Benefit From Evidence-Based Supported Employment?
In recent years, policy makers at the Social Security Administration (SSA) have become increasingly concerned by the rising number of beneficiaries with psychiatric disabilities of working age (18–64 years) in its two disability programs: Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI). In fact, psychiatric disability (that is, disability from mental illness) comprises the largest diagnostic group on the disability rolls ( 1 ). At the same time, SSA has been criticized for failing to do more to assist beneficiaries to return to work ( 2 ). Historically, people with psychiatric disabilities have been unlikely to reenter the labor force. However, recent research on supported employment for this population shows great promise ( 3 , 4 , 5 ), suggesting a reconsideration of the role of competitive employment (defined as a regular permanent community job that pays at least minimum wage and for which anyone can apply) for this group.
Although both the SSDI and SSI programs provide income support to individuals with disabilities, their rules governing eligibility and the disincentives for working differ profoundly. SSDI provides income support to individuals of working age who have paid a specified amount of Social Security tax and subsequently are determined to be eligible because of a disability. SSDI beneficiaries are allowed a trial work period in which they may earn more than a federally established earnings limit without affecting their SSDI status. However, once they complete their trial work period, they are subject to losing SSDI benefits. The total loss of benefits has been referred to as "falling off a cliff."
The SSI program provides income assistance to individuals with disabilities who do not have a substantial work history. Eligibility is based on income and resources, in addition to establishing that the disability is severe enough to render the person unable to work for at least 12 months ( 6 ). SSI beneficiaries can work for pay without losing SSI eligibility; however, after certain exclusions, SSI payments are reduced by $1 for every $2 in earned income. Finally, approximately one-fourth of SSDI beneficiaries are "dual eligibles," meaning that they are eligible to receive both SSI and SSDI payments ( 7 ).
Individuals with psychiatric disabilities, 85% of whom have either a mood disorder or a psychotic disorder ( 8 , 9 ), are the fastest-growing SSA beneficiary group. Between 1989 and 1999, the number of SSDI and SSI beneficiaries with psychiatric disabilities more than doubled, from a little over one million to nearly 2.5 million. By 1999, 27% of SSDI beneficiaries of working age and 34% of SSI beneficiaries of working age were disabled by mental illness ( 10 ). These figures do not include individuals who had a psychiatric disorder in addition to their primary disability, a group comprising approximately one-fifth of the SSI and SSDI rolls ( 10 ). One primary reason for this growth is that beneficiaries with psychiatric disabilities generally are younger than other groups of SSA beneficiaries ( 11 , 12 ), which leads them to stay on disability rolls longer than other beneficiaries ( 10 , 13 ).
Disincentives to working
There is little question that receipt of disability benefits creates a powerful disincentive to seeking out work. The process of applying for and receiving SSA benefits has demoralizing and debilitating effects on identity and self-esteem ( 14 , 15 , 16 ), discouraging those who obtain benefits from entering or reentering the work force ( 17 , 18 ). Among persons with mental illness who are beneficiaries of SSI, SSDI, or both, less than 1% leave the disability rolls each year because earned income has exceeded eligibility criteria ( 13 , 19 ). Surprisingly, receipt of assistance from the state-federal vocational rehabilitation system does not appear to increase movement from SSA disability rolls ( 20 ). In one study even though nearly half of beneficiaries with mental illness reported they would be ashamed if they did not try work, over 90% refused an invitation to participate in an employment program ( 2 ).
For most beneficiaries, losing health insurance is a far greater worry than losing cash payments ( 7 , 21 , 22 , 23 , 24 , 25 ). Most SSDI and SSI recipients receive health insurance in the form of Medicare, Medicaid, or both ( 8 , 23 ). Specifically, after a two-year waiting period, SSDI beneficiaries are automatically eligible for Medicare. And in most states SSI beneficiaries are automatically eligible for Medicaid. However, SSI beneficiaries whose income exceeds a certain level may lose their SSI and consequently may be vulnerable to losing Medicaid benefits. To mitigate this disincentive to employment, Congress has created special programs to allow individuals who lose SSI eligibility because of earnings to continue to qualify for Medicaid (for example, section 1619B of the Social Security Act and the Medicaid Buy-In Program) ( 26 ). As of 2004, 29 states had implemented changes under the Medicaid Buy-In Program to expand Medicaid eligibility with more liberal income thresholds for people with disabilities who are working ( 27 ).
Work potential of beneficiaries with psychiatric disabilities
Studies typically have found competitive employment rates of 15% or less for clients receiving treatment for psychiatric disorders ( 18 , 28 ). In community studies, employment rates for people with psychiatric disabilities are lower than for individuals with other disabilities ( 10 ), and their rates are even lower if they receive SSDI or SSI. The poorer work outcomes for disability beneficiaries could be a reflection of either illness severity or the disincentives to working, or both. Another barrier to employment has been challenges in obtaining help from the state-federal vocational rehabilitation system. Historically, vocational rehabilitation sponsorship for services has been far lower for psychiatric disabilities than for other disability groups ( 29 , 30 ). Possible reasons include vocational rehabilitation counselors' unfamiliarity and discomfort with psychiatric disabilities as well as their stereotypes of poorer work potential for this population, difficulties clients have in navigating the eligibility process, and bureaucratic delays in setting intake appointments.
One important change in the vocational rehabilitation landscape is the recent emergence of supported employment as an effective approach for helping persons with mental illness, even those with the most severe psychiatric disabilities, to attain competitive employment ( 3 , 4 , 31 , 32 , 33 , 34 ). The best-researched approach to supported employment is individual placement and support ( 35 ). The principles of this program include zero exclusion, integration of mental health and vocational services, benefits counseling, client choice regarding jobs and disclosure, rapid job search, and individualized ongoing supports. Eleven randomized controlled trials favor individual placement and support over various other approaches ( 36 ), and the principles of the program are supported by empirical research ( 3 ).
Surprisingly, little attention has been given to the outcomes for SSDI and SSI beneficiaries with mental illness enrolled in vocational programs. An evaluation of a job club found that SSI beneficiaries were less successful than both SSDI beneficiaries and nonbeneficiaries in obtaining a competitive job, a result the authors attributed to the poorer work histories, earlier age of illness onset, and more hospitalizations among SSI beneficiaries ( 37 ). An early study of a supported employment program found poorer competitive employment outcomes for both SSI and SSDI beneficiaries ( 38 ). An evaluation of benefits counseling found that SSDI beneficiaries had higher earnings than either SSI or dual beneficiaries ( 39 ). Recently, a multisite study of different models of supported employment found that persons not receiving entitlements were four times as likely to retain their competitive job for six months or more compared with persons receiving entitlements ( 40 ). None of these studies focused specifically on evidence-based supported employment.
The purpose of this study was to examine whether SSDI and SSI beneficiaries with mental illness respond favorably to evidence-based supported employment to the same extent as individuals who do not have SSA benefits. The focus was therefore on the differences in employment outcomes for SSDI and SSI beneficiaries enrolled in individual placement and support services versus usual services and in comparison with the difference for nonbeneficiaries.
Methods
Overview
We examined the merged data from four independent randomized controlled trials to determine the magnitude of effects of individual placement and support on three employment outcomes (obtaining a job, job tenure, and amount of work) for four beneficiary groups (SSI, SSDI, dually eligible beneficiaries, and nonbeneficiaries). We also examined the effect of benefit status on outcomes. The original projects were approved by institutional review boards at local sites and participating universities. All study participants gave written informed consent after participating in multiple informational groups in which study procedures were explained. In addition, the data reanalyses were approved by institutional review boards.
Sample and procedures
The sample consisted of study participants from four randomized controlled trials of individual placement and support services versus usual services ( 41 , 42 , 43 , 44 ). All four studies compared a newly established individual placement and support program with one or more well-established vocational programs, ensuring fidelity to the individual placement and support model through intensive training or consultation as well as monitoring with the individual placement and support fidelity scale ( 45 ).
In three studies, participants were recruited from mental health centers, and in the Chicago study recruitment was from a psychiatric rehabilitation agency. Participants were adults who met each state's criteria for severe mental illness, typically a DSM-IV ( 46 ) axis I or II diagnosis plus severe and persistent impairment in psychosocial functioning. Participants in all four studies were unemployed at the time of study admission. Other eligibility criteria common across the four studies included desire for competitive work, ability and willingness to give informed consent, and absence of significant medical conditions that would preclude working or participating in assessment interviews. In addition, all participants were required to attend multiple research information meetings, in which the project was explained, and they gave written informed consent to participate in the study. All four studies used similar protocols to track employment outcomes and assessed symptoms with either the Brief Psychiatric Rating Scale (BPRS) ( 47 ) or a later scale incorporating BPRS items.
Data sources
The New Hampshire study was conducted in two mental health centers, which were in Concord and Manchester, New Hampshire ( 42 ). It compared individual placement and support (N=74) with group skills training (N=69), in which a rehabilitation agency unaffiliated with the mental health centers provided prevocational skills training, individualized placement, and follow-along support. Clients were recruited from 1991 to 1993.
The DC study recruited clients in an intensive case management program in Washington, D.C., from 1994 to 1995 ( 43 ). Individual placement and support (N=76) was compared with enhanced vocational rehabilitation (N=76), in which rehabilitation agencies provided stepwise vocational services, primarily paid work adjustment training in a sheltered workshop.
The Hartford study recruited clients receiving services at a mental health center in Hartford, Connecticut, from 1996 to 1998 ( 44 ). Clients were randomly assigned as follows: 68 to individual placement and support, 67 to a psychosocial rehabilitation program, and 69 to standard services. Psychosocial rehabilitation program participants attended a series of preparatory training activities, followed by transitional employment and assistance with obtaining competitive work. Standard services involved access to two off-site employment programs, one providing brokered supported employment (which lacked the integrated services offered by individual placement and support) and the other providing supervised janitorial enclaves. Because the differences in employment outcomes for the two Hartford control groups were small, they were combined into a single control group.
In the Chicago study, clients attending two separate day programs at a comprehensive psychiatric rehabilitation agency in Chicago were randomly assigned from 1999 to 2002 to individual placement and support (96 clients) or to a diversified placement approach (98 clients). The latter program offered stepwise preparation for competitive employment, including prevocational training, agency-run business opportunities, and group and individual placements ( 41 ).
Overall, the samples and follow-up rates for employment outcomes, respectively, were 140 (98%), 150 (99%), 204 (100%), and 187 (96%) for the New Hampshire, DC, Hartford, and Chicago samples. Four participants had missing data on Social Security status, for a final sample of 677.
Social Security beneficiary status
On the basis of baseline interviews, participants were classified into one of four mutually exclusive categories: SSDI beneficiaries (receiving SSDI but no SSI), SSI beneficiaries (receiving SSI but no SSDI), dual eligibles (receiving both SSDI and SSI), and nonbeneficiaries (receiving no Social Security benefits).
Outcome variables
Two major outcomes of interest in this study were acquisition and retention of competitive employment. To standardize the outcome measures across the study, we used 18 months of follow-up data from all four studies. The acquisition of competitive employment at any time during the 18-month follow-up was coded dichotomously. Job retention was examined in two ways: one, total number of weeks worked on competitive jobs during the follow-up (referred to as "total weeks worked"), and two, number of weeks worked on the longest-held competitive job during the follow-up (referred to as "job tenure"). For job retention outcomes, zero weeks was entered for clients who never obtained a competitive job during the 18-month follow-up.
Data analysis
We conducted analyses using generalized linear models ( 48 ) implemented in SAS PROC GENMOD procedure ( 49 ). This modeling approach is an extension of traditional linear regression, which unifies seemingly disparate models for various types of data (continuous or dichotomous counts). For the acquisition of competitive work, we used the logistic regression model under the generalized linear model with the logit link function and binomial distribution; for total weeks worked and job tenure, we used the standard linear regression model under the generalized linear model with the identity link function and normal distribution of errors. Our primary objectives were to examine the associations between the three employment outcomes, the two treatment groups (individual placement and support versus the usual services control group), and the four benefit types.
For the inferential statistical analyses, we initially tested for possible site differences. Employment outcomes were stronger in the New Hampshire and Chicago sites than in the DC and Hartford sites for both individual placement and support and the control group. However, the statistical advantage of individual placement and support over the control group, measured in effect size, was comparable across sites. Because of these site differences, in subsequent analyses we treated group and benefit type as predictors but also included site in the models. We first examined three-way interaction models (examining interactions between group, benefit, and site) and found that the three-way interaction terms were not significant. We then fitted two-way interaction models (group × benefit, group × site, and benefit × site interactions) and found that two-way interaction terms were also not significant. Therefore, we present a main effects model with vocational service group and benefit type as predictors and site as a control variable.
After testing for overall significance, we conducted post hoc multiple comparisons within condition to compare employment outcomes for the four beneficiary groups using Tukey's adjustment and an alpha level of .05. Post hoc comparisons between the individual placement and support group and the control group were also conducted within each benefit type.
Finally, we computed effect size using Cohen's d statistic ( 50 ) for our key comparisons. For continuous outcome variables (total weeks worked and job tenure), effect size is the mean difference divided by the pooled standard deviation. For the dichotomous outcome variable (job acquisition), effect size was computed with the arcsine approximation ( 50 ).
Results
Sample characteristics of the individual placement and support group and the control group are shown in Table 1 . As expected, the two samples were well matched. The only exception was the finding of significantly more severe symptoms for the control group, which, however, reflected a small effect size (d=.20), not considered clinically significant. The Hartford study purposively sampled for Latinos and randomly assigned to the three groups (individual placement and support and two control groups), thereby accounting for the higher proportion of Latinos in the control groups in the combined sample.
 |
Shown in Table 2 are differences among beneficiary groups on background variables. At baseline, beneficiary groups did not differ on gender, marital status, or three clinical indicators: BPRS symptoms, days hospitalized, and substance abuse. The groups differed on several other variables, however. The SSDI group was the oldest and best educated. As expected, SSI recipients had the poorest work histories. SSI recipients were also more likely to be African American. Nonbeneficiaries had the best work histories. Compared with beneficiaries, they had a lower proportion of psychotic diagnoses, were younger, and were more likely to have been homeless in the prior year.
 |
Tables 3 , 4 , 5 show results for the three employment outcomes. Omnibus tests for service group and benefit type indicate significant overall group and benefit differences with respect to all three outcomes. Site was included as a control variable in all models. For all 12 comparisons between individual placement and support and control groups (four beneficiary groups × three employment outcomes), individual placement and support had significantly better outcomes than usual services. Moreover, ten of the 12 effect sizes were .73 or larger, reflecting moderately large to very large effects ( 51 ).
 |
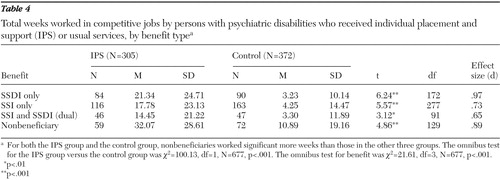 |
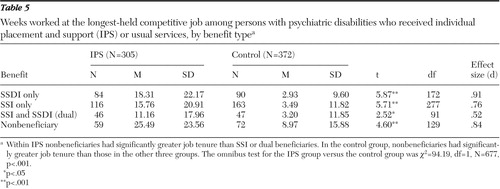 |
For most comparisons, employment outcomes were significantly lower for the three SSA beneficiary groups compared with the nonbeneficiary group. Among control groups, nonbeneficiaries had a higher rate of job acquisition than all three SSA beneficiary groups, although not so among individual placement and support participants. Pairwise post hoc comparisons among the beneficiary groups indicated that the nonbeneficiary group had more weeks worked and longer job tenure than each of the three SSA beneficiary groups within both the individual placement and support and the control samples, with one exception: the nonbeneficiary group did not differ on job tenure from the SSDI group within the individual placement and support sample.
Combining the three types of SSA beneficiaries into a single group, we calculated effect sizes for the differences between beneficiaries and nonbeneficiaries. Among those receiving individual placement and support, the effect sizes for the difference between beneficiaries and nonbeneficiaries were .28 for job acquisition, .56 for total weeks worked, and .45 for job tenure. In the control group, the corresponding effect sizes were .50 for job acquisition, .50 for total weeks worked, and .47 for job tenure. Thus five of six effect sizes comparing beneficiaries with nonbeneficiaries were in the moderate range.
Discussion
Our data indicate that evidence-based supported employment can enable SSA beneficiaries with severe mental illness and long-term disabilities to attain competitive work and maintain employment over time. Effect sizes for the IPS-control comparisons within benefit type were similar for the three employment outcomes, a finding that demonstrates that SSDI and SSI beneficiaries with severe mental illness attain a similar magnitude of benefit as nonbeneficiaries by enrolling in supported employment.
Although the focus of this report is on comparisons within benefit type, some readers may wonder about the clinical significance ( 52 ) of the work outcomes for participants in individual placement and support. Do the employment outcomes captured by the three indicators used in this report reflect meaningful levels of employment? A face-valid benchmark for meaningful employment is 20 hours per week of employment. In the total sample, 134 (44%) of individual placement and support participants obtained 20-hour-per-week positions, compared with 53 (14%) in the control group. A comprehensive individual placement and support review substantiates the clinical significance of individual placement and support employment outcomes across many indicators ( 36 ).
Another important question raised by this study is whether the disincentives for SSDI and SSI lead to differential patterns of employment. The SSDI program reinforces working below the earnings cutoff that triggers the trial work period, whereas the SSI program, after exclusions, reduces benefits by one-half the amount earned, even at relatively low earning levels. Both programs have implications for medical insurance. However, this study did not find differences between the two beneficiary groups on any of the outcome measures, so it provides no new insights on which might be better from a policy perspective. Our view is that both programs warrant changes to encourage beneficiaries to work to their full potential.
The limited data on long-term vocational outcomes and career trajectories of persons with psychiatric disabilities who receive supported employment suggest that time in employment improves over ten years but does not result in leaving SSA rolls ( 53 , 54 ). Because of the potential "benefits cliff" related to SSDI, it would be particularly valuable to study this group over longer time intervals. Leaving disability rolls may realistically require changes in insurance regulations, however, because individuals with chronic illnesses have great difficulty obtaining health insurance ( 7 ).
Mirroring the findings in prior studies ( 37 , 38 ), our findings indicated that the three SSA beneficiary groups had poorer employment outcomes than nonbeneficiaries. Background characteristics—especially work history, but also education and diagnosis—may partially explain some of these differences, although the four groups differed little on clinical factors such as symptoms, substance abuse, and time hospitalized. However, many lines of research also indicate that SSA regulations operate as a disincentive to return to competitive employment ( 55 , 56 , 57 ). For example, many applicants believe that applying for SSA benefits is the only way that they can obtain health insurance ( 23 ). It appears that individuals obtain SSA benefits to meet legitimate needs but then become socialized into further disability by the process and regulations ( 7 ). Intervening early in the illness process with evidence-based supported employment before individuals obtain disability payments may prevent long-term disability ( 58 , 59 ).
This analysis of data from supported employment studies was of course limited by self-selection because only psychiatric clients who entered randomized controlled trials of vocational rehabilitation were included. In addition, these studies of supported employment were focused on persons with severe mental illnesses, most of whom have long-term psychotic disorders such as schizophrenia and bipolar disorder, whereas a majority of SSDI beneficiaries with psychiatric disabilities are individuals with mood disorders. Thus these results may not apply to SSA beneficiaries in general or to SSDI beneficiaries with less severe disorders in particular.
SSA is currently sponsoring in 22 cities a national intervention study, the Mental Health Treatment Study, to examine the proposition that high-quality services (supported employment, systematic medication management, and other evidence-based practices) and enhanced health insurance will enable many SSDI beneficiaries with primary psychiatric disabilities to return to work (www.ssa.gov/disabilityresearch/mentalhealth.htm). The study will also determine what proportion of SSDI beneficiaries choose to enter a study of supported employment because beneficiaries in the 22 cities will be invited to participate by random selection from SSA rolls. Thus the Mental Health Treatment Study should provide more definitive answers to questions regarding return to work among SSDI beneficiaries with psychiatric disabilities.
Conclusions
SSA beneficiaries with psychiatric disabilities are a particularly important group for several reasons: they are the fastest-growing and largest disability group, they become disabled at a young age and remain on the rolls for many years, and yet most have fluctuating levels of impairment that trend toward improvement and functional recovery. Furthermore, recent developments in vocational rehabilitation technology have shown that a large proportion of this population have much greater employment potential than previously expected. The analysis of data from four studies of evidence-based supported employment presented here extends optimism that SSA beneficiaries with severe mental illness have excellent potential to return to competitive employment.
Acknowledgments and disclosures
Dr. Bond's time in preparing this article was supported by contract SS00-05-60072 from the Social Security Administration.
The authors report no competing interests.
1. Kouzis AC, Eaton WW: Psychopathology and the initiation of disability payments. Psychiatric Services 51:908–913, 2000Google Scholar
2. Ruiz-Quintanilla SA, Weathers RF, Melburg V, et al: Participation in programs designed to improve employment outcomes for persons with psychiatric disabilities: evidence from the New York WORKS demonstration project. Social Security Bulletin 66:49–79, 2006Google Scholar
3. Bond GR: Supported employment: evidence for an evidence-based practice. Psychiatric Rehabilitation Journal 27:345–359, 2004Google Scholar
4. Cook JA: Employment barriers for persons with psychiatric disabilities: update of a report for the President's Commission. Psychiatric Services 57:1391–1405, 2006Google Scholar
5. Drake RE, Becker DR, Goldman HH, et al: The Johnson & Johnson—Dartmouth Community Mental Health Program: disseminating evidence-based practice. Psychiatric Services 57:302–304, 2006Google Scholar
6. Barnett B, Born D, Katuin CH, et al: Moving Ahead Without Fear: Work, Benefits, and You. Anderson, Ind, Supported Employment Consultation and Training Center, 2005Google Scholar
7. Stobo JD, McGeary M, Barnes DK: Improving the Social Security Disability Decision Process: Final Report. Washington, DC, National Academies Press, 2006Google Scholar
8. Aron L, Burt M, Wittenburg D: Recommendations to the Social Security Administration on the Design of the Mental Health Treatment Study. Washington, DC, Urban Institute, 2005Google Scholar
9. Burt MR, Aron LY: Promoting Work Among SSI/DI Beneficiaries With Serious Mental Illness. Washington, DC, Urban Institute, 2003Google Scholar
10. McAlpine DD, Warner L: Barriers to Employment Among Persons With Mental Illness: A Review of the Literature. New Brunswick, NJ, Rutgers University, Center for Research on the Organization and Financing of Care for the Severely Mentally Ill, Institute for Health, Health Care Policy and Aging Research, 2000Google Scholar
11. Ferron DT: Diagnostic trends of disabled Social Security beneficiaries, 1986–93. Social Security Bulletin 58:15–31, 1995Google Scholar
12. Kennedy C, Manderscheid RW: SSDI and SSI disability beneficiaries with mental disorders, in Mental Health, United States. Edited by Manderscheid RW, Sonnenschein MA. Washington, DC, National Institute of Mental Health, 1992Google Scholar
13. Rupp K, Scott CG: Trends in the characteristics of DI and SSI disability awardees and duration of program participation. Social Security Bulletin 59:3–21, 1996Google Scholar
14. Estroff SE, Patrick DL, Zimmer CR, et al: Pathways to disability income among persons with severe, persistent psychiatric disorders. Milbank Quarterly 75:495–532, 1997Google Scholar
15. Massel HK, Liberman RP, Mintz J, et al: Evaluating the capacity to work of the mentally ill. Psychiatry 53:31–41, 1990Google Scholar
16. Zola IK: Self, identity, and the naming question: reflections on the language of disability. Social Science and Medicine 36:167–173, 1992Google Scholar
17. Mercer's Fax Facts Surveys: Behavioral Health and Disability. Baltimore, Mercer, 1998Google Scholar
18. Rosenheck RA, Leslie D, Keefe R, et al: Barriers to employment for people with schizophrenia. American Journal of Psychiatry 163:411–417, 2006Google Scholar
19. Rupp K, Scott C: Determinants of duration on the disability rolls and program trends, in Growth in Income Entitlement Benefits for Disability: Explanations and Policy Implications. Edited by Rupp K, Stapleton D. Kalamazoo, Mich, Upjohn Institute, 1998Google Scholar
20. Vocational Rehabilitation: Earnings Increased for Many SSA Beneficiaries After Completing VR Services, but Few Earned Enough to Leave SSA's Disability Rolls. No GAO-07-332. Washington, DC, US Government Accountability Office, 2007Google Scholar
21. Elinson L, Frey WD, Beemer MA, et al: Task 10: Demonstration Program Progress to Date: A Synthesis of Key Findings, Issues, and Lessons Learned. Report to Office of Disability and Employment Policy, US Department of Labor. Rockville, Md, Westat, 2005Google Scholar
22. MacDonald-Wilson KL, Rogers ES, Ellison ML, et al: A study of the Social Security work incentives and their relation to perceived barriers to work among persons with psychiatric disability. Rehabilitation Psychology 48:301–309, 2003Google Scholar
23. Mashaw JL, Reno VP: The Environment of Disability Policy: Programs, People, History, and Context. Washington, DC, National Academy of Social Insurance, 1997Google Scholar
24. Noble JH, Honberg RS, Hall LL, et al: A Legacy of Failure: The Inability of the Federal-State Vocational Rehabilitation System to Serve People With Severe Mental Illness. Arlington, Va, National Alliance for the Mentally Ill, 1997Google Scholar
25. O'Day BL, Killeen M: Does US federal disability policy support employment and recovery for people with psychiatric disabilities? Behavioral Sciences and the Law 20:559–583, 2002Google Scholar
26. Golden TP, O'Mara S, Ferrell C, et al: A theoretical construct for benefits planning and assistance in the Ticket to Work and Work Incentive Improvement Act. Journal of Vocational Rehabilitation 14:147–152, 2000Google Scholar
27. Kiernan WE, Halliday JF, Boeltzig H: Economic Engagement: An Avenue to Employment for Individuals With Disabilities. Preliminary Report. Boston, Institute for Community Inclusion, 2004. Available at www.communityinclusion.orgGoogle Scholar
28. Salkever DS, Karakus MC, Slade EP, et al: Measures and predictors of community-based employment and earnings of persons with schizophrenia in a multisite study. Psychiatric Services 58:315–324, 2007Google Scholar
29. Andrews H, Barker J, Pittman J, et al: National trends in vocational rehabilitation: a comparison of individuals with physical disabilities and individuals with psychiatric disabilities. Journal of Rehabilitation 58:7–16, 1992Google Scholar
30. Marshak LE, Bostick D, Turton LJ: Closure outcomes for clients with psychiatric disabilities served by the vocational rehabilitation system. Rehabilitation Counseling Bulletin 33:247–250, 1990Google Scholar
31. Burns T, Catty J, Becker T, et al: The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial in six European countries. Lancet, in pressGoogle Scholar
32. Crowther R, Marshall M, Bond GR, et al: Vocational rehabilitation for people with severe mental disorders. Cochrane Database of Systematic Reviews 2: CD003080, 2001Google Scholar
33. Crowther RE, Marshall M, Bond GR, et al: Helping people with severe mental illness to obtain work: systematic review. British Medical Journal 322:204–208, 2001Google Scholar
34. Twamley EW, Jeste DV, Lehman AF: Vocational rehabilitation in schizophrenia and other psychotic disorders: a literature review and meta-analysis of randomized controlled trials. Journal of Nervous and Mental Disease 191:515–523, 2003Google Scholar
35. Becker DR, Drake RE: A Working Life for People With Severe Mental Illness. New York, Oxford University Press, 2003Google Scholar
36. Bond GR, Drake RE, Becker DR: An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal, in pressGoogle Scholar
37. Jacobs HE, Wissusik D, Collier R, et al: Correlations between psychiatric disabilities and vocational outcome. Hospital and Community Psychiatry 43:365–369, 1992Google Scholar
38. Bond GR, Miller LD, Dietzen LL: Final Report on SSA Supported Employment Project for SSI/SSDI Beneficiaries With Serious Mental Illness. Grant no 12-D-70299-5-01. Washington, DC, Social Security Administration, 1992Google Scholar
39. Tremblay T, Smith J, Xie H, et al: Effect of benefits counseling services on employment outcomes for people with psychiatric disabilities. Psychiatric Services 57:816–821, 2006Google Scholar
40. Cook JA, Leff HS, Blyler CR, et al: Results of a multisite randomized trial of supported employment interventions for individuals with severe mental illness. Archives of General Psychiatry 62:505–512, 2005Google Scholar
41. Bond GR, Salyers MP, Dincin J, et al: A randomized controlled trial comparing two vocational models for persons with severe mental illness. Journal of Consulting and Clinical Psychology, in pressGoogle Scholar
42. Drake RE, McHugo GJ, Becker DR, et al: The New Hampshire study of supported employment for people with severe mental illness: vocational outcomes. Journal of Consulting and Clinical Psychology 64:391–399, 1996Google Scholar
43. Drake RE, McHugo GJ, Bebout RR, et al: A randomized clinical trial of supported employment for inner-city patients with severe mental illness. Archives of General Psychiatry 56:627–633, 1999Google Scholar
44. Mueser KT, Clark RE, Haines M, et al: The Hartford study of supported employment for persons with severe mental illness. Journal of Consulting and Clinical Psychology 72:479–490, 2004Google Scholar
45. Bond GR, Becker DR, Drake RE, et al: A fidelity scale for the Individual Placement and Support model of supported employment. Rehabilitation Counseling Bulletin 40:265–284, 1997Google Scholar
46. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
47. Overall JE, Gorham DR: Brief Psychiatric Rating Scale. Psychology Report 10:799–812, 1962Google Scholar
48. McCullagh P, Nelder JA: Generalized Linear Models. London, Chapman and Hall, 1989Google Scholar
49. SAS/STAT User's Guide, version 9. Cary, NC, SAS Institute Inc, 2003Google Scholar
50. Lipsey MW, Wilson DB: Practical Meta-Analysis. Newbury Park, Calif, Sage, 2000Google Scholar
51. Lipsey MW: Design Sensitivity. Newbury Park, Calif, Sage, 1990Google Scholar
52. Jacobson NS, Roberts LJ, Berns SB, et al: Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. Journal of Consulting and Clinical Psychology 67:300–307, 1999Google Scholar
53. Becker DR, Whitley R, Bailey EL, et al: Long-term employment outcomes of supported employment for people with severe mental illness. Psychiatric Services 58:922–928, 2007Google Scholar
54. Salyers MP, Becker DR, Drake RE, et al: Ten-year follow-up of clients in a supported employment program. Psychiatric Services 55:302–308, 2004Google Scholar
55. Averett S, Warner R, Little J, et al: Labor supply, disability benefits and mental illness. Eastern Economic Journal 25:279–288, 1999Google Scholar
56. Walls RT, Dowler DL, Fullmer SL: Incentives and disincentives to supported employment, in Supported Employment: Models, Methods, and Issues. Edited by Rusch FR. Sycamore, Ill, Sycamore, 1990Google Scholar
57. Warner R: Work disincentives in US disability pension programs. Journal of Mental Health 10:405–409, 2001Google Scholar
58. Nuechterlein KH, Subotnik KL, Ventura J, et al: Advances in improving and predicting work outcome in recent-onset schizophrenia. Schizophrenia Bulletin 31:530, 2005Google Scholar
59. Killackey E, Jackson HJ, McGorry PD: Results of the first Australian randomised controlled trial of Individual Placement and Support in first episode psychosis. Schizophrenia Bulletin 33:593, 2007Google Scholar



