Effects of Compulsory Treatment Orders on Time to Hospital Readmission
Abstract
To evaluate the effect of compulsory community treatment orders on subsequent time out of the hospital, the authors studied the admission dates of psychotic patients who had repeated hospitalizations in Quebec, Canada, and divided each admission according to its time in relation to the index admission, during which the judicial order was obtained. The data were stratified by type of admission (early, preindex, index, or postindex), and the hypothesis tested was that the median time to readmission would be greatest for the index admission. The hypothesis was confirmed, supporting previous findings that judicial orders that mandate severely ill psychotic patients to undergo compulsory community treatment are associated with decreased time spent in the hospital and thus increased personal freedom.
Compulsory community treatment orders can assist chronically psychotic individuals who are not adherent to treatment when they are discharged from hospitals to live in the community. Without such orders, these patients are more apt to become symptomatic or violent and to be reinstitutionalized (1,2,3,4,5,6). A randomized controlled trial by Swartz and colleagues (1,2) of compulsory community treatment orders showed that such patients had a significant reduction in admissions and mean duration of hospital stay compared with patients in a control group. In the context of public concern about violent acts performed by psychotic patients, the patients in their sample carried out and experienced significantly less violence than the control patients. One other randomized controlled study in New York did not confirm positive benefits of outpatient commitment (7), but there was no provision for enforcement of the order through pickup by the police.
In the study reported here, we examined the time until readmission before and after psychotic patients received an outpatient commitment order. This quasi-experimental design, with each patient serving as his or her own control, used survival analysis to compare times to readmission during a five-year period before and for at least 21 months of follow-up after the initiation of outpatient commitment. Because no experimental procedure was used and patients were otherwise treated in the usual way within the hospital-based system, this design reflects the effectiveness of this judicial procedure on the outcome of survival time until readmission. We selected a naturalistic, observational design that is ecologically valid in that it does not interfere in any aspects of patient treatment or follow-up. The trade-off is that it cannot address the issue of efficacy because of the absence of a control condition.
In the province of Quebec, Canada, a psychiatrist obtains a compulsory treatment order by petitioning a judge in the Superior Court. The pertinent section of the Quebec civil code states: "The authorization of the court is necessary where the person who may give consent to care … is incapable of giving his consent … or, without justification, refuses to do so. It is also required where a person … incapable of giving his consent categorically refuses to receive care, except in the case of hygienic care or emergency." The orders generally state that the patient must attend outpatient facilities for a two-year period and comply with the medications and treatment plan of the treating physician. If the patient does not comply with the order, the police are required by the order to bring the patient to the hospital for readmission.
Methods
The setting for this study was the SMBD Jewish General Hospital in Montreal. The sample included all consecutive patients from the hospital whom a judge ordered to submit to involuntary outpatient treatment in the two-year period July 1, 1998, to June 30, 2000. The last follow-up with the entire sample was on April 1, 2002. All patients in the catchment area receive outpatient, emergency, and inpatient services at the hospital. If they visit community health centers or other hospitals they are transferred back to their own hospital. This approach ensured that the data on hospitalizations were complete for the period under study. Outpatient treatment is free and readily available at the sector hospital for all patients in the Quebec Medicare system. Outpatient utilization data were not available for this study.
The sample included all consecutive hospital patients during a two-year period who received a compulsory community treatment order. The psychiatric inpatient admission during which the order was issued was designated the index admission. From the dates of admission and discharge, the number of days that the patient was maintained in the community after each admission was calculated. Each study participant's hospitalizations were divided into four groups: early hospitalizations, which included those in the previous five years before the preindex admission; the preindex admission, or the admission immediately before the index admission; the index admission; and any postindex admissions. All analyses were conducted with use of SAS version 8.2 for Windows PC. Survival analysis was conducted with PROC LIFETEST to examine the Kaplan-Meier estimates of the time to readmission or the end of the study (data censored). The hypothesis we tested was that the median time to readmission would be greatest for the index admission, in which the patient received a compulsory treatment order. Both log-rank and Wilcoxon statistics were used as appropriate.
Results
The sample comprised 42 patients, for whom the total number of admissions was 238. All patients were Caucasian, and 21 (48 percent) were women. The mean±SD age at last observation was 48.4±16.4 years (range, 22 to 82). In terms of chart diagnoses, 32 patients (76 percent) had one axis I disorder, and ten patients (24 percent) had two axis I disorders. These disorders included schizophrenia (23 patients, or 55 percent), bipolar disorder (nine patients, or 21 percent), schizoaffective disorder (eight patients, or 19 percent), substance use disorder (seven patients, or 17 percent), delusional disorder (three patients, or 7 percent), and organic mental disorders (one patient, or two percent). Nine patients (21 percent) had an axis II disorder, and 24 (57 percent) had at least one axis III disorder listed on the chart. Axis V diagnosis was not consistently available.
The median and mean times to readmission for all four types of admissions are shown in Table 1. The numbers for each type differ because not every patient had every type of admission. In a test of the differences in homogeneity of the survival curves for time to readmission across all four admission types, both the log-rank test (p<.0001) and the more conservative Wilcoxon (p=.0002) test indicated that the survival curves were not homogeneous across the total sample. The median and mean number of days until readmission (662 and 557 days, respectively) were the highest after the index admission during which the patient received a compulsory community treatment order. Time until readmission after the postindex admission was the next longest, followed by the early admissions, whereas the time to hospitalization after the preindex admission was the shortest.
A series of paired comparisons were carried out between the index admission and each of the other three admission types. Thus only patients who had both admission types were included in each analysis. The median time to readmission (199 days compared with 662 days) was 3.33 times as long for the index admission as for any early admission, which was significant by both the log-rank and Wilcoxon tests. The second analysis compared preindex and index admissions for patients who had both types of admission. The median time to readmission (128 days compared with 662 days) was 5.17 times as long for the index admission, which was highly significant by both tests. The third analysis examined only patients who were readmitted after their index admission. In this analysis the median time to readmission (137 days compared with 253 days) was only .65 times as long for the index admission as for the postindex admission. This difference was not significant according to the log-rank or Wilcoxon tests. Five of 21 individuals who had a postindex hospitalization were not included because they were still in the hospital, were transferred to a nursing home, or died in the hospital of medical causes.
Discussion
The principal finding in this study was that a compulsory community treatment order was associated with significantly increased periods free of hospitalization. Specifically, when all admission types were compared, the patients in the index admission group had the longest time until readmission. Our results complement and support the findings of Swartz and colleagues (1,2), although our study used a different design. Our concern that the results might have been biased because of the different numbers of patients with each type of admission was largely not borne out for the early and preindex comparisons with the index admission period. After compulsory treatment was initiated following the index admission, the same patients stayed out of the hospital 3.33 times as long as in their early admission period and 5.17 times as long as in the preindex admission period. By contrast, the return of the postindex admission group to a shorter time to readmission must be interpreted in the light of the fact that this group was a subgroup of 40 percent of the whole sample—a group that demonstrably had the most treatment-refractory illness.
Taking into account the quasi-experimental naturalistic design of this study, we conclude that compulsory treatment is effective overall for increasing the time out of the hospital.
Some might argue that it is the provision of additional ambulatory services and not the court order per se that accounted for the longer times out of the hospital in our sample. However, all patients in Quebec have equal, free, and ready access to the same spectrum and intensity of services that are offered. To our understanding, the main barrier to services for the patients we report on here was their own poor compliance or unwillingness to receive services. We do not have an "in-house" assertive community treatment team, but we use the assertive community treatment resources that are available in our network of community services as clinically indicated. Because of the severity of their illnesses and associated dangerousness, the patients under court orders in our system tend to receive the most attention and services available. The patients also are aware that the result of their missing appointments or injections of antipsychotics will result in their being brought by the police to the hospital for readmission. These "teeth" in the Quebec law (compared with many other jurisdictions) seem to result in enhanced compliance with treatment. Finally, no identifiable changes in access to or the nature of the psychiatric care delivery system, such as the institution of assertive community treatment teams, occurred during the duration of this study.
Weaknesses of this study include the relatively small sample, the lack of a randomized controlled design, the absence of outpatient service use data, and the lack of ability to differentiate noncompliant, "revolving-door" patients who respond to treatment from those whose illness is treatment refractory.
It was our impression that this mechanism seemed to assist patients to remain in ongoing treatment and to adhere to medication regimens more consistently than before their being subjected to the judicial order.
The data reported here appeared to be persuasive in the courtroom when the senior author solicited a compulsory treatment order. The judges seemed to be favorably influenced toward awarding such an order by learning that the patient in front of them would most likely benefit from increased time out of the hospital in exchange for the limited loss of liberty entailed by the order.
Penal psychiatric facilities in Quebec remain strapped for funds and resources. Consequently, general hospitals have had to treat increasingly violent patients. Thus there has been resistance on the part of the psychiatric staff and increased numbers of violent incidents.
Psychiatrists and nurses are more willing to assume responsibility for potentially dangerous patients only if a compulsory treatment order has been issued. Our clinical experience has been that the patients are less psychotic and dangerous when under the mandate of such an order. This fact, together with the data reported here in consideration of the particularities of the Quebec context, and the findings of Swartz and Swanson showing reduced violence under compulsory treatment orders (3,4,5,6), make us hesitant on clinical grounds to randomly assign dangerously psychotic patients to a "no-compulsory community treatment" control group.
Conclusions
By using each patient as his or her own control, we found that compulsory outpatient treatment was associated with a significant lengthening of the time until readmission compared with the previous five-year period. Although the study was quasi-experimental, the results are consistent with those of one other experimental study and suggest that compulsory community treatment is effective for most patients for whom it is obtained, resulting in increased time in the community until readmission. The implications of this study do not extend to the larger patient population who were not given a compulsory treatment order.
Dr. Frank, Dr. Perry, and Dr. Geagea are affiliated with the department of psychiatry at McGill University and with the SMBD Jewish General Hospital, 4333 Cote St. Catherine Road, Montreal, Quebec, Canada H3T 1E4 (e-mail, [email protected]). Maitre Kean is affiliated with St. Mary's Hospital in Montreal. Dr. Sigman is with the SMBD Jewish General Hospital.
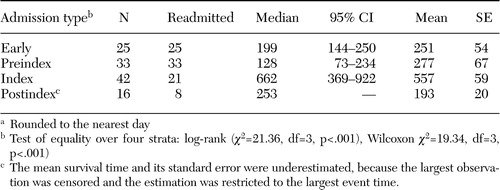 |
Table 1. Median and mean time to readmission (daysa) to the hospital for four types of admissions in a sample of 42 psychotic patients who received compulsory community treatment orders
aRounded to the nearest day
1. Swartz MS, Swanson JW, Wagner HR, et al: Can involuntary outpatient commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. American Journal of Psychiatry 156:1968–1975,1999Abstract, Google Scholar
2. Swartz MS, Swanson JW, Hiday VA, et al: A randomized controlled trial of outpatient commitment in North Carolina. Psychiatric Services 52:325–329,2001Link, Google Scholar
3. Swartz MS, Swanson JW, Hiday VA, et al: Violence and severe mental illness: the effects of substance abuse and non-adherence to medication. American Journal of Psychiatry 155:226–231,1998Abstract, Google Scholar
4. Swanson JW, Estroff S, Swartz MS, et al: Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry 60:1–22,1997Crossref, Medline, Google Scholar
5. Swanson JW: Mental disorder, substance abuse, and community violence: an epidemiological approach, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994Google Scholar
6. Swartz MS, Swanson JW, Hiday VA, et al: Taking the wrong drugs: substance abuse, medication non-adherence, and violence in severely mentally ill individuals. Social Psychiatry and Psychiatric Epidemiology 33:75–80,1998Crossref, Medline, Google Scholar
7. Steadman HJ, Gounis K, Dennis D, et al: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services 52:330–336,2001Link, Google Scholar



