Brief Reports: Outcomes of Patients in a Low-Intensity, Short-Duration Involuntary Outpatient Commitment Program
Abstract
This study examined the outcomes of patients in a low-intensity, short-duration involuntary outpatient commitment program. After release from inpatient commitment, one group (N=150) entered an involuntary outpatient commitment program that lasted up to six months; a comparison group (N=140) was released into the community without further involuntary care. After the analysis adjusted for confounding variables, patients who were in the involuntary outpatient commitment program had greater use of follow-up outpatient and residential services and psychotropic medications than patients in the comparison group. No differences were found between the groups in follow-up acute psychiatric hospitalization or arrests. Low-intensity, short-duration involuntary outpatient commitment appears to have a limited, but important, impact.
Involuntary outpatient commitment refers to court-ordered ambulatory treatment for persons with severe mental illness who are unlikely to adhere to care plans without external leverage (1). Typical implementations of involuntary outpatient commitment include its use as an alternative to hospitalization for patients who meet criteria for involuntary inpatient commitment (major psychiatric illness, with danger to self or others, or inability to meet basic needs) or as a step-down from inpatient treatment (conditional release) (2). Most states permit involuntary outpatient commitment, but the effectiveness of this type of commitment is debated (3,4).
Outpatient commitment has been examined in randomized, controlled trials in New York (5) and North Carolina (6). The former study showed that outpatient commitment had no impact on psychiatric rehospitalizations or arrests, but the latter study suggested that such commitment is effective when it lasts at least six months and intensive outpatient services are provided (6). Less is known about involuntary outpatient commitment programs that are shorter than six months and offer low-intensity services—that is, less than seven services per month on average (7). Brief, low-intensity commitment might reduce medication nonadherence, which occurs among up to 74 percent of patients with schizophrenia within two years of hospital discharge (8) and is associated with poor outcomes (9). Given current resource limitations, this topic is of considerable interest.
In Oregon, persons who are committed by the court are almost always placed in a hospital or locked residential facility. After discharge from inpatient care, some patients are released into the community without further commitment. Others are assigned to involuntary outpatient commitment (also known as the trial visit program) for up to 180 days. Patients' release from the locked facility may be contingent on their participation in the trial visit program, but assignment to this program often depends on staff availability.
The trial visit program includes a contract that the patient develops with a mental health monitor. Contracts can require living in a structured setting, outpatient treatment, medication, and abstinence from substance use. The monitor has regular contact with the patient and members of the patient's support network, including treatment providers. If the patient adheres to the contract, participation in the trial visit program can be terminated, but nonadherence can lead to a court hearing and hospital readmission.
Our hypothesis was that participants in the trial visit program would have more extensive nonhospital treatment and fewer adverse outcomes (acute psychiatric hospitalizations or arrests) than participants in the comparison group.
Methods
During the study period, 1995 through 1999, the Multnomah County trial visit program had approximately 100 clients each year. For our study, 30 clients aged 18 to 64 years were randomly chosen from each year's caseload, for a total of 150 participants in the trial visit program. Program archives also contained information on individuals who were civilly committed during the same period and were eligible to participate in the trial visit program but did not participate for various reasons: clinical (for example, dementia), personal (for example, refusal to participate), or logistical (for example, insufficient program capacity or funding). A total of 140 clients who did not participate in the trial visit program were randomly selected to create the comparison group. Whenever possible, clients were chosen for the comparison group if they did not participate in the trial visit program for logistical reasons. Participants were followed for an average of three years after index hospital discharge.
Data on the trial visit program were supplemented with county behavioral health clinical records that were abstracted by using an inpatient severity of psychiatric illness scale developed by Flynn and Henisz (10). The scale has been found to be reliable (interrater reliability generally exceeds .7 for trained raters). State databases provided information on outpatient mental health services, prescriptions, residential treatment, acute psychiatric hospitalizations, and arrests. The project was approved by the institutional review board of Oregon Health and Science University. Informed consent requirements were waived.
Bivariate analyses (chi square analysis and t tests) were used to compare participants in the trial visit program and in the comparison group. Cox proportional hazards survival analysis models were used to examine the times to certain outcomes, such as acute psychiatric hospitalizations or arrests. The date of discharge from the index hospitalization was the starting point for follow-up. Predictor variables in the Cox models included demographic characteristics, diagnoses, hospitalization history, and index Medicaid enrollment. Logistic and linear regressions were used to examine use of community mental health services and psychotropic medications with predictors similar to those in the Cox models. Analysis of covariance approaches (that is, regression models with interaction terms) were used to examine change in outcomes, such as acute psychiatric hospitalization.
Results
Table 1 displays the demographic characteristics, clinical history, follow-up services, and outcomes of the two groups. Bivariate analyses showed that, at the time of discharge from the index hospitalization participants in the two groups differed only in medication adherence before the index hospitalization. Participants in the trial visit program were more likely than those in the comparison group to have been nonadherent to medications at the time of the index hospitalization (76 percent compared with 50 percent).
Bivariate analysis of follow-up data showed some differences between the two groups. During the follow-up period, more participants in the trial visit program than in the comparison group used basic outpatient mental health services (72 percent versus 59 percent) for a greater percentage of follow-up months (36 percent compared with 23 percent). Also, a greater proportion of participants in the trial visit program used psychotropic medications (75 percent versus 63 percent) for a greater percentage of follow-up months (49 percent compared with 37 percent). In particular, a greater proportion of participants in the trial visit program used mood stabilizers (45 percent compared with 28 percent). Also, a greater proportion of participants in the trial visit program used antipsychotics (74 percent compared with 60 percent) for a greater percentage of follow-up months (45 percent compared with 34 percent).
Participants in the trial visit program were enrolled in Medicaid for a greater percentage of follow-up months compared with those in the comparison group (69 percent compared with 57 percent). Specifically, compared with participants in the comparison group, a greater proportion of participants in the trial visit program were in the medically needy disabled Medicaid category (28 patients, or 19 percent, compared with 12 patients, or 9 percent) for a greater percentage of follow-up months (a mean±SD of 12±29 percent compared with a mean of 4±15 percent). Additionally, participants in the trial visit program had more subacute (locked residential) admissions than those in the comparison group (overall admissions, 33 percent compared with 15 percent; involuntary admissions, 19 percent compared with 8 percent; and voluntary admissions, 19 percent compared with 9 percent). Participants in the trial visit group also used subacute residential services for a greater percentage of follow-up months (overall admissions, 2 percent compared with 1 percent; involuntary admissions, 1 percent compared with less than 1 percent; and voluntary admissions, no difference between groups). All differences remained significant after linear and logistic regression analyses adjusted for age, sex, race or ethnicity, and diagnosis (see Table 1).
On the other hand, there were no differences between the groups in acute inpatient psychiatric hospitalizations or in arrests during the follow-up period. Moreover, analysis of covariance approaches (that is, regression equations that included interaction terms) showed no differences between groups in change measures, such as those pertaining to acute inpatient psychiatric admissions. Cox proportional hazards regression models also showed no differences between groups in the time to first follow-up acute psychiatric hospitalization or in the time to first follow-up arrest. Although the small numbers of deaths precluded detailed analysis, all participants who died from suicide or other unnatural causes were in the comparison group.
Discussion and conclusions
Bivariate and regression analyses suggested that short-duration, low-intensity outpatient commitment had a positive impact on use of services among persons with serious mental illness who were leaving court-ordered inpatient psychiatric treatment. Even after the analyses adjusted for age, sex, race or ethnicity, and diagnosis, compared with participants in the comparison group, those in the trial visit program used significantly more outpatient mental health services, residential care, and psychotropic medications during follow-up.
However, these differences in service use did not extend to differences in follow-up acute psychiatric hospitalization or arrests. Moreover, changes in outcomes—such as acute psychiatric hospital admission—from before to after discharge from the index hospitalization did not differ between the groups. It could be that the trial visit program facilitated receipt of services by participants but the services had little or no impact on outcomes. Additionally, these outcomes are limited to measures of service use. Such process outcomes do not provide information on symptoms, quality of life, or client function during follow-up. Furthermore, in this observational study, participants in the trial visit program could have been more severely impaired than those in the comparison group, even though there were few (measured) differences at baseline. For example, clients may have been selected for the trial visit program on the basis of previous medication nonadherence or a perceived need for close monitoring. Alternatively, clients may have been selected for the trial visit program because it was perceived that they were able to comply with commitment contracts. Because this study was limited to available data, there may have been other differences between the two groups.
Sample sizes were adequate to detect clinically meaningful differences between groups. For example, there was 70 percent statistical power to detect a rehospitalization proportion difference of 15 percent, which is a small-to-medium effect size. It is also important to note that the data analysis used baseline measures (such as history of hospitalization) to predict outcome measures (such as readmission). In effect, this statistical approach allowed for comparison of "differences in differences," contrasting change in the trial visit program with change in the comparison group. No differences were found in these change measures. However, the study reported here was not a randomized trial.
The two randomized, controlled trials of involuntary outpatient commitment that were conducted also did not provide a clear answer on the effectiveness of such commitment. In the New York study, the experimental group was mandated by the court to receive 180 days of community services; 65 percent of those participants also received a 180-day renewal (5). The New York study showed no impact of involuntary outpatient commitment on treatment compliance, arrests, or psychiatric hospitalization. In the North Carolina study, clients who were mandated by the court to receive involuntary outpatient commitment were assigned to case management for a 90-day commitment, with a renewable 180-day extension (sustained commitment) (6). In the North Carolina study, a comparison of participants in the involuntary outpatient commitment group and those in the control group showed that overall the groups did not differ significantly in hospital outcomes. However, patients with sustained commitment had 57 percent fewer hospital admissions and 20 fewer days of hospitalization than those in the control group.
A recent review discussed the clinical implications of these randomized, controlled trials (7). Namely, involuntary outpatient commitment seems most effective when sustained for at least six months and when combined with frequent services. However, the review also acknowledged that the two studies showed inconsistent results and noted that the positive findings in North Carolina's sustained commitment group may not generalize to involuntary outpatient programs in other states.
The findings of this study are inconclusive regarding the effectiveness of the use of low-intensity, short-duration involuntary outpatient commitment when all outcome measures are considered. For example, this type of involuntary outpatient commitment may not reduce subsequent arrests or inpatient admissions, but it may reduce medication nonadherence and promote increased outpatient service use. Further research is needed to understand what programs will be most helpful to persons with severe mental illness who are involved with the involuntary treatment system and to determine how such services can be provided in an environment with markedly constrained resources.
Acknowledgments
This project was supported in part by the Medical Research Foundation of Oregon and the Stanley Foundation. The authors thank Shelby L. Haugan, M.D., and D. Ann Penaloza, M.D., for their invaluable assistance.
The authors are affiliated with the department of psychiatry at the Oregon Health and Science University in Portland. Dr. Pollack is also with the Office of Mental Health and Addiction Services in the Oregon Department of Human Services in Salem. Send correspondence to Dr. McFarland at Oregon Health and Science University, Department of Psychiatry, Mail Code CR-139, Portland, Oregon 97239 (e-mail, [email protected]).
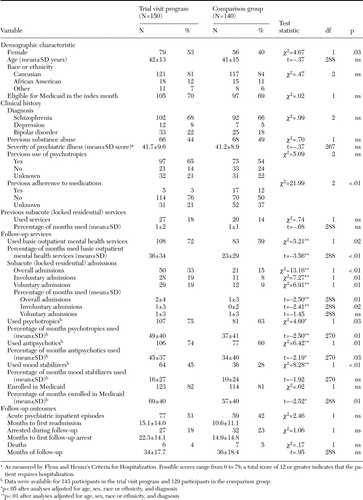 |
Table 1. Characteristics of persons with serious mental illness who completed court-ordered inpatient psychiatric treatment
1. Torrey EF, Kaplan RJ: A national survey of the use of outpatient commitment. Psychiatric Services 46:778–784,1995Link, Google Scholar
2. Monahan J, Swartz M, Bonnie RJ: Mandated treatment in the community for people with mental disorders. Health Affairs 22(5):28–38,2003Google Scholar
3. Appelbaum PS: Thinking carefully about outpatient commitment. Psychiatric Services 52:347–350,2001Link, Google Scholar
4. Hiday VA: Outpatient commitment: the state of empirical research on its outcomes. Psychology, Policy, and Law 9:8–32,2003Crossref, Medline, Google Scholar
5. Steadman HJ, Gounis K, Dennis D, et al: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services 52:330–336,2001Link, Google Scholar
6. Swartz MS, Swanson JW, Hiday VA, et al: A randomized controlled trial of outpatient commitment in North Carolina. Psychiatric Services 52:325–329,2001Link, Google Scholar
7. Swartz MS, Swanson JW: Involuntary outpatient commitment, community treatment orders, and assisted outpatient treatment: what's in the data? Canadian Journal of Psychiatry 49:585–591,2004.Google Scholar
8. Weiden PJ, Olfson M: Cost of relapse in schizophrenia. Schizophrenia Bulletin 21:419–429,1995Crossref, Medline, Google Scholar
9. Swartz MS, Swanson JW, Hiday VA, et al: Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. American Journal of Psychiatry 155:226–231,1999Google Scholar
10. Flynn HR, Henisz JE: Criteria for psychiatric hospitalization: experience with a checklist for chart review. American Journal of Psychiatry 132:847–850,1975Link, Google Scholar



