Stigma as a Barrier to Recovery: Adverse Effects of Perceived Stigma on Social Adaptation of Persons Diagnosed With Bipolar Affective Disorder
Abstract
OBJECTIVE: The purpose of this study was to evaluate the effect of concerns about stigma on social adaptation among persons with a diagnosis of bipolar affective disorder. METHODS: The sample comprised 264 persons who were consecutively admitted to a psychiatric inpatient or outpatient service at a university-affiliated hospital and who met research diagnostic criteria for bipolar I disorder, bipolar II disorder, or schizoaffective disorder, manic type. Patients were evaluated with use of the Schedule for Affective Disorders and Schizophrenia, Lifetime Version (SADS-L), the Brief Psychiatric Rating Scale (BPRS), and a measure of perceived stigma. Social adjustment was measured at baseline and seven months later with the Social Adjustment Scale (SAS). RESULTS: As predicted, patients who had concerns about stigma showed significantly more impairment at seven months on the social leisure subscale but not on the SAS extended family subscale, after baseline SAS score and symptom level had been controlled for. More refined models using SAS-derived factors as dependent variables indicated that concerns about stigma predicted higher avoidance of social interactions with persons outside the family and psychological isolation at seven-month follow-up, after baseline SAS and BPRS scores had been controlled for. CONCLUSIONS: Concerns about the stigma associated with mental illness reported by patients during an acute phase of bipolar illness predicted poorer social adjustment seven months later with individuals outside the patient's family. Greater attention to patients' concerns about stigma is needed from both researchers and clinicians.
Research over the past four decades has compellingly demonstrated that individuals diagnosed as having mental illness are socially stigmatized or discriminated against on several dimensions by key individuals in their social networks and communities (1). For example, studies have found that employers (2,3,4), families of patients (5), mental health workers (6), and prospective landlords (7) all endorsed devaluing statements about or discriminated against mentally ill individuals. The degree of stigmatization has been found to be positively associated with the manifest severity of the mental disorder (8); however, even persons who have minimal signs of mental illness, that is, those who appear "troubled," may be stereotyped and rejected (9).
Link and colleagues (10,11) have argued that because persons with mental illness internalize the devaluing or discriminatory attitudes of society at large, they anticipate discrimination or rejection by others and develop coping strategies, such as secrecy about their illness or withdrawal from social interaction, in an effort to avoid the rejection they anticipate. Goffman (12) has suggested that to avoid discrimination and rejection, persons with mental illness may limit their social interaction to individuals who are similarly stigmatized or who are aware and accepting of the stigma—for example, family members.
To test Goffman's theory, Link and colleagues (11) evaluated the association between reports of withdrawal from social interaction by persons with mental illness in response to concerns about stigma and their reliance on individuals inside their households rather than those outside for emotional and practical support. As predicted by Goffman's theory, they found that reports of withdrawal in response to concerns about stigma were positively associated with reliance on individuals within the household for support but were negatively associated with reliance on individuals outside the household. In other words, persons with mental illness who reported avoiding social interaction to avoid exposure to rejection because of their mental illness also indicated that they turned to members of their own family rather than to persons outside the family for emotional and practical support.
One implication of these findings is that the adoption of coping strategies that reduce the stigmatized person's range of social contacts—for example, withdrawal—may in fact further handicap social adaptation and delay recovery or limit the prospects of recovery. To investigate this possibility, we evaluated the impact of concerns about stigma among persons with a diagnosis of bipolar affective disorder on their social adaptation over time within and outside of the family.
Most studies of the stigma associated with mental illness have focused on persons with schizophrenia or chronic mental illness; however, there are indications that persons with bipolar illness may also be exposed to stigma (13). On the basis of findings from previous studies, we hypothesized that strong concerns about stigma at baseline would predict impaired social functioning over time among persons diagnosed as having bipolar illness. We further predicted that after baseline social functioning had been controlled for, concerns about stigma would be found to have a more serious impact on patients' social interaction with individuals outside their families than on their interaction with family members.
Methods
Subjects
The sample comprised 264 persons aged 16 years or older who were consecutively admitted to a university-affiliated psychiatric inpatient or outpatient service and who had a lifetime diagnosis of bipolar depression with mania (bipolar I disorder), hypomania (bipolar II disorder), or schizoaffective disorder, manic type, according to research diagnostic criteria (14). Because the study was carried out as part of a study on family burden in bipolar illness (15), only patients whose family members consented to be studied were included. Fifty-seven percent of eligible patients agreed to participate. Additional details about sample selection are available elsewhere (15). Institutional review board approval was obtained for this study, and all the participants gave informed consent.
Patients were enrolled in the study between October 1993 and September 1995; seven-month follow-up data were collected approximately through April 1996. The attrition rate over the seven-month follow-up period was 20 percent. A comparison of the socioeconomic and clinical characteristics of the participants who remained in the study at seven months with those lost to follow-up found that the latter were more likely to be inpatients at baseline (χ2=4.52, df=1, p=.03). No other significant differences were found.
Measures
Baseline assessments were conducted within one week of discharge from the index inpatient admission or within one week of entry into a new episode of outpatient care. The Schedule for Affective Disorders and Schizophrenia, Lifetime Version (SADS-L) (16) was used to establish lifetime diagnosis and to rate the nature of the patient's index episode of illness—manic versus depressed. The expanded version of the Brief Psychiatric Rating Scale (BPRS) (17), developed by Lukoff and colleagues (18) to incorporate the psychotic and affective symptoms associated with bipolar disorder, was used to evaluate symptom severity. The 24-item, interviewer-administered instrument uses a 7-point scale on which 1 indicates not present and 7 indicates extremely severe. Possible scores range from 7 to 168. An intraclass correlation coefficient was calculated for the four raters on the basis of two videotaped interviews, using all 24 items. Coefficients for tape 1 were .83, .82, .85, and .96; for tape 2, coefficients were .88, .87, 1, and .90. Internal consistency for the expanded BPRS was acceptable (Cronbach's alpha=.76).
Patients' concerns about stigma were evaluated with use of a scale composed of eight items that measure withdrawal as a coping mechanism designed to avoid rejection (10) and 12 items from Link's Beliefs About Devaluation-Discrimination Scale (11). Withdrawal was measured by asking the respondents to indicate the extent to which they agreed with statements such as "It is easier for me to be friends with people who have been psychiatric patients" and "After being in psychiatric treatment, it is a good idea to keep what you are thinking to yourself."
Beliefs about devaluation and discrimination were measured by having the respondents report the extent to which they agreed with statements such as "Most people feel that entering a mental hospital is a sign of personal failure" and "Most employers will pass over the application of a former mental patient." All statements were rated on a 4-point scale with anchors ranging from "agree strongly" to "disagree strongly." The scale demonstrated adequate internal consistency (Cronbach's alpha=.83).
The interview version of the Social Adjustment Scale (SAS) (19) was used at baseline and at seven-month follow-up to evaluate participants' adaptive social functioning over the previous three months. The extended family subscale and the social leisure subscale of the SAS were used to evaluate participants' adaptive social functioning with their family and with their broader social network, respectively. The extended family subscale assesses the quality of the respondent's relationships with his or her parents, siblings, in-laws, and children living away from home along eight dimensions: friction, reticence, withdrawal, dependency, rebelliousness, worry, guilt, and resentment. The social leisure subscale assesses the quantity and quality of social interactions outside the family, including the number of close friends and social interactions and the experienced degree of friction, social discomfort, hurt feelings, boredom, loneliness, and ease of confiding.
The global ratings made immediately after the interview were used to measure these dimensions of social adaptation over the previous three months and to assess overall adjustment during this time frame. Patients were rated on 7-point Likert scales on which 1 indicates excellent adjustment and 7 indicates very severe maladjustment. The SAS marital and parental subscales, which assess relationships with spouses and children living at home, respectively, were not included in this study, because only a relatively small number of patients had spouses and children. The work subscale was not used, because it combines data on adjustment within the family—for example, functioning as a homemaker—with data on adjustment outside the family—for example, adaptation to competitive employment—and thus precludes examination of our hypothesis on the effects of stigma on social adaptation with family members compared with others.
Analyses
Bivariate correlations were calculated with the Pearson r product-moment correlation coefficient to identify sociodemographic variables and clinical characteristics—for example, inpatient versus outpatient and bipolar spectrum diagnosis—associated with the outcome variables for inclusion in the multivariate models. Of all the variables evaluated, only the participant's marital status and BPRS score at baseline were significantly correlated with any of the measures of social adjustment; these were included in the multivariate models described below.
Multiple regression models were then run with each of the three global measures of social adjustment as an outcome variable. In each model, the corresponding baseline value for that dimension of social functioning, the total BPRS score at baseline, the total stigma score at baseline, and the patient's marital status were entered simultaneously to identify the contribution of the stigma variable to social outcome while controlling for the effects of other potential explanatory factors.
To further evaluate significant findings from the initial regression analyses, the seven-month item-level data from the global scales were subjected to a principal components analysis, and additional, exploratory models were run by using the resulting factor scores as dependent variables. This analytic strategy enabled us to specify more precisely the dimensions in social adjustment at seven months that were affected by the patients' perceptions of stigma at baseline. In these models the global score for the relevant domain was used to control for the effects of baseline functioning on seven-month adaptation.
Results
Sample characteristics
Demographic and clinical characteristics of the sample are presented in Table 1. Most of the participants were white, female, and single. Most had a primary diagnosis of bipolar I disorder and a relatively large number of psychiatric inpatient admissions. Onset of the illness had occurred at a relatively early age. All the participants met criteria for a current affective episode at baseline—49 percent for a manic spectrum episode and 51 percent for a depressive spectrum episode. About two-thirds were inpatients when they entered the study. The participants' mean±SD BPRS score at baseline was 39.42±10.34. The mean global ratings assigned on the SAS at baseline and at seven-month follow-up, respectively, were 3.02±1.25 and 2.83±1.15 for the extended family subscale, 3.49±1.41 and 3.27±1.36 for the social leisure subscale, and 3.91±1.14 and 3.58±1.21 for the overall adjustment subscale.
Predictors of social adjustment: global scales
As Table 2 shows, concerns about stigma significantly predicted adjustment at seven-month follow-up as measured on the social leisure subscale (b=.151, t=2.37, df=177, p= .019), even after symptom level, baseline functioning, and sociodemographic covariates had been controlled for. By contrast, concerns about stigma at baseline were not a significant predictor of social adjustment at seven months on the SAS extended family subscale, either before or after symptom level and baseline functioning in this domain had been controlled for. Thus, as hypothesized, individuals who reported higher levels of concern about stigma at baseline had more impaired social functioning in interactions with persons outside their family but not in interactions with family members.
The effect of stigma in the model predicting seven-month functioning on the overall adjustment subscale was not significant. Baseline social adjustment was a significant predictor of functioning at seven months in all three domains. Conversely, marital status and baseline BPRS score, although significant at the bivariate level, were not significant predictors in any domain, after baseline social adaptation had been controlled for.
Factor analysis and exploratory models
The principal components analysis for the SAS social leisure subscale produced three orthogonal factors. Factor 1, psychological isolation, had high loadings (greater than .50) on social discomfort, loneliness, and boredom. Factor 2, behavioral avoidance, had high loadings on diminished contacts, reticence, and diminished interactions. Factor 3, rejection sensitivity, had high loadings on friction and hypersensitivity. Together the three factors explained 53.7 percent of the cumulative variance.
As Table 3 shows, the regression models that used the three seven-month social leisure scale factors as dependent variables demonstrated that stigma concerns at baseline were positive and significant predictors of psychological isolation and behavioral avoidance. Baseline social leisure functioning was also a positive and significant predictor of both factors, whereas baseline BPRS scores predicted poorer functioning on the psychological isolation factor alone. Interestingly, a participant's marital status was differentially related to the psychological isolation and behavioral avoidance factors. Being married predicted decreased psychological isolation but increased behavioral avoidance seven months after the index episode of illness.
Discussion
The findings of this study demonstrate that concerns about stigma associated with mental illness reported by persons diagnosed as having bipolar affective disorder during an acute phase of their illness adversely affected an aspect of their social adaptation seven months later. As predicted, patients with strong concerns about stigma at baseline showed greater impairment in their subsequent social and leisure functioning, even after symptom severity, baseline social adaptation, and sociodemographic characteristics had been controlled for.
This study was designed in part to test the hypothesis that stigma-related impairment in social adaptation results from avoidant coping strategies, such as secrecy and withdrawal (11), that patients use to minimize their exposure to discrimination from individuals outside their family or peer group. As hypothesized, we found that concerns about stigma were associated with poorer functioning on the SAS social leisure subscale, which evaluates relationships with individuals outside the family, but not with functioning on the extended family subscale, which evaluates relationships within the family.
Our data thus represent an extension of the cross-sectional findings of Link and colleagues (11) to a different patient sample, to additional dimensions of social functioning, and to a longitudinal time frame. The finding that concerns about stigma were not associated with poorer functioning on the SAS overall adjustment subscale, which is a composite general measure of social adaptation, further supports the hypothesis that stigma specifically compromises social functioning in nonfamily relationships.
Of particular interest are the results of the factor analysis of the social leisure subscale, which identified three different dimensions of social dysfunction in interactions with individuals outside the family. Regression analyses using these refined dimensions may help to elucidate the specific ways in which persons with concerns about stigma adapt their social behavior to avoid exposure to rejection or discrimination. These analyses found that such concerns predicted social dysfunction in two of the three dimensions: psychological isolation and behavioral avoidance. Psychological isolation was associated with being single and having a higher symptom severity; behavioral avoidance was associated with being married. These findings suggest that these strategies may be employed by different subgroups of patients.
Additional research is needed to replicate the findings of this study and to clarify the ways in which concerns about stigma and coping strategies affect social behavior outside the family. Although the findings are consistent with our hypothesis that patients exercise avoidant coping strategies selectively in anticipation of rejection by individuals outside the family, an alternative explanation of the results is that family members compensate for their ill relatives' social deficits in ways that people outside the family do not.
Future research might address this alternative explanation by considering the impact of the family's attitudes and behavior toward the ill relative on his or her concerns or behavior in coping with stigma as well as the potential contribution of family members' own concerns about stigma (5). Sociocultural factors other than stigma that may influence the social adjustment of persons with mental illness should also be investigated.
A limitation of this study was that it did not address social adaptation relative to employment or members of the immediate family. Future studies should examine the impact of concerns about stigma on social functioning in these areas.
The impairment in social and leisure functioning associated with concerns about stigma has implications for the health and well-being of persons diagnosed as having bipolar illness. First, the extent and quality of social interactions have an important bearing on quality of life (20,21). Second, research on social support has consistently shown that the absence of close or confiding relationships is associated with greater risk of relapse or nonremission among individuals with depression (22,23,24,25). Because chronic symptoms of depression are associated with greater risk of medical illness (26), the adverse impact of stigma on social functioning could affect the physical health of persons diagnosed as having mental illness.
Although our findings underscore the need for interventions to reduce the adverse impact of stigma for persons with bipolar disorders and other mental illnesses, the results of previous studies suggest that such interventions need to be developed with caution. For example, the results of national surveys indicate that most people prefer to maintain a social distance from individuals who have a mental illness (9); therefore, interventions that attempt to counter the social withdrawal of people with mental illness may, paradoxically, expose them to more experiences of rejection.
One possible strategy to alleviate this concern might be to link interventions for stigma with existing models for promoting the recovery of persons with mental illness, such as supported employment (27). This strategy would provide individuals with an opportunity to recognize and respond to discrimination or rejection within the supportive framework of the program, where they can rely on peers or professionals to support and guide them. Such a buffered exposure might help inoculate them against the adverse effects of future experiences of discrimination or rejection.
Research on interventions also must consider the individual cognitive biases and coping styles that individuals employ. For example, studies have demonstrated that some stigmatized persons may preferentially attribute rejection and other negative outcomes of stigma to internal factors—for example, ability—in order to protect self-esteem or perceived social control (28). The results of the factor analyses in our study suggest that persons with bipolar disorders have more than one way of coping with concerns about stigma in social situations outside the family. Because it is possible that different modes of coping with stigma are differentially associated with mental health and well-being over time, empirical research using a factor analytic approach might help identify the more adaptive modes and thus inform research on interventions.
Conclusions
The Surgeon General's report on mental health (29) noted that stigma "is among the many barriers that discourage people from seeking treatment" for their condition. We found that concerns about stigma also serve as a barrier to meaningful social interactions with persons outside patients' own families. Thus our study highlights the importance and potential benefits to consumers of reducing the stigma associated with mental illness. To achieve this goal and promote optimal functioning for persons with mental illness, innovative research is needed to develop effective intervention strategies that do not unduly expose them to rejection and discrimination. At the same time, mental health practitioners, families, and consumer advocates must join to promote more widespread efforts to educate the public about mental illness.
Acknowledgment
This study was supported by grant MH-51348 from the National Institute of Mental Health.
Dr. Perlick and Dr. Rosenheck are with the Northeast Program Evaluation Center at the Veterans Affairs Medical Center in West Haven, Connecticut, and Yale University School of Medicine in New Haven. Dr. Clarkin and Dr. Sirey are with the department of psychiatry of the New York Presbyterian Hospital, Westchester Division, of the Joan and Sanford I. Weill Medical College of Cornell University in White Plains, New York. Ms. Salahi is in the master's program at the Social Work School of the University of Connecticut in West Hartford. Dr. Struening and Dr. Link are with the epidemiology of mental disorders program at Columbia University and New York State Psychiatric Institute in New York City. Send correspondence to Dr. Perlick, Northeast Program Evaluation Center, Department of Veterans Affairs, VA Connecticut Healthcare System, 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]). This paper is part of a special section on stigma as a barrier to recovery from mental illness.
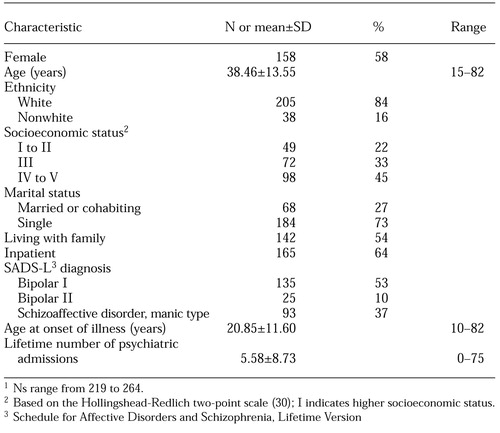 |
Table 1. Characteristics at baseline of individuals diagnosed as having mental illness who participated in as study of the effects of concerns about stigma on social functioning1
1Ns range from 219 to 264
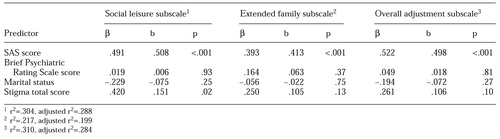 |
Table 2. Baseline predictors of study participants' scores on subscales of the Social Adjustment Scale (SAS) at seven-month follow-up
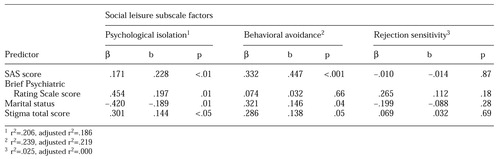 |
Table 3. Baseline predictors of study participants' scores on the social leisure subscale of the Social Adjustment Scale (SAS) at seven-month follow-up
1. Link BG, Phelan JC: Labeling and stigma, in The Handbook of the Sociology of Mental Health. Edited by Aneshensel CS, Phelan JC. New York, Kluwer Academic/ Plenum, 1999Google Scholar
2. Farina A, Felner RD: Employment interviewer reactions to former mental patients. Journal of Abnormal Psychology 82:268-272, 1973Crossref, Medline, Google Scholar
3. Olshansky S, Grob S, Malamud IT: Employer's attitudes and practices in hiring of ex-mental patients. Mental Hygiene 42:391-401, 1958Medline, Google Scholar
4. Farina A, Murray PJ, Groh T: Sex and worker acceptance of a former mental patient. Journal of Consulting and Clinical Psychology 46:887-891, 1978Crossref, Medline, Google Scholar
5. Struening EL, Perlick DA, Link BG, et al: The extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services 52:1633-1638, 2001Link, Google Scholar
6. Cohen G, Struening EL: Opinions about mental illness in the personnel of two large mental hospitals. Journal of Abnormal and Social Psychology 64:349-360, 1962Crossref, Medline, Google Scholar
7. Page S: Effects of the mental illness label in attempts to obtain accommodations. Canadian Journal of Behavioral Science 9:84-90, 1977Crossref, Google Scholar
8. Farina A: Are women nicer people than men? Sex and the stigma of mental disorders. Clinical Psychology Review 1:223-243, 1981Crossref, Google Scholar
9. Link BG, Phelan JC, Bresnahan M, et al: Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health 89:1328-1333, 1999Crossref, Medline, Google Scholar
10. Link BG, Cullen F, Struening EL, et al: A modified labeling theory approach in the area of the mental disorders: an empirical assessment. American Sociological Review 54:400-423, 1989Crossref, Google Scholar
11. Link BG, Cullen F, Frank J, et al: The social rejection of ex-mental patients: understanding why labels matter. American Journal of Sociology 92:1461-1500, 1987Crossref, Google Scholar
12. Goffman E: Stigma: Notes on Management of Spoiled Identity. Englewood Cliffs, NJ, Prentice-Hall, 1963Google Scholar
13. Fadden G, Bebbington P, Kuipers L: Caring and its burdens: a study of the spouses of depressed patients. British Journal of Psychiatry 151:660-667, 1987Crossref, Medline, Google Scholar
14. Spitzer RL, Endicott J, Robins E: Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry 35:773-782, 1978Crossref, Medline, Google Scholar
15. Perlick D, Clarkin JF, Sirey J, et al: Burden experienced by caregivers of persons with bipolar affective disorder. British Journal of Psychiatry 174:56-62, 1999Crossref, Medline, Google Scholar
16. Endicott J, Spitzer RL: A diagnostic interview: Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry 35:837-844, 1978Crossref, Medline, Google Scholar
17. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799-812, 1962Crossref, Google Scholar
18. Lukoff D, Nuechterlein KH, Ventura J: Manual for the expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594-602, 1986Google Scholar
19. Weissman MM: The Depressed Woman: A Study of Social Relationships. Chicago, University of Chicago Press, 1974Google Scholar
20. Lehman AF: A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 11:51-62, 1988Crossref, Google Scholar
21. Rosenheck R, Evans D, Herz L, et al: How long to wait for a response to clozapine: a comparison of time course of response to clozapine and conventional antipsychotic medication in refractory schizophrenia. Schizophrenia Bulletin 25:709-719, 1999Crossref, Medline, Google Scholar
22. Sherbourne CD, Hays RD, Wells KB: Personal and psychological risk factors for physical and mental health outcomes and course of depression among depressed patients. Journal of Consulting and Clinical Psychology 63:345-355, 1995Crossref, Medline, Google Scholar
23. Cronkite RC, Moos RH, Twohey J, et al: Life circumstances and personal resources as predictors of the ten-year course of depression. American Journal of Community Psychology 26:255-279, 1998Crossref, Medline, Google Scholar
24. George LK, Blazer DG, Hughes DC, et al: Social support and the outcome of major depression. British Journal of Psychiatry 154:478-485, 1989Crossref, Medline, Google Scholar
25. Dean A, Kolody B, Wood P: Effects of social support from various sources on depression in elderly persons. Journal of Health and Social Behavior 31:148-161, 1990Crossref, Medline, Google Scholar
26. Salovey P, Rothman AJ, Detweiler JB, et al: Emotional state and physical health. American Psychologist 55:110-121, 2000Crossref, Medline, Google Scholar
27. Drake RE, McHugo GJ, Bebout RR, et al: A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Archives of General Psychiatry 56:627-633, 1999Crossref, Medline, Google Scholar
28. Crocker J, Major B, Steel C: Social stigma, in The Handbook of Social Psychology, 4th ed. Edited Gilbert D, Fiske S, Lindzey G. New York, McGraw-Hill, 1998Google Scholar
29. Mental Health: A Report of the Surgeon General. Washington, DC, US Department of Health and Human Services, US Public Health Service, 1999Google Scholar
30. Hollingshead A, Redlich FC: Social Class and Mental Illness: A Community Study. New York, Wiley, 1958Google Scholar



