Correlates of Health Insurance Among Persons With Schizophrenia in a Statewide Behavioral Health Care System
Abstract
This study explored the demographic and service use correlates of insurance status among 539 persons with schizophrenia-spectrum disorders by using the administrative data set of a statewide behavioral health care system. Lack of health insurance was prevalent in the sample (20 percent) and was associated with younger age, Latino ethnicity, and male sex. Persons who did not have insurance were less likely to use a community-based service and more likely to use only crisis or emergency services than persons who had public or private insurance. The findings are consistent with the results of previous research demonstrating that lack of insurance is associated with decreased use of community-based services among persons with severe mental illness.
A growing body of research has documented the problem of underinsurance among persons with severe mental illness in the United States (1,2,3,4,5,6,7). Studies indicate that insurance status is a major predictor of service use in this population, with lack of health insurance strongly associated with a lower likelihood of using community-based mental health services and a greater reliance on emergency services (2,3,4,5,6,7). Estimates of the proportion of persons with severe mental illness who lack health insurance in the United States range from 18 percent to 44 percent (2,3,4,5,6,7).
Previous studies of the relationship between service use and insurance status among persons with severe mental illness have been hampered by certain limitations. Two studies relied on secondary analyses of community surveys (2,7) in which data on insurance status, diagnosis, and service use were based on self-report and were of questionable validity. Another major study examined a cohort of persons presenting for a first psychiatric admission in a primarily white suburban community, and thus the results may not be generalizable to other settings (5,6). Other reports have not described the demographic characteristics associated with insurance status in this population (2,7).
The purpose of the study reported here was to explore the demographic and service use correlates of insurance status in a sample of persons with a diagnosis of a schizophrenia-spectrum disorder by using the administrative data set of a statewide behavioral health care system. This data set has the advantage of providing diagnostic, health insurance, and service use data that are based on administrative claims and that are therefore more reliable than self-reported data. Although the sample was limited to persons who had presented for services, the service system covers a range of sectors, including emergency, fee-per-visit outpatient, intensive case management, and day treatment services, and thus provides a broad snapshot of persons presenting for ambulatory treatment. In addition, the system of care serves diverse ethnic, racial, and socioeconomic groups, and findings are likely to generalize to other settings.
We hypothesized that, consistent with previous research findings (5), demographic characteristics would vary by insurance status. We also hypothesized that insurance status would predict service use and that, also consistent with previous research findings (2,3,4,5,6,7), persons who did not have insurance would be more likely than other persons to rely on crisis services than community-based services.
Methods
Data on diagnosis, demographic characteristics, and service use were extracted from the administrative data set of a public-sector behavioral health service system located in a Northeastern state. The service system is the largest behavioral health provider in the state and serves all the state's major regions. Data were drawn from administrative records of all persons who were admitted with a diagnosis of a schizophrenia-spectrum disorder (DSM-IV codes 295.xx) between January 1, 2000, and August 31, 2002. This period was selected because the administrative data set became active on January 1, 2000, and the last date for which complete data were available at the time of data extraction was August 31, 2002. All service use that occurred within the system of care during the study period was recorded in the database. Of 25,048 persons who were admitted to the service system during the study period, 569 had a diagnosis of a schizophrenia-spectrum disorder.
Data on payer source were recoded to create three categories of insurance status: public insurance (Medicaid, Medicare, or both), private insurance, and no insurance. Data on insurance status were available for 539 individuals (95 percent of the total sample). Of these 539 persons, 296 (55 percent) had public insurance, of whom 142 (26 percent) had Medicaid and 154 (29 percent) had Medicare as their primary payer (data on secondary insurance was not available); 134 (25 percent) had private insurance; and 109 (20 percent) had no insurance. Differences in demographic characteristics and service use by insurance status were examined by using analysis of variance and chi square tests; statistical significance was set at .05.
Results
Demographic characteristics and service use by insurance status are summarized in Table 1. An association was found between demographic characteristics and insurance status: persons with no insurance were likely to be younger than those who were covered by public or private insurance and were more likely to be male. Latino persons, although they accounted for a relatively small proportion of the overall sample, were highly concentrated among the uninsured (43 percent of all Latino persons in the sample had no insurance). Persons with private insurance were more likely to be white than persons with public or no insurance.
Analyses of service use focused on any use of a given type of service during the study period. This approach was chosen because individual duration of treatment varied depending on when persons were admitted into the sample, which made comparisons of duration of treatment less meaningful. Overall, mean duration of treatment for outpatient services was 203.4±226.3 calendar days, and mean service duration for day treatment was 278.4±242.8 calendar days. As can be seen from Table 1, study participants who had private insurance were significantly more likely to use fee-per-visit outpatient services than persons who had public or no insurance. Use of crisis or emergency, intensive case management, and acute day treatment services did not vary significantly by insurance status. Use of continuing day treatment services was significantly greater among persons with public insurance, who were almost twice as likely to use this service modality as persons with private or no insurance.
We also examined overall use of any community-based service, defined as any use of the services studied except for crisis or emergency services, and whether crisis services were the only type of service used by the individual. Although the vast majority of the sample did use a community-based service, those who did not have insurance were less likely than those with public or private insurance to use any community service and more likely to use only crisis services. A multivariate logistic regression predicting use of only crisis or emergency services examined whether this difference could be explained by the demographic characteristics associated with lack of insurance. Predictor variables included insurance status (no insurance versus insurance), race or ethnicity (white versus not white), age, and sex. Lack of insurance significantly predicted the use of only crisis services, even when the other variables were controlled for (odds ratio=1.78, Wald F=4.36, df=1, 4, p=.037).
Discussion
The results of this study indicated that, even in a treated sample, lack of insurance is relatively common among persons with a schizophrenia-spectrum disorder. The proportion of study participants who had no insurance (20 percent) was strikingly similar to what has been observed in studies that used different methods (2,4,6). Lack of health insurance was found to be associated with age, gender, and race or ethnicity. Alarmingly, close to half of the Latino persons in the sample had no health insurance. Young men with a minority background appear to be especially at risk of not having health insurance in this population.
Findings on service use confirmed that persons who had no health insurance used many types of services, including outpatient care and intensive case management. Nevertheless, this group was more likely than others to use only emergency services. Although the study participants who did not have insurance differed demographically from those who did, demographic differences did not explain this difference in service use when they were examined in a multivariate model. These findings indicate that uninsured persons may be more likely to present for services only during a crisis situation without following up on referrals for continued treatment and may then exit the system. These individuals may be at a higher risk of "falling through the cracks" of the service system. However, this interpretation should be made with caution, because it is possible that these persons received subsequent outpatient services from another provider.
Study participants who had either private insurance or no insurance were less likely to use continuing day treatment services than those who had public insurance. This difference may reflect difficulty obtaining reimbursement from private and charity payers for this high-intensity service. However, persons who had private insurance tended to be more likely to use fee-per-visit outpatient services than others, which gave them an overall rate of use of community-based services that was comparable to that of persons who had public insurance. Participants who did not have insurance did not use any more outpatient services than those who had public insurance and therefore lagged behind in their overall use of community-based services.
One alternative explanation for these study findings is that insurance type is related to severity of symptoms and that these differences might explain differences in service use. To address this possibility we examined differences in mean scores on the 32-item Behavior and Symptom Identification Scale (BASIS-32) for the three insurance groups. BASIS-32 is a self-report checklist of symptoms and functioning administered to clients on admission to the system of care whenever possible. BASIS-32 data were available for 287 study participants—167 (58 percent) who had public insurance, 70 (24 percent) who had private insurance, and 50 (17 percent) who had no insurance. Our analyses revealed no significant differences or trends between the three insurance groups in scores on any of the BASIS-32 symptom or functioning scales, which suggests that differences in symptoms probably do not explain the differences we observed in service use.
This study had some important limitations. The findings apply only to persons receiving treatment. However, research from community surveys indicates that only 50 to 60 percent of persons with severe mental illness receive treatment in a given year (8). Thus our findings do not provide information about how insurance status relates to the likelihood of receipt of any treatment. Furthermore, the data were limited to service use within the system of care studied. Although there is no reason to anticipate that the use of services outside the system would vary by insurance status, it is possible that some of the study participants received outpatient services from another provider.
Conclusions
On the whole, the findings of this study, consistent with the results of other research, suggest that insurance status has a substantial impact on the use of mental health services among persons with severe mental illness. In particular, lack of insurance was common and was associated with lower use of day treatment services and a greater likelihood of using only crisis and emergency services. The findings support the view that efforts to increase access to the public insurance safety net—that is, Medicaid and Medicare—would be an important step in reducing gaps in the provision of services to persons with severe mental illness (1,9).
Acknowledgments
The authors thank William Vega, Ph.D., for his support and guidance in directing the analyses and David Mechanic, Ph.D., for his helpful comments on an earlier draft.
Dr. Yanos is affiliated with the department of psychiatry at the University of Medicine and Dentistry of New Jersey-New Jersey Medical School in Newark and the Behavioral Research and Training Institute of University Behavioral Healthcare in Piscataway. Dr. Lu is with the New Hampshire-Dartmouth Psychiatric Research Center in Concord. Dr. Minsky and Dr. Kiely are with the quality improvement division of University Behavioral Healthcare in Piscataway. Send correspondence to Dr. Yanos at UMDNJ-UBHC, Behavioral Health Sciences Building, 183 South Orange Avenue, Newark, New Jersey 07103 (e-mail, [email protected]).
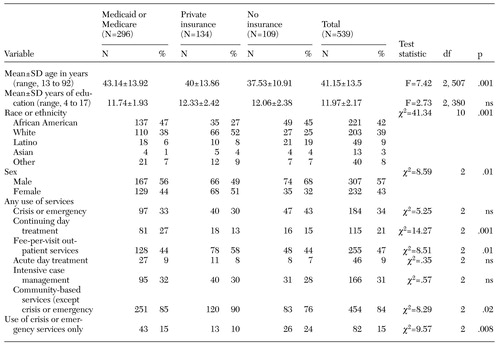 |
Table 1. Demographic characteristics and service use by insurance type in a sample of patients with schizophrenia-spectrum disorders
1. Rupp A: Underinsurance for severe mental illness. Schizophrenia Bulletin 17:401–405, 1991Crossref, Medline, Google Scholar
2. McAlpine DD, Mechanic D: Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Services Research 35:277–292, 2000Medline, Google Scholar
3. Landerman LR, Burns BJ, Swartz MS, et al: The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. American Journal of Psychiatry 151:1785–1790, 1994Link, Google Scholar
4. National Advisory Mental Health Council: Health care reform for Americans with severe mental illnesses: report of the National Advisory Mental Health Council. American Journal of Psychiatry 150:1447–1465, 1993Link, Google Scholar
5. Rabinowitz J, Bromet EJ, Lavelle J, et al: Relationship between type of insurance and care during the early course of psychosis. American Journal of Psychiatry 155:1392–1397, 1998Link, Google Scholar
6. Rabinowitz J, Bromet EJ, Lavelle J, et al: Changes in insurance coverage and extent of care during the two years after first hospitalization for a psychotic disorder. Psychiatric Services 52:87–91, 2001Link, Google Scholar
7. McAlpine DD, Mechanic D: Payer source for emergency room visits by persons with psychiatric disorders. Psychiatric Services 53:14, 2002Link, Google Scholar
8. Kessler RC, Berglund PA, Bruce ML, et al: The prevalence and correlates of untreated serious mental illness. Health Services Research 36:987–1007, 2001Medline, Google Scholar
9. Mechanic D: Closing gaps in mental health care for persons with serious mental illness. Health Services Research 36:1009–1017, 2001Medline, Google Scholar



