Changes in Insurance Coverage and Extent of Care During the Two Years After First Hospitalization for a Psychotic Disorder
Abstract
OBJECTIVE: This study examined changes in insurance coverage during the 24 months after first admission for a psychotic disorder and the relationship of insurance type to the extent of care. METHODS: The sample consisted of 443 persons who were enrolled in the Suffolk County (New York) Mental Health Project. Information about coverage—private insurance, Medicaid-Medicare, or no insurance—was obtained from hospital records and interviews. The insurance status groups were compared to examine differences in the percentage of days they received inpatient, outpatient, and day hospital care. Results and CONCLUSIONS: The proportion of persons with no insurance decreased from baseline to 24 months, from 42 percent to 21 percent. The proportion of persons with private insurance remained similar, 42 and 37 percent. The proportion of those with Medicaid-Medicare increased from 15 percent to 42 percent. Of those with Medicaid-Medicare at baseline (67 persons), 88 percent had such coverage 24 months later. Of those with private insurance at baseline (188 persons), 73 percent had the same coverage 24 months later. Of those with no insurance at baseline (188 persons), 35 percent had no insurance at 24 months, 54 percent had Medicaid-Medicare, and 11 percent had private insurance. Over the 24 months, the Medicaid-Medicare group had the most days of care, the private insurance group had the least inpatient care, and those with no insurance were least likely to receive outpatient care. There was a linear relationship between receiving more outpatient care and spending less time in the hospital and the day hospital.
Many persons with psychotic disorders lack health insurance coverage at the time of their first psychiatric hospitalization. Previously we found that 44.6 percent of 525 persons included in a countywide study lacked health insurance at the time of their first admission, 14.9 percent had Medicaid or Medicare, 38.9 percent had private insurance, and 1.5 percent were insured by the Department of Veterans Affairs (1). Data were unavailable to examine whether the participants maintained coverage after the first admission. Self-report data for persons with severe mental disorders from the National Comorbidity Survey, more than 80 percent of whom had private or government insurance, suggest that insurance coverage may increase over time (2).
Given the alarmingly high proportion of persons who do not have insurance at the time of the first psychiatric hospitalization and the importance of health insurance coverage for obtaining care, the study reported here examined changes in coverage during the two years after first admission and the relationship between the type of insurance coverage and the extent of care. We also examined reasons why some persons lacked or lost insurance.
Methods
Sample and procedure
Data were from the Suffolk County Mental Health Project. The design of the Suffolk County study has been described elsewhere (3). Briefly, the overall sample included 695 presumed psychotic patients hospitalized in one of the 12 psychiatric facilities in Suffolk County, New York, between September 1989 and December 1995. Respondents were interviewed in person six months and 24 months after their hospitalization and by telephone at three-month intervals in between.
Patients included in the study were 15 to 60 years of age. All were residents of Suffolk County. When they were hospitalized, the patients all showed clinical evidence of psychosis, were taking neuroleptic medications, or had a diagnosis from another facility indicating psychosis. Patients who had a first psychiatric hospitalization more than six months before the current admission were excluded, as were those with moderate or severe mental retardation and those who could not speak English.
The response rate for the initial interview was 72 percent. Of the 695 persons interviewed at baseline, 11 died before the 24-month interview, 30 were dropped after the six-month diagnostic review because they no longer met inclusion criteria, 26 were lost to follow-up, and 48 refused to be interviewed. Thus a total of 580 persons remained in the study for the full 24 months, which represents 88 percent of eligible respondents.
After written consent for the baseline interview was obtained, written permission was obtained from respondents to review their medical records and to interview the treating clinician and significant others.
Diagnosis and course
Consensus diagnoses were derived after the six-month interview using all available clinical information and the Structured Clinical Interview for DSM-III-R (SCID) (4), which was administered at baseline and at six and 24 months. Interrater reliability was in the acceptable-to-excellent range (5). Other sources of information were interviews with clinicians and significant others and hospital discharge summaries.
This analysis is based on the 443 respondents for whom complete insurance information was available at baseline, six months, and 24 months. At six months the diagnoses were schizophrenia spectrum disorder, 168 persons (38 percent); bipolar disorder with psychotic features, 128 persons (29 percent); major depressive disorder with psychotic features, 89 persons (20 percent); and other nonorganic psychoses, 58 persons (13 percent).
Measures
Five demographic variables were analyzed: age, gender, race, marital status, and household socioeconomic status. Education was not included in this analysis because many respondents were young adults who had not finished their education. Household socioeconomic status was rated by applying the Hollingshead 7-point occupational scale to the person who contributed the most financially to the household in which the respondent lived at baseline.
Service utilization data were extracted from responses to the mental health contact inventory developed for the Suffolk County Mental Health Project, which was completed at each six-month interview. The inventory includes the number of contacts for monthly inpatient, day hospital, and outpatient care according to information provided by respondents and treatment records that are routinely requested for all respondents.
Insurance data
Six categories were considered for insurance status: staff model health maintenance organization (HMO), preferred-provider arrangement, fee-for-service arrangement, Medicaid or Medicare, Veterans Affairs (VA), and no insurance. This information as well as information about reasons for not having insurance was obtained from multiple sources, including admission and discharge records, hospital billing records, responses to a questionnaire on insurance by the patient and a significant other, employment history, and interviewers' narratives.
The most informative data sources for insurance type at baseline were hospital admission and discharge records. One hospital made billing records available. Data were obtained from hospital records for 438 persons. For the remaining patients, we relied on information provided by significant others and the respondents themselves. Hospital data were compared with the information obtained from interviews with patients and significant others. In the few cases in which insurance status remained unclear, patients' records were further reviewed for other information, such as employment history, that might help determine whether the person was insured and, if so, what type of insurance it was. Not all respondents were hospitalized during the 24-month follow-up period. Thus the determination of insurance status was based more on the reports of respondents and significant others than on hospital records. The interrater reliability of insurance coding was checked by having 50 randomly selected records recoded by a second rater. Raters agreed on all but five cases.
Analysis
In a preliminary analysis of the data, we found that only one respondent was a member of a staff model HMO and that two were insured by the VA. For half of the persons with private insurance, it was difficult to determine whether coverage was in a preferred-provider or a fee-for-service arrangement. The primary reason for the difficulty was that some insurers provided both types of coverage, and in many cases the respondents themselves were not sure of the type of arrangement by which they were covered; in other cases insurance information came only from hospital records. Thus HMO, preferred-provider arrangements, and fee-for-service arrangements were combined into the category of private insurance.
Four respondents had Medicare only, and nine had both Medicare and Medicaid. Respondents were therefore stratified into three groups: private insurance, Medicaid or Medicare; and no insurance. Two respondents with VA coverage were dropped from the analysis.
Changes in insurance status were mapped by contingency table analysis. Reasons for not having insurance are presented descriptively.
To test the association between type of insurance and extent of care, the average number of days of inpatient care, day hospitalization, and outpatient care for each six-month interval were calculated and also summed to create an index indicating the percentage of days with care. In addition, a binary variable was created indicating whether or not the respondent received any outpatient care.
To examine the extent to which care varied by insurance type at six and 24 months, we used one-way analysis of variance. We controlled for age, socioeconomic status, gender, marital status, race, and diagnosis. As in our previous study (1), our preliminary analysis found that these variables were related to obtaining care. The association between receiving outpatient care and insurance status was examined with logistic regression, using the same control variables as in the one-way analysis of variance. We also examined the correlations between outpatient, inpatient, and day hospital care. To test the hypothesis that obtaining more outpatient care would result in the use of less inpatient and day hospital care, we included all three variables in a multiple regression equation in which we also included the same control variables as in previous analyses.
Results
Insurance status over 24 months
Table 1 presents data on insurance status at baseline and at six and 24 months. The proportion of respondents with no insurance decreased from 42 percent at baseline to 21 percent at 24 months. The proportion with private insurance remained about the same, 42 percent at baseline and 37 percent at 24 months. The proportion covered by Medicaid or Medicare increased, from 15 percent at baseline to 42 percent at 24 months.
Of the 188 persons with no insurance at baseline, 65 (35 percent) had no insurance at 24 months, 102 (54 percent) were covered by Medicaid or Medicare, and 21 (11 percent) were covered by private insurance. Of the 188 respondents with private insurance at baseline, 73 percent had such coverage 24 months later. Of the 67 persons with Medicaid or Medicare at baseline, 88 percent had such coverage 24 months later.
Reasons for not having insurance
Ninety-two persons did not have insurance at the 24-month interview. The reasons they gave could be grouped into four categories. Fifty-three persons (58 percent) held jobs that did not provide insurance. Fourteen (15 percent) were ineligible for Medicaid or Medicare because of technicalities; for example, the amount of financial aid some persons received exceeded the Medicaid limits. Eleven (12 percent) apparently were too ill to apply for Medicaid or Medicare; for example, one paranoid respondent made frequent moves, and another paranoid respondent had delusions about the government that precluded her from applying for Medicaid. A third respondent with severe phobia could not cope with contacting the Department of Social Services. The other 14 respondents had miscellaneous reasons: nine were without insurance apparently by choice, and two said they were about to start work and would be getting insurance through work. For three respondents no reason could be determined.
Males were more likely than females to have no insurance (odds ratio=1.5, 95% confidence interval=1.01 to 2.5). No discernible differences were found in age, gender, marital status, or diagnosis in reasons for having no insurance.
Extent of care
Information on the extent and type of care received under different insurance arrangements is presented in Table 2. During the first six-month interval, the Medicaid-Medicare group had the largest proportion of persons receiving any type of care, and persons in this group received the most days of care. These differences were statistically significant. On average, persons in the Medicaid-Medicare group had some kind of care—inpatient, outpatient, or day hospital—during almost a third (31 percent) of the days during the first six months. The number of days of care for this group is about 12 percent higher than for the group with private insurance and the group with no insurance; persons with private insurance and with no insurance received care on about 19 percent of the days in the first six-month period.
For the six months preceding the 24-month follow-up, all groups experienced a substantial reduction in care. The Medicaid-Medicare group received the most care, and the group with no insurance experienced the greatest decline in care.
At six months the private insurance group had more outpatient care (7.8 percent of the days) than the Medicaid-Medicare group (6 percent) and the group with no insurance (5.9 percent). At 24 months the Medicaid-Medicare group had slightly more outpatient care than the other groups.
At six months outpatient care accounted for 41 percent of care for the private insurance group, compared with 33 percent for the Medicaid-Medicare group and 30 percent for the group with no insurance. At 24 months the proportion of outpatient care for the private insurance group increased to 67 percent. The proportion for the Medicaid-Medicare group remained about the same at 37 percent. The proportion increased for the group with no insurance from 30 percent to 51 percent.
As Table 2 shows, the private insurance group had the smallest proportion of inpatient days of care, followed by the group with no insurance. The Medicaid-Medicare group received the most day hospital care and the no insurance group the least.
For the Medicaid-Medicare group, we found a negative correlation between outpatient and inpatient care (six months: r=-.35, p<.001, N=161; 24 months: r=-.21, p=.008, N=167) and between outpatient care and day hospital care (six months: r=-.38, p<.001, N=161; 24 months: r=-.23, p=.003, N=169). A similar trend was noted for the other two insurance groups. No significant correlations were found between day hospital and inpatient care.
When inpatient care and day hospital care were used together in a multiple regression equation predicting outpatient care, we found that after age, diagnosis, and gender were controlled for, inpatient care and day hospital care explained 26 percent of the variance in outpatient care at six months (R2=.26; day hospital: b=-.37, t=5.43, df=159, p<.001; inpatient: b= -.36; t=5.27, df=159, p<.001; N=161). These two variables also explained about 10 percent of the variance in outpatient care at 24 months (R2=.09; day hospital: b=-.23, t=3.08, df=167, p=.002; inpatient, b=-.21; t=2.70, df= 167, p=.007; N=169). These results suggest that outpatient care may reduce the need for inpatient care.
At six months more than 92 percent of each group had obtained at least some outpatient care. However, by 24 months the proportion of respondents with no insurance who received outpatient care decreased 35 percent—from 92 percent to 57 percent. The proportion of those with private insurance receiving outpatient care fell 27.7 percent—from 98 percent to 70 percent. However, the proportion of respondents in the Medicaid-Medicare group who received outpatient care at 24 months remained similar to the proportion at six months—84 percent and 93 percent, respectively.
The odds of getting outpatient care at either six months or 24 months were significantly higher for those with private insurance than for those with no insurance (OR=1.8, CI=1.1 to 3.1; N=109). The odds were also higher for those in the Medicaid-Medicare group than for those with no insurance (OR=4.1, CI=2.3 to 7.4; N=152).
Longitudinal perspective
We conducted a longitudinal analysis of changes in the percentage of days with care to complement the cross-sectional analysis in Table 2. Persons who had the same insurance coverage at six and 24 months were compared with those whose insurance arrangement changed. Five major paths from six months to 24 months were found. In two of them the insurance arrangement changed: 35 persons with no insurance changed to Medicaid-Medicare, and 17 persons with private insurance at six months had no insurance at 24 months. In three of the paths, there was no change in status. At both six and 24 months, 140 persons had private insurance, 144 persons had Medicaid-Medicare, and 62 persons had no insurance. We examined the effect of gaining and losing coverage compared with maintaining the same coverage. For this analysis a difference score was calculated for each respondent for each type of care for six- and 24-month intervals.
An analysis of covariance controlling for levels of care at six months, age, gender, diagnosis, and socioeconomic status revealed no significant differences among the five groups described above in total days of care at 24 months. For all groups, the number of outpatient days of care decreased by about 11 percent between six and 24 months. The adjusted mean differences for outpatient care showed a trend toward significance (p=.09). For persons who remained on Medicaid-Medicare, the percentage of days per month of outpatient care changed very little, by .02 percent. For the other groups, the percentage declined. For those who changed from no insurance to Medicaid-Medicare, the decrease was 1.4 percent. For those who kept private insurance, it was 2.4 percent. For those who were not insured at both time points, the decrease was 4.2 percent, and for those who changed from private insurance to no insurance, it was 5.2 percent.
For the five groups, the adjusted mean differences for inpatient care were significant (F=2.50, df=4, 355, p=.04). The persons who shifted from no insurance to Medicaid-Medicare had the smallest decrease in inpatient care, 10.3 percent. For those covered by Medicaid-Medicare at both time points, inpatient care fell 15 percent. For those with private insurance at six months and no insurance at 24 months, the decrease was 18 percent. The decrease was 22 percent for those not insured at both follow-ups. And for those who maintained their private insurance over the 24 months, inpatient care fell 22 percent. No significant difference in day hospital care was found for the five groups.
Discussion and conclusions
Of 443 persons who experienced a first admission for a psychotic disorder, 20 percent appeared not to have health insurance two years after the admission. In addition, some who had insurance at the time of admission lost coverage over the two-year period. The results also suggest that having some kind of insurance is associated with more outpatient care.
Like many working Americans, about 60 percent of the persons in this study who had no insurance did not have it because their jobs did not provide it. These individuals with severe mental disorders were cut off from needed services by virtue of trying to work and improve their level of functioning. This catch-22 situation works against psychiatric patients. Also troubling is that a large group without insurance were not able to obtain Medicaid or Medicare because of apparently minor deviations from eligibility criteria. It is also noteworthy that about 10 percent of respondents were apparently too ill to apply for help. Ways should be found to help such persons get needed Medicaid and Medicare. Some states have appointed an ombudsman to help persons obtain coverage. The patients in this sample were in the early course of psychotic illness, and thus none of them had lost coverage for having exceeded lifetime limits. The issue of lifetime limits has been of major concern and has led to legislation for parity in limits between mental and physical health coverage.
Our findings on insurance coverage at six and 24 months are almost identical to those in the National Comorbidity Survey, which indicated that more than 80 percent of persons with severe mental disorders had private or government insurance (2). Given the substantial differences in methods between the two studies, the similarity in results is surprising and supports the generalizability of the findings of the Suffolk County study.
As in other studies (6), we found that persons with no insurance were less likely to receive outpatient care. Our previous analysis of the baseline data from this cohort produced similar findings (1). Like others (7), we found that persons who received outpatient care used less inpatient and day hospital care, suggesting that ambulatory care for this vulnerable population may have a protective effect. These findings also suggest that easy access to generous outpatient care might reduce the need for and use of costly hospital care. These findings and others like them provide important support for insurers' allowing easy access to generous outpatient care.
The study had some limitations. The analysis did not control for the type of private insurance, such as preferred-provider and fee-for-service arrangements, and the type of coverage, which is known to vary and which is often inadequate for mental health care (8,9). These factors could have affected the extent of care. Another limitation is that some persons obtained insurance to get care, whereas others may have been in a treatment setting that helped them apply for insurance, especially Medicaid or Medicare. Thus the direction of association between having insurance and obtaining care may not always be obvious.
Future studies should examine insurance coverage of persons who have other serious mental disorders and who are not psychotic. In addition, although we had follow-up data on 89 percent of eligible respondents, it is possible that the insurance or care situation differed among the 11 percent for whom data were missing. We will continue to examine data on the insurance status and treatment of this cohort through the 48-month follow-up to examine changes in care that may have occurred as Medicaid moves to a managed care arrangement.
Acknowledgments
This research was supported in part by grant 44801 from the National Institute of Mental Health and a Young Investigator Award from the National Alliance for Research on Schizophrenia and Affective Disorders to Dr. Rabinowitz. The authors thank the project psychiatrists who formulated the psychosis diagnoses, including Drs. Charles Rich, Shmuel Fennig, Marsha Tanenberg-Karant, Gerardo Tolentino, Joan Rubinstein, Noam Eitan, Ranganathan Ram, and Kinga Koreh. They also thank Sharon L. Zariello, M.S.W., who assisted in the collating of insurance information.
Dr. Rabinowitz is affiliated with Bar Ilan University, Ramat Gan, Israel (e-mail, [email protected]). The other authors are affiliated with the State University of New York at Stony Brook.
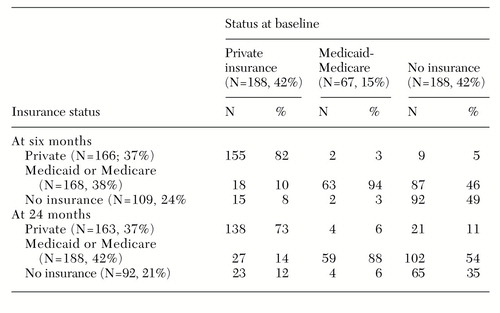 |
Table 1. Insurance status six and 24 months after initial hospital admission of 443 persons with psychotic disorders, as a function of status at baseline
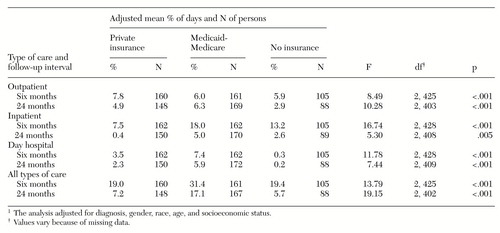 |
Table 2. Adjusted mean percentage of days that 443 persons received three types of care during six- and 24-month follow-up periods after a first hospitalization for a psychotic disorder, by insurance status
1. Rabinowitz J, Bromet EJ, Lavelle J, et al: Relationship between insurance type and care during early course of psychosis. American Journal of Psychiatry 155:1392-1397, 1998Link, Google Scholar
2. National Advisory Mental Health Council: Health care reform for Americans with severe mental illnesses. American Journal of Psychiatry 150:1447-1465, 1993Link, Google Scholar
3. Bromet EJ, Schwartz JE, Fennig S, et al: The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophrenia Bulletin 18:243-255, 1992Crossref, Medline, Google Scholar
4. Spitzer RL, Williams JBW, Gibbon M, et al: The Structured Clinical Interview for DSM-III-R (SCID): I. history, rationale, and description. Archives of General Psychiatry 49:624-629, 1992Crossref, Medline, Google Scholar
5. Bromet EJ, Jandorf L, Fennig S, et al: The Suffolk County Mental Health Project: demographic, pre-morbid, and clinical correlates of 6-month outcome. Psychological Medicine 26:953-962, 1996Crossref, Medline, Google Scholar
6. Landerman LR, Burns BJ, Swartz MS, et al: The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. American Journal of Psychiatry 151:1785-1790, 1994Link, Google Scholar
7. Lehman AF, Steinwachs DM, and co-investigators of the PORT project: At issue: translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
8. Sharfstein SS: The role of private insurance in financing treatment for depression. Social Psychiatry and Psychiatric Epidemiology 30:236-239, 1995Medline, Google Scholar
9. Stoline AM, Sharfstein SS: Funding the continuum of care: a rational social policy for the care and support of persons with schizophrenia, in Handbook of Mental Health Economics and Health Policy, vol 1. Edited by Moscarelli M, Rupp A, Sartorious N. Chichester, England, Wiley, 1996Google Scholar



