The Feasibility of Enhancing Psychiatric Outpatients' Readiness to Change Their Substance Use
Abstract
OBJECTIVE: This stage I therapy development study evaluated the feasibility and acceptability of a brief motivational intervention for outpatients with severe and persistent mental illness and drug use problems and examined preliminary indicators of outcome. METHODS: A motivational intervention was evaluated with 22 outpatients. The intervention consisted of four individual sessions that were guided by the therapeutic principles of motivational interviewing. All participants met DSM-IV criteria for substance abuse or dependence within the previous six months and were not engaged in treatment for substance abuse. Substance use, treatment involvement, and attitudes toward substance use and cessation were assessed before and after the intervention and at a three-month follow-up session. RESULTS: The feasibility of the motivational intervention was demonstrated. The median time to completion of the intervention was 28 days. It was possible to retain psychiatric outpatients in the intervention, and the patients had favorable perceptions of the intervention. Readiness to change and involvement in treatment increased between preintervention and postintervention assessments. However, many of the postintervention gains had not been maintained at three-month follow-up. CONCLUSIONS: Use of brief motivational interventions can enhance patients' readiness to change substance use to better prepare them for drug treatment programs. Future interventions might benefit from the integration of the intervention with ongoing treatment to ensure that motivational gains are maintained.
Substance use disorders are prevalent among persons who have severe and persistent mental illness (1,2). Although many persons with dual diagnoses participate in psychiatric treatment, many do not recognize their substance use as problematic. Evidence suggests that the vast majority of persons who have substance use disorders are not in the action stage of change (3). Most outpatients with dual diagnoses exhibit low levels of readiness to change their substance abuse (4,5). Data indicating poor treatment attendance (6,7,8) and compliance (9,10) among persons with dual diagnoses suggest that greater attention should be paid to problem recognition and treatment engagement (11). Thus there is a need to develop therapies to increase motivation to reduce or cease substance use.
Individual differences in readiness to change have important implications for treatment. Most therapies for the treatment of substance use disorders focus on active treatment and the prevention of relapse (12,13). However, according to the transtheoretical model, intervention strategies should be tailored to the various stages of change (14). For example, training to develop drug refusal skills may be well received by persons who are ready for active change, but cognitive and motivational strategies—such as consciousness raising—may be more appropriate for persons who are only contemplating change. The effectiveness of treatment can be increased through strategies to motivate patients to make active efforts to change.
Outcome data on the efficacy of interventions to improve motivation among patients with dual diagnoses are lacking. However, several interventions have incorporated motivational principles. In two separate studies, a single motivational interview before inpatient discharge resulted in significant increases in attendance at the first outpatient appointment (15,16). The interviews were based on the principles of motivational interviewing (17) and included discussions of previous treatment experiences and potential barriers to compliance with outpatient treatment. Other programs have incorporated motivational principles within multidimensional treatments (18,19). However, the feasibility of a motivational intervention as an adjunct to outpatient treatment has not been assessed, and the effects of such interventions on problem recognition have not been evaluated.
The purpose of this study was to develop and evaluate a brief motivational intervention for persons with dual diagnoses who are not participating in drug abuse treatment—that is, those who are in the precontemplation, contemplation, or preparation stages of change. The intervention was designed specifically to engage the patient in a discussion of substance use, enhance recognition of a substance use problem, increase involvement in substance abuse treatment, and supplement ongoing outpatient mental health treatment. This stage I therapy development study aimed to evaluate the feasibility and acceptability of the intervention, as determined by attendance patterns and patient satisfaction, and to report preliminary indicators of outcome.
Methods
Participants and procedures
Patients from two hospitals were recruited through referrals from hospital staff. The recruitment criteria were a diagnosis of either a schizophrenia spectrum disorder or bipolar disorder, a current substance use disorder or lifetime substance abuse or dependence as well as problematic substance use during the previous six months, and lack of active engagement in treatment for a substance use disorder. Patients who were judged to be too disorganized or symptomatic to engage in meaningful dialogue were not recruited. A research assistant approached patients at a regularly scheduled appointment, described the project, and invited them to participate. All procedures were reviewed and approved by the institutional review boards of the two hospitals and Syracuse University.
Eligibility was determined on the basis of an interview conducted by a doctoral-level psychologist. The Mini Mental State Examination (MMSE) (20) was used to screen for gross cognitive dysfunction. Possible scores on the MMSE range from 0 to 30, with higher scores indicating better functioning. Patients with scores below 24 were excluded, except for one person for whom a lower score was due to a documented learning disability that affects spelling. The Structured Clinical Interview for DSM-IV (SCID) (21) was used to confirm the diagnoses of patients who were eligible to participate. Of the 31 eligible patients identified, 30 agreed to participate. Data collection took place between March 1999 and July 2000.
Several descriptive measures were also used during the screening session: the Global Assessment of Functioning (GAF) (22), the Positive and Negative Symptom Scale (PANSS) (23), the Alcohol Use Disorders Identification Test (AUDIT) (24), and the short (ten-item) version of the Drug Abuse Screening Test (DAST-10) (25). Possible scores on the GAF range from 1 to 100, with higher scores indicating better functioning. Possible scores on the PANSS range from 30 to 210, with higher scores indicating more severe pathology. Possible scores on the AUDIT range from 0 to 40, with higher scores indicating more harmful or hazardous alcohol consumption. Possible scores on the DAST-10 range from 1 to 10, with higher scores indicating greater risk of drug abuse. All of these instruments have demonstrated strong psychometric properties in previous research with this population (26,27). Patients were paid $10 to participate in this screening session.
Substance use, treatment involvement, and attitudes toward substance use and cessation were assessed before and after the intervention and at three-month follow-up. A research assistant administered all the instruments orally to maximize the quality of the data (28). During all assessments, patients' breath was analyzed with an AlcoSensor IV (Intoximeters, Inc., St. Louis, Missouri) to maximize the accuracy of reporting. The assessment was rescheduled if the patient's blood alcohol level was above .02. The participant's primary problem substance was the reference point for all attitudinal measures, because readiness to change may vary by substance. Nicotine and caffeine were not considered primary substances, because of their pervasive use in this population (29). Participants were paid $10 for each of the pre- and postintervention assessments and $15 at the follow-up session.
Preintervention assessment. The contemplation ladder (30) was used as a representation of participants' readiness to change; higher rungs on the ladder represent greater readiness to change. Four expectancy scales were used to assess participants' perceived importance of quitting substance use and of cutting down and their confidence that they could quit or cut down if they decided to (31).
A stage-of-change algorithm was used to assign patients to one of six stages: precontemplation, during which the person has current substance dependence or abuse and expresses no intention to quit or cut down within six months; contemplation, during which the person intends to change within six months but not within the next month; preparation 1, during which the person intends to change within the month; preparation 2, during which a person in preparation 1 also reports an attempt to quit or cut down in the previous month; action, during which the person says that he or she has quit or cut down within the past six months; and maintenance, during which the person reports change that has been sustained for at least six months. Separate stages were assigned for quitting and cutting down, with the expectation that the latter may be more sensitive to differences among persons with low readiness to change.
Participants then completed a series of self-report scales that measure motivation to change. All the scales have demonstrated reliability and validity with this population (28). The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) (32) assesses the participant's recognition of a substance use problem and whether he or she is taking steps to resolve the problem. The Decisional Balance Scale (DBS) (unpublished data, King TK, DiClemente CC, 1993) assesses perceived pros and cons of continued substance use. The Alcohol and Drug Consequences Questionnaire (ADCQ) (33) measures perceived costs and benefits of quitting or cutting down.
Participation in available treatments was also assessed. We adapted the Treatment Services Review (TSR) (34) to evaluate, for each participant, the number of professional contacts, services provided, and significant discussions that occurred in seven areas: psychiatric problems, alcohol problems, drug problems, medical problems, legal problems, employment problems, and family or social problems. We used a two-week time frame and excluded participation in the research-related intervention sessions from calculations of contacts related to drug or alcohol use.
Substance use was assessed with a 90-day Timeline Followback (TLFB) (35). Alcohol use was recorded in standard drink units for each of the previous 90 days. Drug use was documented by type of drug. Thus we obtained frequency data for a wide range of substances. Temporal reliability and convergent evidence for the validity of TLFB data are strong (36,37).
Three clinician rating scales were completed by primary therapists before the intervention and at the follow-up session, with reference to use of the primary problem substance over the previous 90 days. The Stages of Substance Abuse Treatment Scale (SATS) (38) is used to categorize a patient's involvement in substance abuse treatment as preengagement, engagement, early persuasion, late persuasion, early active treatment, late active treatment, relapse prevention, or full recovery. The SATS is reliable across raters and over time (38). Primary therapists also completed the Alcohol Use Scale (AUS) and the Drug Use Scale (DUS) (39) to indicate the level of a patient's alcohol or drug use over the previous three months on a 5-point scale. The AUS and the DUS are reliable (39) and valid (40).
Intervention. The four individual sessions were conducted according to a detailed treatment manual (4). The intervention was designed to increase recognition of a problem and dissatisfaction with using drugs, interest in quitting, and confidence in the ability to change. Sessions were structured with specific activities and work sheets to help focus participants' attention and record their ideas for later reference. We maintained flexibility in session goals and adjusted the pace when necessary. Catch-up sessions were added when lapses in treatment occurred.
The development of the intervention was guided by three treatment approaches or philosophies. First, the intervention incorporated the five therapeutic principles of motivational interventions (20): expressing empathy, developing discrepancy, avoiding arguments, "rolling with the resistance," and supporting self-efficacy. Central to the motivational approach is a respect for and support of goals that are important to the patient. These principles promote a client-centered yet directive interventional style that can improve recognition of a problem and motivation to change (41).
Second, consistent with a harm-reduction philosophy (42), reductions in substance use that fell short of abstinence were accepted by the therapist. Reduced use is a more proximal goal and may appear more attainable to some patients, especially those who are less ready to change. Third, the transtheoretical model of change (3) was influential in that more action-oriented procedures—for example, developing an action plan—were emphasized only among participants who were judged to be farther along in the change process, whereas consciousness-raising techniques were emphasized among participants who did not recognize their substance use as problematic.
All sessions were conducted by a clinical psychologist with training in motivational interventions (the fourth author). The first session included feedback on substance use patterns identified by the TLFB, comparison with national patterns, and discussion of the consequences and associated risks. The second session involved a decisional balance activity. Reasons for and against change—for example, "good things about using" and "not-so-good things about using"—were elicited from the patient and discussed. Participants were encouraged to elaborate on change-promoting factors. Change-inhibiting factors presented opportunities for problem solving.
In the third session, one to three personal goals—for example, "to live in a better place"—were discussed in light of the potential impact that cutting down or quitting—as opposed to continuing current use patterns—would have on achieving the goals. In session 3 or 4, expectancies about the importance of and confidence in changing were revisited, which provided an opportunity to reinforce improvements and to address reasons for lack of improvement. In the fourth session, realistic substance-related goals were identified and an action plan was developed that included specific steps, how others may help, and ways to address specific barriers that might arise. The therapist also highlighted themes that emerged during the intervention and reinforced change-oriented talk. All participants continued to receive usual medications and supportive counseling but were paid $5 for expenses associated with attending each 30- to 60-minute session.
Postintervention assessment. Treatment acceptability ratings were obtained about a week after the last intervention session. For these ratings, seven adjectives were used to describe the intervention—for example, "valuable" or "worthless"—and seven adjectives were used to describe the therapist—for example, "caring" or "uncaring"—on a 7-point Likert scale. Scores for each item were averaged to form summary scores. At that time, all self-report measures that had been administered before the intervention were readministered. The average weekly use from pre- to postintervention assessments was calculated on the basis of participants' TLFB data.
Follow-up assessment. All the preintervention measures were readministered at the three-month follow-up session. Average weekly use between postintervention and follow-up assessments was determined from TLFB data. In addition, a measure of retention of ideas introduced in the intervention was administered. Participants indicated whether each of 20 topics had been discussed in the intervention—for example, "We discussed reasons I might want to quit or cut down." Foils were included to minimize demand characteristics—for example, "We discussed each of the 12 steps."
Analysis
Analyses were conducted to gather empirical evidence relevant to treatment feasibility and acceptability and within-subject change. First, descriptive statistics were calculated for three sets of variables: consent rates and attrition; client satisfaction variables, including comfort with the intervention and the therapist; and recall of the content of the intervention. Taken together, these data can provide support for the feasibility and acceptability of a newly developed intervention.
Second, we calculated means and effect sizes reflecting change over time on continuous measures of motivation, treatment utilization, and substance use. Effect sizes can be used to estimate the sample size needed to achieve sufficient statistical power in future investigations. Change on categorical measures was evaluated with Wilcoxon signed-rank tests. Evidence of change was derived from both self-report and clinician ratings.
Results
The 30 participants were predominantly male (25 patients, or 83 percent) and either white (16 patients, or 53 percent) or African American (12 patients, or 40 percent). Their mean± SD age was 39±7.2 years, and their mean number of years of education was 12±2.3. Primary psychiatric diagnoses were schizophrenia or schizoaffective disorder (22 patients, or 73 percent), psychotic disorder not otherwise specified (six patients, or 20 percent), and bipolar disorder (two patients, or 7 percent). The primary problem substances were alcohol (20 patients, or 67 percent), cannabis (five patients, or 17 percent), and cocaine (five patients, or 17 percent). Continuous psychiatric and substance use variables for the study sample are listed in Table 1. Mean AUDIT and DAST-10 scores exceeded the recommended cutoff points for identifying substance use disorders among psychiatric outpatients (26).
Of the 30 patients who consented to participate, six did not begin the intervention—two missed at least three scheduled appointments, two lost contact, one had worsening symptoms, and one had transportation problems. One patient withdrew from the intervention after two sessions, and one was hospitalized after the third session. Thus 22 patients completed the intervention and the postintervention assessment, reflecting a completion rate of 73 percent of eligible participants and 92 percent of those who began the intervention. These 22 patients were not significantly different from the eight patients who did not complete the assessment on any demographic, psychiatric, or substance use variables. Follow-up data were obtained for 19 of these 22 patients. Two participants could not be found, and another participant was too disorganized to provide reliable data.
The median time to complete four intervention sessions was 28 days. Participants missed a median of two appointments during the course of attending the seven scheduled meetings. The patients had favorable perceptions of the therapeutic experience; median ratings across the seven dimensions that we assessed ranged from 5 to 6.5. Perceptions of the therapist were also positive, with a median rating of 6.1. At the three-month follow-up session, 18 participants completed the measure of therapy idea retention. However, three of these said they recalled content that was not in fact covered in the therapy sessions and endorsed all items that were actually covered by the intervention, so their responses on this measure may not have been reliable. The remaining 15 participants recalled 69 percent of the topics that were actually included in the intervention.
Although this study was designed as a stage I therapy development study, some indicators of outcome can be reported. At baseline, the sample exhibited low levels of readiness to change; in terms of quitting substance use, most (73 percent) were in the precontemplation stage of change. In terms of cutting down, four participants were in the precontemplation stage, three were in the contemplation stage, two were preparing to change in the next month, five had made an effort to change during the previous month, one was in the action stage, and one was in the maintenance stage. The results of the Wilcoxon signed-rank test indicated that at the postintervention assessment, participants had not moved forward in terms of cutting down. However, in terms of quitting substance use, participants tended to be in more advanced stages of change.
Mean±SD values of continuous variables at the three assessment times are presented in Table 2, along with effect sizes. The table lists effect sizes rather than inferential statistics as a means of presenting the magnitude of change observed, a practice consistent with the recommendations of leading data analysts (43,44). Effect sizes can be interpreted as follows: .2 is small, .5 is medium, and .8 is large (45). From pre- to postintervention assessments, taking steps to resolve problematic substance use increased the most (effect size, .63), followed by confidence in cutting down (.46), reflecting medium-sized effects. The items with the next largest effect sizes were confidence in quitting (effect size, .37), readiness to change as represented on the contemplation ladder (.31), alcohol or drug-related treatment involvement (.30), perceived cons of substance use (.29), and recognition of problematic use (.28), reflecting small to medium-sized effects. The reductions in substance use observed between preintervention and postintervention assessments all reflect small effects.
Table 3 shows the pattern of change in a subset of variables that represent primary intervention goals, illustrating the pattern and variability of responses to the intervention. After the intervention, a majority of the participants (17 patients, or 77 percent) used their primary problem substance less frequently, used more treatment services, or had greater recognition of their problem.
As can be seen in Table 2, only a few of the postintervention gains were maintained over the three-month follow-up period. Scores for the contemplation ladder, confidence in quitting, recognition, and taking steps to resolve problematic substance use all decreased relative to the postintervention scores, although these motivational indexes remained elevated relative to preintervention levels. Participation in alcohol and drug treatment remained elevated at follow-up, but most gains in substance use variables were not maintained.
Clinicians' reports were consistent with the changes reported by the patients. Before the intervention, both the mode and the median of the SATS ratings reflected the early persuasion stage, indicating that most participants were not actively involved in substance-related treatment. However, by the follow-up session, eight participants received higher ratings of treatment involvement, whereas only two received lower ratings (p<.04). These independent clinicians' ratings support the idea that participation in the intervention helped to increase the treatment engagement of many of the participants in this study.
Clinicians' ratings on the AUS and the DUS also indicated that patients reduced their use of substances between preintervention and the follow-up session; the median rating decreased from 3 (indicating abuse) at preintervention to 2 (indicating nonproblematic use) at follow-up. More participants received lower ratings than received higher ratings for severity of substance use (eight participants and two participants, respectively; p=.05).
Discussion and conclusions
The results of this study support the feasibility and acceptability of a four-session motivational intervention for use with persons who have serious and persistent mental illness and a substance use disorder. The study provided preliminary evidence that the intervention had the intended effects on attitudes and behaviors. Patients became engaged in discussion about their substance use, improved their recognition of their substance use problems, and demonstrated greater involvement in substance-related treatment.
The feasibility of this intervention was demonstrated in several ways. First, only one patient discontinued the intervention voluntarily, and the 22 patients who completed the intervention rated the intervention and the therapist positively. Thus although these participants were identified as not being actively engaged in treatment for their substance use problems, they became engaged in the brief motivational intervention. Only six patients did not attend any sessions. An attrition rate of 20 percent is encouraging given that patients with dual diagnoses often find it difficult to follow through on structured commitments.
Our results compare favorably with the rate of 33 percent (19 of 58 consenters) who failed to begin a substance abuse treatment program in a study of persons with serious mental illness (18). In that study 62 percent of the outpatients who started the six-month intervention also completed it. Thus our ability to conduct a three-month follow-up session with 79 percent of the patients who started the intervention appears to be consistent with the results of others who have worked with this treatment-resistant population.
As with any study that uses a small sample, we observed substantial variability in participants' responses to the intervention. In addition, most gains dissipated after patients finished the intervention. In the absence of more intensive, action-oriented treatment options for patients dual diagnoses, the patients in our study could not maintain changes. This finding is not surprising; most providers recognize that treatment for patients with dual diagnoses should be ongoing and multidimensional (19,46,47). Future efforts might enhance the integration of a motivational intervention with ongoing treatment to facilitate maintenance or might supplement the initial intervention with booster sessions to maintain motivational gains.
Our findings suggest that moving to the next stage of therapy development is warranted. To enhance confidence in these findings, treatment effects should be demonstrated with a comparison group in a study using a randomized design and a larger sample. It may be productive to use this intervention as an initial component of therapy (15,16,48) that leads to more extensive treatment for persons with dual diagnoses, one that addresses skills training (18) and environmental supports and incentives for abstinence.
Acknowledgments
This work was supported by grants R01-DA-10010 and K02-DA-00426 to Kate Carey from the National Institute on Drug Abuse. The authors thank Adrienne Williams.
The authors are affiliated with the Center for Health and Behavior at Syracuse University. Send correspondence to Kate B. Carey, Ph.D., 430 Huntington Hall, Center for Health and Behavior, Syracuse University, Syracuse, New York 13244-2340 (e-mail, [email protected]).
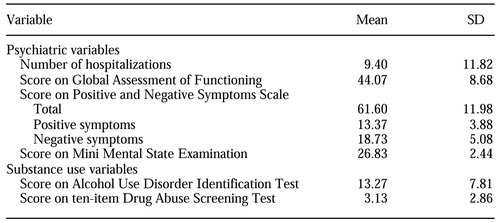 |
Table 1. Psychiatric and substance use variables among 30 psychiatric outpatients who participated in a study of readiness to change substance use
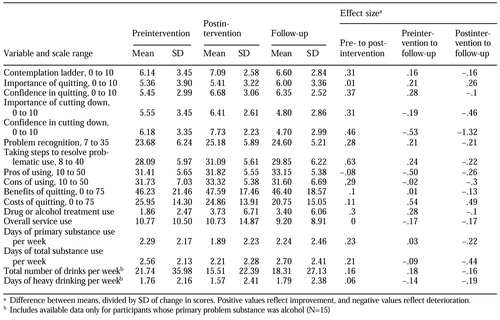 |
Table 2. Therapeutic outcomes among 30 psychiatric outpatients at preintervention, postintervention, and three-month follow-up
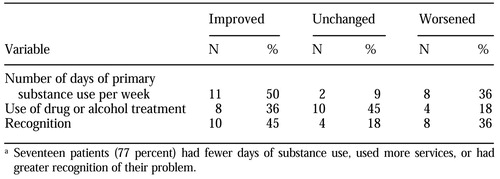 |
Table 3. Changes in key substance use variables between preintervention and postintervention for 22 patients with severe and persistent mental illness and drug use problemsa
a Seventeen patients (77 percent) had fewer days of substance use, used more services, or had greater recognition of their problem
1. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
2. Blanchard JJ, Brown SA, Horan WP, et al: Substance use disorders in schizophrenia: review, integration, and a proposed model. Clinical Psychology Review 20:207-234, 2000Crossref, Medline, Google Scholar
3. Prochaska JO, DiClemente CC, Norcross JC: In search of how people change: applications to addictive behaviors. American Psychologist 47:1102-1114, 1992Crossref, Medline, Google Scholar
4. Carey KB, Purnine DM, Maisto SA, et al: Enhancing readiness-to-change substance abuse in persons with schizophrenia: a four-session motivation-based intervention. Behavior Modification 25:331-384, 2001Crossref, Medline, Google Scholar
5. Ziedonis DM, Trudeau K: Motivation to quit using substances among individuals with schizophrenia: implications for a motivation-based treatment model. Schizophrenia Bulletin 23:229-238, 1997Crossref, Medline, Google Scholar
6. Lehman AF, Herron JD, Schwartz RP, et al: Rehabilitation for adults with severe mental illness and substance use disorders. Journal of Nervous and Mental Disease 181:86-90, 1993Crossref, Medline, Google Scholar
7. Richardson MA, Craig TJ, Haugland G: Treatment patterns of young chronic schizophrenic patients in the era of deinstitutionalization. Psychiatric Quarterly 57:104-110, 1985Crossref, Medline, Google Scholar
8. Teesson M, Gallagher J: Evaluation of a treatment programme for serious mental illness and substance use in an inner city area. Journal of Mental Health 8(1):19-28, 1999Google Scholar
9. Owen RR, Fischer EP, Booth BM, et al: Medication noncompliance and substance abuse among patients with schizophrenia. Psychiatric Services 47:853-858, 1996Link, Google Scholar
10. Pristach CA, Smith CM: Medication compliance and substance abuse among schizophrenic patients. Hospital and Community Psychiatry 41:1345-1348, 1990Abstract, Google Scholar
11. Osher FC, Kofoed LL: Treatment of patients with psychiatric and psychoactive substance abuse disorders. Hospital and Community Psychiatry 40:1025-1030, 1989Abstract, Google Scholar
12. Hester RK, Miller WR: Handbook of Alcoholism Treatment Approaches: Effective Alternatives. New York, Pergamon, 1989Google Scholar
13. Onken LS, Blaine JD, Boren JJ: Behavioral treatments for drug abuse and dependence, in NIDA Research Monograph 137. Washington, DC, National Institute on Drug Abuse, 1993Google Scholar
14. DiClemente CC: Changing addictive behaviors: a process perspective. Current Directions in Psychological Science 2:101-106, 1993Crossref, Google Scholar
15. Daley DC, Zuckoff A: Improving compliance with the initial outpatient session among discharged inpatient dual diagnosis clients. Social Work 43:470-473, 1998Crossref, Medline, Google Scholar
16. Swanson AJ, Pantalon MV, Cohen KR: Motivational interviewing and treatment adherence among psychiatric and dually diagnosed patients. Journal of Nervous and Mental Disease 187:630-635, 1999Crossref, Medline, Google Scholar
17. Miller WR, Rollnick S: Motivational interviewing: preparing people to change addictive behavior. New York, Guilford, 1991Google Scholar
18. Bellack AS, Gearon JS: Substance abuse treatment for people with schizophrenia. Addictive Behaviors 23:749-766, 1998Crossref, Medline, Google Scholar
19. Ziedonis DM, Fisher W: Motivation-based assessment and treatment of substance abuse in patients with schizophrenia. Directions in Psychiatry 16:1-7, 1996Google Scholar
20. Folstein MF, Folstein SE, McHugh PR: "Mini-Mental State": a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189-198, 1975Crossref, Medline, Google Scholar
21. First MG, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV—Patient Version (SCID-I/P, Version 2.0). New York, New York State Psychiatric Institute, biometric department, 1995Google Scholar
22. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
23. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin 13:261-276, 1987Crossref, Medline, Google Scholar
24. Bohn MJ, Babor TF, Kranzler HR: The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol 56:423-432, 1995Crossref, Medline, Google Scholar
25. Skinner H: The Drug Abuse Screening Test. Addictive Behaviors 7:363-371, 1982Crossref, Medline, Google Scholar
26. Maisto SA, Carey MP, Carey KB, et al: Use of the AUDIT and DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychological Assessment 12:186-192, 2000Crossref, Medline, Google Scholar
27. Purnine DM, Carey KB, Maisto SA, et al: Assessing positive and negative symptoms in outpatients with schizophrenia and mood disorders. Journal of Nervous and Mental Disease 188:653-661, 2000Crossref, Medline, Google Scholar
28. Carey KB, Maisto SA, Carey MP, et al: Readiness to change substance misuse among psychiatric outpatients: I. reliability and validity of self-report measures. Journal of Studies on Alcohol 62:79-88, 2001Crossref, Medline, Google Scholar
29. Carey KB, Maisto SA, Carey MP, et al: Use of legal drugs by psychiatric outpatients: benefits, costs, and change. Cognitive and Behavioral Practice 6:15-22, 1999Crossref, Medline, Google Scholar
30. Biener L, Abrams DB: The contemplation ladder: validation of a measure of readiness to consider smoking cessation. Health Psychology 10:360-365, 1991Crossref, Medline, Google Scholar
31. Sobell MB, Sobell LC: Problem drinkers: guided self-change treatment. New York, Guilford, 1993Google Scholar
32. Miller WR, Tonigan JS: Assessing drinkers' motivation for change: the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychology of Addictive Behaviors 10:81-89, 1996Crossref, Google Scholar
33. Cunningham JA, Sobell LC, Gavin DR, et al: Assessing motivation for change: preliminary development and evaluation of a scale measuring the costs and benefits of changing alcohol or drug use. Psychology of Addictive Behaviors 11:107-114, 1997Crossref, Google Scholar
34. McLellan AT, Alterman AI, Woody GE, et al: A quantitative measure of substance abuse treatments: the Treatment Services Review. Journal of Nervous and Mental Disease 180:101-110, 1992Crossref, Medline, Google Scholar
35. Sobell LC, Sobell MB: Timeline Followback User's Guide: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Addiction Research Foundation, 1996Google Scholar
36. Carey KB: Reliability and validity of the Timeline Follow-Back Interview among psychiatric outpatients: a preliminary report. Psychology of Addictive Behaviors 11:26-33, 1997Crossref, Google Scholar
37. Ehrman RN, Robbins SJ: Reliability and validity of 6-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology 62:843-850, 1994Crossref, Medline, Google Scholar
38. McHugo GJ, Drake RE, Burton HL, et al: A scale for assessing the stage of substance abuse treatment in persons with severe mental illness. Journal of Nervous and Mental Disease 183:762-767, 1995Crossref, Medline, Google Scholar
39. Drake RE, Mueser KT, McHugo GJ: Clinical rating scales: Alcohol Use Scale (AUS), Drug Use Scale (DUS), and Substance Abuse Treatment Scale (SATS), in Outcomes Assessment in Clinical Practice. Edited by Sederer LI, Dickey B. Baltimore, Williams & Wilkins, 1996Google Scholar
40. Carey KB, Cocco KM, Simons JS: Concurrent validity of substance abuse ratings by outpatient clinicians. Psychiatric Services 47:842-847, 1996Link, Google Scholar
41. Enhancing motivation to change, in Treatment Improvement Protocol (TIP) Series. DHHS publication no (SMA) 99-3353. Washington, DC, Center for Substance Abuse Treatment , 1999Google Scholar
42. Marlatt GA: Harm Reduction. New York, Guilford, 1999Google Scholar
43. Cohen J: The earth is round (p<.05). American Psychologist 49:997-1003, 1994Crossref, Google Scholar
44. Wilkinson L: Statistical methods in psychology journals: guidelines and explanations. American Psychologist 54:594-604, 1999Crossref, Google Scholar
45. Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Erlbaum, 1988Google Scholar
46. Carey KB: Substance use reduction in the context of outpatient psychiatric treatment: a collaborative, motivational, harm reduction approach. Community Mental Health Journal 32:291-306, 1996Crossref, Medline, Google Scholar
47. Drake RE, Bartels SJ, Teague GB, et al: Treatment of substance abuse in severely mentally ill patients. Journal of Nervous and Mental Disease 181:606-611, 1993Crossref, Medline, Google Scholar
48. Brown JM, Miller WR: Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors 7:211-218, 1993Crossref, Google Scholar



