Relationship of Treatment Orientation and Continuing Care to Remission Among Substance Abuse Patients
Abstract
OBJECTIVES: The authors examined whether continuing outpatient mental health care, the orientation of the treatment program (12-step, cognitive-behavioral, or eclectic), and involvement in self-help groups were linked to substance abuse patients' remission status two years after discharge. METHODS: The data were from a cohort of 2,805 male patients who were treated through one of 15 Department of Veterans Affairs substance abuse programs. Remission was defined as abstinence from illicit drug use and abstinence from or nonproblem use of alcohol during the previous three months. The relationships of the three variables to remission were tested with regression models that controlled for baseline characteristics. RESULTS: About a quarter of the study participants (28 percent) were in remission two years after discharge. Intake characteristics that predicted remission at two years included less severe substance use and psychiatric problems, lower expected disadvantages and costs of discontinuing substance use, and having abstinence as a treatment goal. No significant relationship emerged between treatment orientation and remission status two years later. Involvement in outpatient mental health care during the first follow-up year and participation in self-help groups during the last three months of that year were associated with a greater likelihood of remission at the two-year follow-up. CONCLUSIONS: The results extend previously published one-year outcome findings showing that cognitive-behavioral and 12-step treatment programs result in similar remission rates. Patients who enter intensive substance abuse treatment with polysubstance use, psychiatric symptoms, or significant emotional distress have more difficulty achieving remission. Routinely engaging patients in continuing outpatient care is likely to yield better outcomes. The duration of such care is probably more important than the number of sessions.
Substance use disorders are notoriously difficult to treat, as evidenced by high relapse rates (1,2). Although there is empirical support for the short-term effectiveness of many treatment modalities (3), sustained remission is difficult to achieve (4). Generalizable information about longer-term remission is scarce, because most trials of treatment efficacy have focused on short-term outcomes after a course of experimentally controlled treatment among "ideal" patients with relatively homogeneous backgrounds. For example, the patients typically have no comorbid psychiatric diagnoses and are treated by staff who are freshly trained in a focused treatment regimen and monitored as they provide treatment. Findings from such studies do not necessarily generalize well to populations of ordinary patients in typical treatment programs.
To learn more about the course of substance use disorders among patients receiving routine treatment and about patient and treatment characteristics that may affect the course of the disorders, we focused on predictors of being in remission two years after an acute episode of intensive treatment for substance abuse. We addressed four questions. First, is the orientation of substance abuse treatment—12-step, cognitive-behavioral, or eclectic (mixed)—associated with remission after two years? Second, does continuing specialized outpatient mental health care or participation in self-help groups during the first year increase the likelihood of being in remission at two years? Third, are the effects of continuing care and involvement in self-help groups independent? And fourth, are such effects similar for patients who have a coexisting psychiatric disorder and those who do not?
Substance abuse treatment programs with 12-step and cognitive-behavioral orientations differ in their underlying principles, intervention techniques, and treatment goals. For example, 12-step programs stress the disease model of addiction, the fellowship of Alcoholics Anonymous, and the necessity of complete abstinence, whereas cognitive-behavioral programs stress change in maladaptive cognitions and development of more effective coping responses.
The relative merits of the two approaches have been debated for many years in terms of both their overall effectiveness and the types of patients for whom they are best suited (5,6). Studies comparing the two methods have been conducted only recently and have not shown consistent differences (7,8,9,10,11,12,13). Although clinical wisdom has long held that matching the type of treatment to patient characteristics will improve outcomes (14), a recent large, rigorous efficacy trial of 12-step facilitation and cognitive-behavioral treatment did not support many hypothesized effects of such matching (8,9,10).
The sample in this study comprised patients with substance use disorders who were treated in 12-step, cognitive-behavioral, and eclectic programs of the Department of Veterans Affairs (VA) under ordinary conditions of care. At a one-year follow-up assessment, there were no significant differences in remission by treatment orientation or by any of several tested interactions between treatment orientation and patient characteristics, including psychiatric comorbidity (12,15,16).
Patients who participate in continuing specialized outpatient mental health treatment after being discharged from intensive treatment for substance abuse tend to have better long-term outcomes in both efficacy studies (17) and effectiveness studies (18,19,20,21,22), including the one-year follow-up of the sample used in this study (23). Continuing care seems to be equally effective regardless of the theoretical orientation of the initial treatment (24).
Several studies have shown that the overall period during which a patient is in specialized outpatient continuing care—or "extensity"—predicts outcome better than does the sheer number of sessions attended—or "intensity" (3,20,23). In this study we examined the relationship of both the extensity and the intensity of continuing care during the first year after intensive treatment to remission status after two years. Furthermore, we investigated whether continuing care is especially important for patients who have comorbid psychiatric symptoms or psychiatric diagnoses.
Involvement in self-help groups after intensive treatment also can be effective in maintaining gains from an initial treatment episode (18,19,21,23,25,26). There is some evidence that 12-step self-help programs are more effective if the initial treatment has a 12-step orientation rather than a cognitive-behavioral one (26,27).
These studies have used outcome measures that were assessed at the same follow-up point at which continuing care or involvement in self-help groups were measured. By contrast, in this study we temporally separated these assessments. We examined whether the orientation of the treatment program, continuing outpatient care, and participation in self-help groups were linked to remission after two years among patients with substance use disorders.
Methods
Participants
All male inpatients in 15 VA substance abuse programs who were sufficiently detoxified were invited to participate in an evaluation of treatment effectiveness. Of the 3,698 patients in the intake sample, 92 died during the first year, and 3,018 (84 percent) completed the one-year follow-up. During the second year, 110 patients died and 2,805 (80 percent) completed the two-year follow-up, of whom 2,529 had provided data at the one-year follow-up. Data were collected between 1992 and 1997. For the group of 2,805, the mean±SD age at intake was 42.8±9.5 years, and the mean number of years of education was 12.7±1.8; 544 patients (19 percent) were currently married, 1,273 patients (45 percent) identified themselves as white, and 1,125 patients (40 percent) had received inpatient substance abuse treatment in the previous two years. Informed consent and institutional review board approval were obtained.
Measures
An intake information form and a follow-up information form were used at entry and follow-up, respectively, to obtain information on demographic characteristics, substance use and related variables, psychiatric symptoms, and psychosocial functioning. Diagnostic and treatment data for the two-year follow-up period were compiled from nationwide VA databases.
Remission. Consistent with the definition used in a previous study (15), remission was defined as abstinence from illicit drug use and either abstinence from or nonproblem use of alcohol. To be categorized as being in remission, a patient had to have abstained from all 13 drugs investigated, to have had no problems related to drug or alcohol abuse, and to have consumed no more than three ounces of alcohol on the day of the highest alcohol consumption in the previous three months. Some patients did not have alcohol use disorders, and, given that alcohol is a legal substance, we allowed for a limited amount of alcohol use, as long as it was not associated with any problems related to substance use. Freedom from problems related to substance use was reflected by a response of "never" to each of 15 problems in the areas of health, work, legal situation, and finances.
Patient characteristics at intake. The covariates listed in Table 1 were chosen because they have been used as covariates in previous studies and because a body of literature suggests that they are predictors of remission in their own right. They include age, number of years of education, marital status, motivation as assessed at intake with items from the determination and action subscales of the Stages of Change Readiness and Treatment Eagerness Scale (28), and whether the patient had received inpatient substance abuse treatment in the previous year, measured as a binary variable. The severity of substance use at intake was assessed by the frequency of alcohol and drug use (total days of use per month during the previous three months) (15,29), the number of substances used, and problems related to substance abuse, as assessed by 15 items about health, work, legal problems, and financial problems (15).
The severity of psychiatric symptoms at intake was assessed with 22 items from the depression, anxiety, paranoid ideation, and psychotic symptom subscales of the Brief Symptom Inventory (BSI) (30). Possible scores on the BSI range from 0 to 88, with higher scores indicating more severe symptoms. In addition, the presence or absence of an ICD-9 psychiatric diagnosis at intake—other than substance abuse or dependence—was determined from the nationwide VA Patient Treatment File, which includes diagnoses provided by VA clinicians. Cognitions related to substance abuse treatment outcomes (31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47) included expectancies about the consequences of continued substance use and of discontinuing substance use, assessed by the Outcomes Expectancies Scale (41); level of religious belief, rated on a scale from 1 to 5, with higher scores indicating higher levels of belief; abstinence as a treatment goal, measured as a dichotomous variable; confidence in being abstinent one year later, rated on a scale of 1 to 10, with higher scores indicating greater confidence; and endorsement of an alcoholic or addict identity, rated on a scale of 1 to 5, with higher scores indicating stronger endorsement.
Index treatment orientation. The 15 treatment programs were judged to have a 12-step, cognitive-behavioral, or eclectic treatment orientation on the basis of interviews with program directors about treatment activities as well as program directors' and staff members' responses to the Drug and Alcohol Program Treatment Inventory (48). There were five programs in each treatment orientation category.
Continuing care. Using the nationwide VA Outpatient Clinic File, we identified all psychiatric or substance abuse outpatient visits by the study participants during the first year. To temper the skewed distribution, we divided the number of visits into quintiles roughly corresponding to no treatment and quarterly, monthly, biweekly, and weekly treatments (zero, one to four, five to12, 13 to 24, and 25 or more visits per year). The overall duration of treatment was indexed by the total number of months (zero to 12) during the first follow-up year in which the patient had at least two outpatient visits. A self-report item from the one-year follow-up information form inquired about the level of attendance at self-help meetings (zero meetings, one to nine meetings, ten to 19 meetings, 20 to 29 meetings, and 30 or more meetings in the previous three months).
Analyses
Using bivariate logistic regression models with a significance threshold of .05, we identified baseline patient characteristics related to both remission status and treatment type as potential covariates. These characteristics are also included in Table 1. All subsequent analyses used an alpha of less than .01 to reduce the likelihood of type I error. The effects of treatment orientation and continuing care on remission were tested with hierarchical logistic regression.
Results
A total of 772 of the 2,805 patients (28 percent) were in remission at the two-year follow-up. Of the 2,521 who provided sufficient data at both time points, 1,547 (61 percent) were not in remission at either follow-up point, 363 (14 percent) were in remission at both points, and the remaining 611 (24 percent) were in remission at one of the two follow-up points. The odds of being in remission at two years were almost six times as high among patients who were already in remission at one year (odds ratio=5.6, 95 percent confidence interval=4.63 to 6.87, p<.001).
After screening patient characteristics to identify relationships with both treatment orientation and two-year remission, we included the following intake variables, listed in Table 1, in the set of covariates: frequency of substance use, number of substances used, problems related to substance abuse, psychiatric diagnosis, expected costs of discontinuing substance use, abstinence as a treatment goal, and confidence in being abstinent one year later. For the sake of consistency, covariates used in previous work (16) were also included—age, education, marital status, motivation, and inpatient substance abuse treatment during the previous two years. Psychiatric symptoms and positive expectancies of substance use at intake were predictive of not being in remission at the two-year follow-up but were independent of treatment type (Table 1).
After adjustment for the 12 covariates, 12-step treatment orientation was not significantly predictive of remission status compared with cognitive-behavioral or an eclectic treatment orientation. Similarly, no significant difference in remission rates was observed between patients who received cognitive-behavioral treatment and those who attended 12-step programs.
Next, we focused on whether continuing outpatient mental health care during the first follow-up year predicted remission at the second-year follow-up when the effects of covariates and index treatment orientation were controlled for (Table 2). The number of months during which a patient had at least two outpatient mental health visits in the first year significantly predicted remission status at two years (OR=1.07 per month, p<.01). Cross-tabulating the number of months of treatment (zero to 12) by remission status, we found that more than half of the patients who had received 12 months of outpatient treatment were in remission (48 of 91 patients, or 53 percent), compared with about a quarter (21 to 29 percent) who had received no more than four months of treatment, and about a third (27 to 41 percent) who had received five to 11 months of treatment (χ2=49.1, df=12, p<.001).
Patients who had received more sessions of outpatient care during the first follow-up year also had a better odds of remission (OR=1.15 per frequency category, controlling for covariates and treatment type). About a third of patients who had had at least 25 sessions were in remission at the end of the second year, compared with 26 percent of those who had had fewer sessions (OR=1.73, p<.01, with covariates and treatment type controlled for).
Attendance at self-help meetings during the last three months of the first year was also related to remission status at the end of the second year (OR=1.22 per ten self-help visits, 95 percent CI=1.15 to 1.29, p<.01), with covariates and treatment type controlled for. About 42 percent of the patients who had attended more than 30 meetings achieved remission, compared with about a quarter of those who had attended fewer meetings.
In an omnibus model that included all three continuing care variables, covariates, and treatment type, the duration of outpatient care (OR=1.11 per month, 99 percent CI=1.03 to 1.18, p<.001) and self-help attendance (OR=1.25 per ten meetings, CI= 1.16 to 1.36, p<.001) remained significant predictors of remission, but the actual number of outpatient treatment sessions was not a significant predictor.
To sharpen the comparison, we limited our interaction analyses to patients who participated in cognitive-behavioral or 12-step programs. Contrary to our prediction, the interactions between treatment orientation and both psychiatric symptoms and diagnosis were not significant when covariates were controlled for. Also contrary to prediction, continuing care was about equally helpful for patients at all levels of baseline severity, whether continuing care was operationalized as duration, number of sessions, or attendance at self-help meetings and whether severity was operationalized as psychiatric symptoms, psychiatric diagnosis, inpatient treatment in the previous year, or problems related to substance abuse. Similarly, attendance at self-help meetings had about the same relationship to remission whether the index treatment had a 12-step or a cognitive-behavioral orientation.
Discussion
Twenty-eight percent of the participants in this study were in remission at the two-year follow-up, compared with 25 percent at the one-year follow-up. Of those who were in remission at one year, 57 percent were also in remission at two years; of those who were not in remission at one year, 19 percent were in remission at two years.
It is difficult to compare remission rates across studies, because many studies have focused on abstinence rather than remission, and the follow-up period and the required duration of remission of symptoms vary widely among studies. However, it is clear from these and previous findings that substance abuse is a chronic relapsing condition and that many patients, even some of those who are receiving continuing care, do not achieve stable remission during the first two years after intensive treatment. Only about 50 percent of the patients in this study who had received a full 12 months of outpatient care during the first posttreatment year were in remission at the end of the second year. Similarly, only about 40 percent of patients with the highest level of participation in self-help groups during the last three months of the first year were in remission at the two-year follow-up.
Consistent with the one-year data (15) and with the results of Project MATCH (8,9,10), there was no significant effect of treatment orientation on second-year remission status after covariates were controlled for. The results were similar for patients who had comorbid psychiatric symptoms or disorders and those who did not. At the one-year follow-up, patients who had participated in 12-step treatment had a slight advantage in terms of abstinence, but no effect of treatment orientation on remission was noted (15). It is unlikely that these results are attributable to differences between sites, because the sites were carefully selected for equivalence on other dimensions, such as treatment intensity (15).
Continuing care, operationalized in terms of both additional outpatient mental health visits and self-help sessions during the first year, was predictive of remission at two years. This finding is consistent with the results of previous analyses of one-year outcomes among patients receiving outpatient care (18,23) or participating in self-help programs (18,26). Alternative explanations for this relationship, such as the possibility that the most compliant or resilient patients were more likely both to attend sessions and to achieve remission, await further exploration. However, we did control for motivation at intake.
The overall duration of additional outpatient care was more predictive of remission than the total number of sessions. This finding suggests that having somewhat less frequent contacts over a longer period could improve outcomes without requiring more staff time. Further research into the nature of this duration-response relationship is needed to determine whether there is an optimal period of care and whether outcomes improve as care increases or only up to a threshold. For this chronic, relapsing disorder, remission tends to be unstable, so the availability of sustained—but not necessarily intensive—therapeutic support is important at each stage of achieving, maintaining, and reestablishing remission.
Overall, patients who had more severe difficulties at intake were less likely to be in remission two years after treatment, particularly if they used multiple substances or had psychiatric problems. Our finding of a greater likelihood of nonremission at two years among patients with comorbid psychiatric conditions contrasts with the one-year findings (16), which showed similar substance abuse outcomes for patients who did and those who did not have psychiatric diagnoses. The longer follow-up period in this study may have provided additional time for the negative effects of psychiatric disorders to unfold.
Patients with dual diagnoses were less likely to achieve remission than patients who received the same level of care but who had only a substance use disorder, even though continuing care was associated with similar increases in their likelihood of remission. It remains an open question whether longer duration, greater intensity, more precisely targeted continuing care, or all of these would improve remission outcomes in this vulnerable patient group.
Although 12-step-oriented treatment is designed partly to facilitate the effectiveness of self-help groups and was found to do so at the one-year follow-up in our cohort (26), we found that self-help attendance was no less predictive of remission among patients who had participated in cognitive-behavioral programs than among patients who had received 12-step-oriented treatment. The previous analyses (26) differed from this one in that they indexed self-help involvement rather than attendance, assessed self-help contemporaneously with outcomes, and did not include remission as an outcome.
Future studies might investigate other treatment outcomes, such as reduced symptoms and improved functioning. The remission variable that we used provides a rough categorization of long-term outcomes. As VA patients, the participants in this study had a particular range of demographic characteristics. Studies of women and of community-based samples are needed to determine the degree to which the pattern of findings from this study is generalizable to other populations. Nevertheless, the sample is a strength of this study in that it was more heterogeneous than the samples used in most treatment trials and is broadly representative of the population of persons served by the large nationwide treatment system we studied.
Conclusions
Participation in cognitive-behavioral, 12-step, or eclectic treatment did not differentially predict remission status two years after discharge from intensive treatment for substance abuse. Patients who entered substance abuse treatment with polysubstance use or a comorbid psychiatric condition had more difficulty achieving long-term remission. Our findings suggest that patients in treatment programs that routinely engage patients in continuing outpatient care are likely to have better outcomes and that the overall duration of care is more important than the number of sessions. Involvement in self-help groups after intensive treatment also can improve outcomes.
However, even with continuing care and attendance at self-help meetings, most patients do not achieve lasting remission after a single course of treatment. Our findings highlight the intractable nature of many persons' substance use disorders and the importance of the provision of ongoing care by substance abuse treatment systems as needed.
Acknowledgments
This work was supported by the Department of Veterans Affairs Mental Health Strategic Healthcare Group and Health Services Research and Development Service and by grant AA-12718 from the National Institute on Alcohol Abuse and Alcoholism.
The authors are affiliated with the Program Evaluation and Resource Center and the Center for Health Care Evaluation of the Veterans Affairs Palo Alto Health Care System and Stanford University School of Medicine in California. Send correspondence to Dr. Ritsher at the Program Evaluation and Resource Center (MPD 152), VA Palo Alto Health Care System, 795 Willow Road, Menlo Park, California 94025 (e-mail, [email protected]).
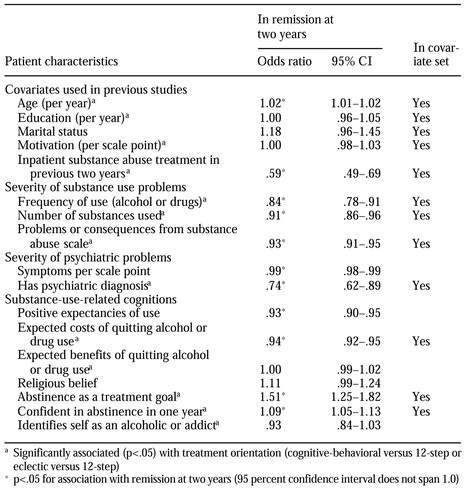 |
Table 1. Results of unadjusted bivariate logistic regression of patient characteristics at intake, remission status at two years, and treatment orientation
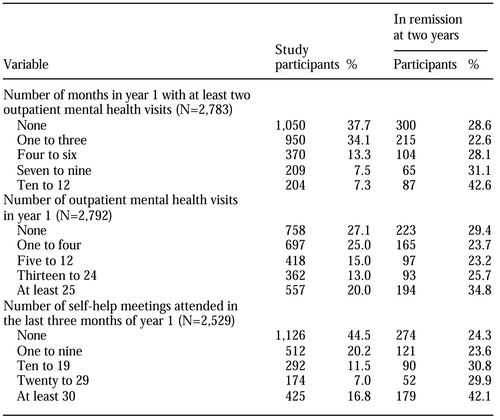 |
Table 2. Remission at two years by involvement in continuing outpatient care and self-help groups
1. Hunt WA, General WR: Relapse rates after treatment for alcoholism. Journal of Community Psychology 1:66-68, 1973Crossref, Google Scholar
2. O'Brian CP, McLellan AT: Myths about the treatment of addiction. Lancet 347:237-240, 1996Crossref, Medline, Google Scholar
3. Finney JW, Moos RH: Psychosocial treatments for alcohol use disorders, in A Guide to Treatments That Work. Edited by Nathan PE, Gorman JM. New York, Oxford University Press, 1998Google Scholar
4. Finney JW, Moos RH, Timko C: The course of treated and untreated substance use disorders: remission and resolution, relapse and mortality, in Addictions: A Comprehensive Guidebook. Edited by McCrady BS, Epstein E. New York, Oxford University Press, 1999Google Scholar
5. Bruns JA, Hanna FJ: Abstinence versus controlled use: a fresh perspective on a stale debate. Journal of Addictions and Offender Counseling 16:14-29, 1995Crossref, Google Scholar
6. Gerstein DR: The effectiveness of drug treatment, in Addictive States. Edited by O'Brian CP, Jaffe JH. New York, Raven, 1992Google Scholar
7. Brennan PI: Cognitive behavioral program vs twelve-step program: comparative effectiveness of two outpatient drug/alcohol treatment models. Dissertation Abstracts International, 96-B, 3049. University Microfilms International order no AAM-9835462, 1998Google Scholar
8. Project MATCH Research Group: Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol 58:7-29, 1997Crossref, Medline, Google Scholar
9. Project MATCH Research Group: Project MATCH secondary a priori hypotheses. Addiction 92:1671-1698, 1997Crossref, Medline, Google Scholar
10. Project MATCH Research Group: Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research 22:1300-1311, 1998Crossref, Medline, Google Scholar
11. Wells EA, Peterson PL, Gainey RR, et al: Outpatient treatment for cocaine abuse: a controlled comparison of relapse prevention and twelve-step approaches. American Journal of Drug and Alcohol Abuse 20:1-17, 1994Crossref, Medline, Google Scholar
12. Ouimette PC, Finney JW, Gima K, et al: A comparative evaluation of substance abuse treatment: III. examining mechanisms underlying patient-treatment matching hypotheses for 12-step and cognitive-behavioral treatments for substance abuse. Alcoholism: Clinical and Experimental Research 23:537-544, 1999Medline, Google Scholar
13. Maude-Griffin PM, Hohenstein JM, Humfleet GL, et al: Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. Journal of Consulting and Clinical Psychology 66:832-837, 1998Crossref, Medline, Google Scholar
14. Miller WS: The effectiveness of treatment for substance abuse: reasons for optimism. Journal of Substance Abuse Treatment 9:93-102, 1992Crossref, Medline, Google Scholar
15. Ouimette PC, Finney JW, Moos RH: Twelve-step and cognitive-behavioral treatment for substance abuse: a comparison of treatment effectiveness. Journal of Consulting and Clinical Psychology 65:230-240, 1997Crossref, Medline, Google Scholar
16. Ouimette PC, Gima K, Moos RH, et al: A comparative evaluation of substance abuse treatment: IV. the effect of comorbid psychiatric diagnoses on amount of treatment, continuing care, and 1-year outcomes. Alcoholism: Clinical and Experimental Research 23:552-557, 1999Crossref, Medline, Google Scholar
17. Patterson DG, Macpherson J, Brady NM: Community psychiatric nurse aftercare for alcoholics: a five year follow-up study. Addiction 92:459-468, 1997Crossref, Medline, Google Scholar
18. Miller NS, Ninonuevo FG, Klamen DL, et al: Integration of treatment and posttreatment variables in predicting results of abstinence-based outpatient treatment after one year. Journal of Psychoactive Drugs 29:239-248,1997Crossref, Medline, Google Scholar
19. Miller NS, Hoffmann NG: Addictions treatment outcomes. Alcoholism Treatment Quarterly 12:41-55, 1995Crossref, Google Scholar
20. Moos RH, Finney JW, Federman EB, et al: Specialty mental health care improves patients' outcomes: findings from a nationwide program to monitor the quality of care for patients with substance use disorders. Journal of Studies on Alcohol 61:704-713, 2000Crossref, Medline, Google Scholar
21. Moos R, Schaefer J, Andrassy J, et al: Outpatient mental health care, self-help groups, and patients' 1-year treatment outcomes. Journal of Clinical Psychology 57:273-287, 2001Crossref, Medline, Google Scholar
22. Swindle RW, Phibbs CS, Paradise MJ, et al: Inpatient treatment for substance abuse patients with psychiatric disorders: a national study of determinants of readmission. Journal of Substance Abuse 7:79-97, 1995Medline, Google Scholar
23. Ouimette PC, Moos RH, Finney JW: Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. Journal of Studies on Alcohol 59:513-522, 1998Crossref, Medline, Google Scholar
24. Donovan DM: Continuing care: promoting the maintenance of change, in Treating Addictive Behaviors, 2nd ed. Edited by Miller WR, Heather N. New York, Plenum, 1998Google Scholar
25. McKay JR, Merikle E, Mulvaney FD, et al: Factors accounting for cocaine use two years following initiation of continuing care. Addiction 96:213-225, 2001Crossref, Medline, Google Scholar
26. Humphreys K, Huebsch PD, Finney JW, et al: A comparative evaluation of substance abuse treatment: V. substance abuse treatment can enhance the effectiveness of self-help groups. Alcoholism: Clinical and Experimental Research 23:558-563, 1999Crossref, Medline, Google Scholar
27. Humphreys K: Professional interventions that facilitate 12-step self-help group involvement. Alcohol Research and Health 23:93-98, 1999Google Scholar
28. Miller WR, Tonigan JS: Assessing drinkers' motivation for change: the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES), in Addictive Behaviors: Readings on Etiology, Prevention, and Treatment. Edited by Marlatt GA, VandenBos GR. Washington, DC, American Psychological Association, 1997Google Scholar
29. Hubbard RL, Mardsen ME, Rachal JV, et al: Drug abuse treatment: a national study of effectiveness. Chapel Hill, University of North Carolina Press, 1989Google Scholar
30. Derogatis L: Brief Symptom Inventory: Administration, Scoring, and Procedures Manual, 3rd ed. Minneapolis, National Computer Systems, 1993Google Scholar
31. Brown SA: Reinforcement expectancies and alcoholism treatment outcome after a one-year follow-up. Journal of Studies on Alcohol 46:304-308, 1985Crossref, Medline, Google Scholar
32. Hittner JB: Alcohol-related outcome expectancies: construct overview and implications for primary and secondary prevention. Journal of Primary Prevention 17:297-314, 1997Crossref, Google Scholar
33. Jones BT, McMahon J: Negative alcohol expectancy predicts post-treatment abstinence survivorship: the whether, when, and why of relapse to a first drink. Addiction 89:1653-1655, 1994Crossref, Medline, Google Scholar
34. Jones BT, McMahon J: Negative and positive alcohol expectancies as predictors of abstinence after discharge from a residential treatment program: a one-month and three-month follow-up study in men. Journal of Studies on Alcohol 55:543-548, 1994Crossref, Medline, Google Scholar
35. Jones BT, McMahon J: Changes in alcohol expectancies during treatment relate to subsequent abstinence survivorship. British Journal of Clinical Psychology 35:221-234, 1996Crossref, Medline, Google Scholar
36. Lee NK, Oei TP, Greeley JD: The interaction of alcohol expectancies and drinking refusal self-efficacy in high and low risk drinkers. Addiction Research 7:91-102, 1999Crossref, Google Scholar
37. Leigh BC, Stacy AW: Alcohol outcome expectancies: scale construction and predictive utility in higher order confirmatory models. Psychological Assessment 5:216-229, 1993Crossref, Google Scholar
38. Sher KJ, Wood MD, Wood PK, et al: Alcohol outcome expectancies and alcohol use: a latent variable cross-lagged panel study. Journal of Abnormal Psychology 105:561-574, 1996Crossref, Medline, Google Scholar
39. Pare LC: The role of self-efficacy in the recovery process among multiple substance abusers in aftercare. Dissertation Abstracts International 60, 12-B, 6378. University Microfilms order no AAINQ-43578, 2000Google Scholar
40. Finney JW, Moos RH, Humphreys K: A comparative evaluation of substance abuse treatment: II. linking proximal outcomes of 12-step and cognitive-behavioral treatment to substance use outcomes. Alcoholism: Clinical and Experimental Research 23:537-544, 1999Medline, Google Scholar
41. Solomon KE, Annis HM: Development of a scale to measure outcome expectancy in alcoholics. Cognitive Therapy Research 13:409-421, 1989Crossref, Google Scholar
42. Sheehan T, Owen P: The disease model, in Addictions: A Comprehensive Guidebook. Edited by McCrady BS, Epstein EE. New York, Oxford University Press, 1999Google Scholar
43. Corwyn RF, Benda BB: Religiosity and church attendance: the effects on use of "hard drugs" controlling for sociodemographic and theoretical factors. International Journal for the Psychology of Religion 10:241-258, 2000Crossref, Google Scholar
44. Glasgow RE, Morray K, Lichtenstein E: Controlled smoking versus abstinence as a treatment goal: the hopes and fears may be unfounded. Behavior Therapy 20:77-91, 1989Crossref, Google Scholar
45. Gottheil E: Advantages and disadvantages of the abstinence goal in alcoholism. American Journal of Drug and Alcohol Abuse 3:13-23, 1976Crossref, Medline, Google Scholar
46. McKay JR, Alterman AI, Cacciola JS, et al: Continuing care for cocaine dependence: comprehensive two-year outcomes. Journal of Consulting and Clinical Psychology 67:420-427, 1999Crossref, Medline, Google Scholar
47. Sanchez-Craig M, Lei H: Disadvantages to imposing the goal of abstinence on problem drinkers: an empirical study. British Journal of Addiction 81:505-512, 1986Crossref, Medline, Google Scholar
48. Moos RH, Finney JW, Ouimette PC, et al: A comparative evaluation of substance abuse treatment: I. treatment orientation, amount of care, and 1-year outcomes. Alcoholism: Clinical and Experimental Research 23:529-536, 1999Medline, Google Scholar



