Outcomes of Decreased Length of Hospital Stay Among Geriatric Patients With Dementia
Abstract
This study examined the outcomes associated with shortening hospital stays for geriatric inpatients with dementia at a Veterans Administration medical center. Thirty-three patients who were admitted after January 1997, when the hospital decided to reduce patients' lengths of stay, were matched with 33 patients who were admitted before January 1997. Despite significant differences in lengths of stay, no differences were found between the groups on measures of agitation or overall functioning. Despite significantly shorter stays since January 1997, the results of our study indicate that the cognitive and emotional status of patients discharged since that time are equivalent to those of patients discharged after longer hospital stays.
Over the past several years, hospitals, insurance companies, and agencies responsible for allocating funds for medical care have mandated increasingly shorter hospital stays for psychiatric patients (1). Whereas formerly these patients were hospitalized for weeks or years, most acutely ill psychiatric patients are now treated with brief inpatient stays or on an outpatient basis (2,3). Some studies suggest that brief inpatient treatment or outpatient treatment is as effective or more effective than long-term inpatient programs for patients with severe mental illness (4). Other findings indicate that patients with depression who are discharged after a shorter stay are more depressed and are more globally impaired on discharge (2). One study found that psychiatric hospitals are increasingly treating a poorer, sicker group of patients with shorter hospital stays, resulting in poorer long-term outcomes and more readmissions (5).
In January 1997 the Houston Veterans Affairs (VA) Medical Center, through a utilization review process, shortened psychiatric lengths of stay. Physicians are now required to report to the chief of service all patients with a length of stay beyond 20 days rather than beyond 30 days, as previously required. In the retrospective case-control study reported here, we examined the outcomes of agitation, cognitive functioning, and readmissions among geriatric patients with dementia after lengths of stay were administratively decreased. We hypothesized that these patients would be negatively affected by the shortened hospital stay because of problems in providing comprehensive biopsychosocial assessment and treatment in a brief period.
Methods
We examined data for all patients who had a primary diagnosis of dementia without delirium and were admitted between October 1993 and November 1997 to the medical center's geropsychiatric inpatient unit for treatment of behavioral disturbance—physical aggression, verbal threats, wandering, or general confusion. The patients received a comprehensive multidisciplinary evaluation by a geriatric psychiatrist, a geropsychologist, psychiatric nurses, a social worker, and a physician's assistant. Each patient's treatment and attending staff remained relatively consistent throughout the course of this study.
On admission and discharge, the attending psychiatrist rated each patient on a standardized battery consisting of the Mini Mental State Examination (MMSE) (6) and the Cohen-Mansfield Agitation Inventory (CMAI) (7), which includes subscales of aggressive, nonaggressive, and verbal agitation. Interrater reliability was evaluated every 12 to 18 months, and intraclass correlation coefficients were never less than .76 for the CMAI and .9 for the MMSE.
Axis I psychiatric diagnoses by DSM-III-R criteria, and later DSM-IV criteria, were established within two weeks of discharge at a consensus conference attended by two geriatric psychiatrists, and a geropsychologist. All patients received multidisciplinary treatment, including pharmacotherapy, a structured milieu, and family education.
Of the 276 patients with dementia consecutively admitted between October 1993 and November 1997, 243 were diagnosed as having dementia without delirium. Thirty-three of these patients were first admitted after January 1997, when the decision was made to reduce length of stay. In order to obtain groups of patients with equivalent baseline psychiatric status, the 33 patients admitted after January 1997 were matched with 33 of the 210 patients admitted before January 1997. Patients were matched on CMAI and MMSE scores at admission and on age. CMAI scores were considered to be equivalent within a range of plus or minus 5 points. MMSE scores were considered to be equivalent within a range of plus or minus 1 point. Age was allowed to vary within a range of plus or minus ten years. In the case of more than one appropriate match, the matching person was randomly selected.
We analyzed the data with SPSS for Windows (1995). We used paired t tests to compare the mean scores between the matched groups and to compare the differences between admission and discharge scores for all 66 patients. We compared Global Assessment of Functioning (GAF) scores at discharge as well as living arrangements—long-term care versus home care—number of readmissions per patient per year, and average length of stay during readmission.
Results
The final sample of 66 patients included 65 men and one woman. The mean±SD age was 73.6±5.75 years (range=62 to 88 years), and the mean±SD MMSE score at admission was 15.22±8.86. (Scores on the MMSE range from 0 to 30, with higher scores indicating higher cognitive function.) Forty-five participants were Caucasian (68 percent), 20 were African American (30 percent), and one was Hispanic (2 percent).
Paired t tests revealed a significant difference in length of stay between patients admitted before January 1997 (mean±SD=32±14.4 days) and those admitted after January 1997 (mean±SD=23±10.7 days) (t=2.48, df=31, p=.02). However, no significant differences were found between the groups in scores at discharge for the CMAI (total score or subscale scores), the MMSE, or the GAF or in GAF change scores. In addition, no significant differences were found in the percentage change in scores between admission and discharge on any of these measures. Living arrangements at discharge also did not differ. No significant differences were found between the groups in the number of psychiatric or medical readmissions or in the average length of stay during readmission.
Paired t tests indicated that all 66 patients in the sample had significantly better CMAI scores and GAF scores at discharge than at admission (Table 1); however, no significant differences were found in MMSE scores.
Discussion and conclusions
The results of this study suggest that significantly shortened lengths of stay may not affect patients' cognitive status, agitation levels, or level of care at discharge. Decreased lengths of stay were accomplished through weekly administrative review of patients whose stays were extended. Several explanations could account for the similar levels of improvement after lengths of stay were decreased. First, patients were so severely ill on admission to the geropsychiatry unit that there was necessarily regression to the mean. Second, during this period of shortened lengths of stay, geropsychiatry outpatient services were enhanced—for example, a geropsychologist was added to the outpatient treatment team. Third, the advantage of using well-validated assessment instruments—a strength of this study—may have been offset by the small sample size.
The reduced lengths of stay in this study were still relatively high by community standards. As lengths of stay continue to decline, outcome studies that go beyond the limitations of large administrative databases will be important. Such studies should examine not only specific behavior and health service use outcomes but also ratings of caregiver burden and staff provider satisfaction.
Dr. Kunik and Dr. Orengo are associated with the department of psychiatry and behavioral sciences at Baylor College of Medicine, One Baylor Plaza, Houston, Texas 77030 (e-mail, [email protected]. edu). Ms. Edwards is a medical student at Baylor College of Medicine. Dr. Kunik is also associated with the Veterans Affairs Medical Center and the Veterans Integrated Service Network in Houston. Dr. Molinari is associated with the Veterans Affairs Medical Center, and Ms. Hale is with the University of Houston.
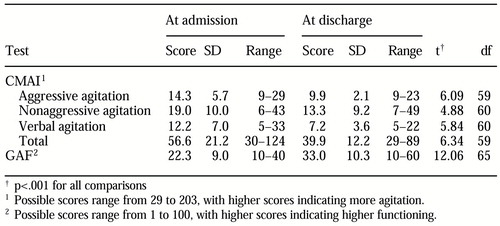 |
Table 1. Comparison of Cohen-Mansfield Agitation Inventory (CMAI) and Global Assessment of Functioning (GAF) scores between admission and discharge for 66 geriatric patients with dementia who were treated at a Veterans Affairs medical center
1. Priest RG, Fineberg N, Merson S, et al: Length of stay of acute psychiatric inpatients: an exponential model. Acta Psychiatrica Scandinavica 92:315-317, 1995Crossref, Medline, Google Scholar
2. Lieberman PB, Wiitala SA, Elliott B, et al: Decreasing length of stay: are there effects on outcomes of psychiatric hospitalization? American Journal of Psychiatry 155:905-909, 1998Google Scholar
3. Glick ID, Hargreaves WA, Drues J, et al: Short vs long hospitalization: a prospective controlled study: VII. two-year results for nonschizophrenics. Archives of General Psychiatry 34:314-317, 1977Crossref, Medline, Google Scholar
4. Creed F, Black D, Anthony P, et al: Randomised controlled trial of day patient versus inpatient psychiatric treatment. British Medical Journal 300:1033-1037, 1990Crossref, Medline, Google Scholar
5. Druss BG, Bruce ML, Jacobs SC, et al: Trends over a decade for a general hospital psychiatry unit. Administration and Policy in Mental Health 25:427-435, 1998Crossref, Medline, Google Scholar
6. Folstein MF, Folstein SE, McHugh PR: "Mini-mental state": a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189-198, 1975Crossref, Medline, Google Scholar
7. Cohen-Mansfield J, Marx MS, Rosenthal AS: A description of agitation in a nursing home. Journal of Gerontology 44:M77-M84, 1989Google Scholar



