A Review of the Literature on the Epidemiology of Parasuicide in the General Population
Abstract
OBJECTIVE: The author reviewed recent literature on the epidemiology of parasuicide in the general population. Major risk factors are also discussed. METHODS: Parasuicide was defined as suicide attempts and deliberate self-harm inflicted with no intent to die. Articles in English on rates of parasuicide in the general population from 1970 through June 2000 were identified by keyword searches of the PsycINFO and MEDLINE databases. Studies that provided data from a representative population sample and provided incidence or prevalence rates were included in the review. Articles focusing on subsamples such as adolescents or psychiatric patients were excluded. Results and conclusions: Twenty studies were analyzed. Although methodological problems constitute a major limitation in interpretation of the results, the literature indicates that parasuicide is a serious public health problem. Reported annual rates of parasuicide in recent decades range from 2.6 to 1,100 per 100,000, and lifetime prevalence rates range from 720 to 5,930 per 100,000. The most important risk factors identified were younger age and female gender. Others included being single or divorced, being unemployed, having a recent change in living situation, having a mental disorder, and having a previous parasuicide incident.
In the past two decades, suicidal behavior has gained recognition as a serious problem worldwide. Suicide is the eighth leading cause of death in the United States (1), and in developed regions worldwide it ranks ninth among causes of death (2). The greatest predictor of eventual suicide is parasuicide, which, defined broadly (3), includes both suicide attempts and deliberate self-harm inflicted with no intent to die. A review by Gunnell and Frankel (4) indicated that 30 to 47 percent of suicide completers had a prior history of parasuicide. Other researchers report similar results (5,6,7,8,9).
Little epidemiological information about parasuicidal individuals is available. National data on parasuicide are not collected in the United States or in Europe (10), but estimates suggest that the rate of attempted suicide may be about ten times the suicide rate (11,12). Although national costs of parasuicide have yet to be calculated, several studies indicate that the toll in terms of psychiatric services is significant (13,14,15). A review of the literature seems timely to consolidate available information and to direct future efforts in this area. This review evaluates research published during the past two decades on the rate of parasuicide in the general population. Methodological problems and risk factors are also discussed.
Methods
Studies of the epidemiology of parasuicide in the general population from 1970 through June 2000 were identified in searches of the PsycINFO and MEDLINE databases using keywords such as attempted suicide, parasuicide, self-mutilation, self-harm, and self-injury along with epidemiology, rates, prevalence, and incidence. Studies in English that provided data based on a representative population sample and calculated incidence or prevalence rates were included in the review. Articles focusing exclusively on self-poisoning or any other specific method of parasuicide were excluded, as were studies on subsamples such as adolescents or psychiatric patients.
Twenty studies were examined. Articles on major risk factors for parasuicide were reviewed as well, but they were not subject to the above criteria. Methodological details are listed in Table 1, and parasuicide rates from studies based on medical records and population surveys are listed in Tables 2 and 3, respectively. Because of methodological inconsistencies across studies, a meta-analysis was not attempted.
Results
Methodological problems
Attempted suicide and deliberate self-harm that is not suicidal in nature are very different behaviors. In research literature on suicidal behavior, however, the two are often blurred together. Self-injurious behavior is often labeled a suicide attempt, and thus people who never intended to kill themselves are included in samples of "suicide attempters" (16,17,18,19). If intent is considered, it is often inferred on the basis of circumstances of the parasuicide (3) in a variety of different ways across studies. This uncertainty is especially problematic in light of evidence demonstrating the importance of stated intent (20,21). Intent is difficult to evaluate and has therefore been left out of major research on parasuicide (22), although some promising results suggest that it can be reliably assessed (23).
The term parasuicide was coined in an attempt to bring clarity to this situation (24). It was intended to serve as a broader term describing all nonfatal self-injurious behavior with clear intent to cause bodily harm or death, thereby reserving "attempted suicide" for situations in which intent is known. The term is commonly used in Europe and increasingly in the United States, but because it has been inconsistently interpreted (25), caution is necessary when making comparisons across studies.
Another problem is the widely differing methodologies between studies. For example, some studies on attempted suicide are based on one question, whereas others are more detailed (26,27,28,29). Most commonly, studies are based on hospital admissions for suicide attempts, though how "suicide attempt" is defined and assessed may vary widely (30). Outcome variables and assessment procedures are not standardized (31). Age-group and gender-specific rates, which are vital in accurately assessing the topography of parasuicide, often are not calculated. Furthermore, although some studies measure parasuicide with event rates—that is, the total number of parasuicide events in a given time frame—others use person rates, in which a person is counted only once, even if he or she had multiple parasuicide incidents within the time period.
The literature on risk factors for parasuicide is equally problematic. Typically risk factors are identified by noting demographic characteristics that appear frequently among parasuicidal individuals. However, because most studies lack control groups, the meaning of such findings is uncertain. We may know, for example, that a high proportion of people who attempt suicide are depressed. If the same proportion in the general population were depressed and did not attempt suicide, however, depression would not be a risk factor (32).
Finally, the sources of information for studies on parasuicide are inadequate. In the absence of national data, information comes from two types of studies: registration studies, which are based on medical records (Table 2), and population surveys (Table 3). Registration studies may miss a substantial number of people who never seek treatment (33,34). Population surveys typically collect lifetime prevalence rates, making them difficult to compare with the annual incidence rates reported in registration studies, and they are usually based on only one question about suicidal behavior. Other sources remain largely untapped—for example, inpatient facilities, psychiatric and veterans hospitals, extended care facilities, police, prison records, insurance records, and private physicians.
Rates of parasuicide
Registration studies. The first large-scale project attempted was the World Health Organization (WHO) Multicentre Study on Parasuicide (25), which drew data from 16 different sites over time. Schmidtke and associates (35) analyzed WHO data collected from 1989 to 1992. The results are interesting in several ways. First, rates of parasuicide varied substantially across sites, by as much as a factor of seven. This variability might support the hypothesis that parasuicide rates vary by location. However, the amounts of missing data and the process of data collection also varied among the sites, which could have influenced rates (22,35).
Another notable finding is the consistently higher rates of parasuicide for females (see Table 2). Rates for men were higher than those for women at only one site, providing strong evidence for the common assumption that parasuicide is more common among women. Age was also consistently important, with higher rates found among younger people. At seven centers, females 15 to 24 years old had the highest rates. Among males, the highest rates were among 25- to 34-year-olds at ten of the centers. The lowest rates for both males and females were among those 55 years of age and older (35).
Parasuicide rates in the WHO study seemed to decrease over time. For males, the average decrease was 17 percent over the four years analyzed. Although this figure reflects a large effect by the center of Guipuzcoa, where rates decreased by 69 percent, the rates decreased by more than 5 percent at 11 centers. For females, the overall decrease was 14 percent. Analyses evaluating fade-out—the gradual slackening of monitoring over time—suggest that the decreases in rates over time were not due to monitoring fatigue. Trends were not uniform across centers over the four years, and continuous decreases were found at only one site. All other sites also had years in which rates increased. Intersite reliability measures were not calculated.
Although the WHO study constitutes a major contribution to the literature on parasuicide, it has some serious limitations. The study used a single definition of parasuicide, but it did not incorporate any measure of intent. Moreover, reports based on the WHO data use "parasuicide" and "attempted suicide" as essentially equivalent terms; throughout the report by Schmidtke and associates (35), the terms are used interchangeably. This is cause for some concern. It calls into question the inclusion criteria used at the various WHO sites. Was "self-harm" actually operationalized into "suicide attempt," and if so, how? It may be that the WHO researchers opted for the term "suicide attempt" in keeping with regional preference; in some areas, including the United States, the term "suicide attempt" tends to be taken more seriously than "parasuicide." Whatever the reason, the result is problematic. As with previous research, we cannot be sure of exactly what behavior is being studied.
Another limitation of the WHO study is its focus on medically treated parasuicide. Although this approach may have been necessary methodologically, it creates problems from an epidemiological standpoint. The potential influence of parasuicide that is not medically treated is strikingly illustrated at two sites that provided estimates—Bordeaux and Umea. If parasuicide rates are calculated from medically treated cases exclusively, Bordeaux's rate would be 42 percent higher than Umea's. If all cases were included, Umea's rate would be 125 percent higher (35). If these estimates are accurate, they provide strong evidence of the need to widen the scope of assessment.
Other registration studies of the epidemiology of parasuicide have tended to mirror the results of the WHO study. Rates have varied widely by location, ranging from a low of 2.6 per 100,000 to a high of 542 per 100,000 (see Table 2). Given methodological differences, it is unclear whether these figures reflect true differences in parasuicide rates with geographic location or whether the differences are attributable to differences in methodology.
The lowest rates were found in cities in Africa and Asia. Rates for females were almost universally higher than rates for males (29,35,36,37,38,39,40,41). Most studies also show the highest rates among women in their teens to early twenties (30,35,36,40,42) and men in their twenties (20,35,36,37,42) (see Table 2).
Gunnell and colleagues (30) made a unique contribution by collecting additional information about admission procedures to explain this effect. They found that 9 percent of the variance in admission rates for parasuicide was explained by socioeconomic status, with lower socioeconomic status correlated with higher rates; with an outlier excluded, the figure leaped to 68 percent. They also found significant variation in admission procedures between the hospitals in their sample. These two factors, then, may explain some of the variation in parasuicide rates across studies.
Population surveys. In population surveys, usually one question on suicide— "Have you ever attempted suicide?"—is incorporated into larger population surveys not focused on parasuicide. The lifetime prevalence rates typically reported are difficult to compare with rates from registration studies. However, the few surveys that have obtained annual rates have shown rates similar to or higher than those of registration studies, ranging from 300 to 1,100 per 100,000 (see Table 3). Lifetime prevalence rates range from 750 to 5,930 per 100,000. As in the registration studies, women typically had higher rates than men (19,27,29,70,71,73,74). Age distributions were more mixed.
The National Comorbidity Study (19) improved on other population surveys by measuring intent. Although an estimated 4.6 percent of the population had made a suicide attempt, 47.3 percent of attempters did not intend to die; hence the percentage of actual attempts should be somewhat lower. This finding also indicates that the single question usually employed in this type of study is insufficient to identify true suicide attempts, and it provides dramatic evidence of the need to measure intent.
In another survey, Briere and Gil (43) made one of the first attempts to measure nonsuicidal deliberate self-harm. Estimates of the prevalence of self-mutilation are speculative, ranging from 14 to 750 per 100,000 each year and 750 per 100,000 (44,45). Briere and Gil found that 4 percent of a representative sample of the general population (4,000 per 100,000) reported engaging in at least occasional instances of self-mutilation over the previous six months, and .3 percent reported often engaging in such behavior. The study's methodology is limited, however. Subjects were simply asked about self-harm without the intent to die. How they interpreted this phrase is anyone's guess, and most likely the findings were inflated.
Risk factors for parasuicide
Marital status. The prevailing idea that being single or divorced is a risk factor for parasuicide appears to have strong empirical support. In the WHO report, for instance, single people had the highest average rate of parasuicide over the entire study period. Although this result was at least partly due to the high proportion of young people in the sample, the relative risk for single and divorced persons was still higher than for the general population when age was controlled for (35). Similar findings have been reported elsewhere (19,20,36,40,42,48,49,72,74).
It has been hypothesized that single or divorced persons have higher rates of parasuicide because they live alone, but other research indicates that the phenomenon may not be so simple. Some studies indicate that many single or divorced persons may actually be cohabiting with a partner of some sort. In a study in Oxford, England, for example, Hawton and colleagues (50) found that single and divorced persons were heavily represented among parasuicidal subjects. However, the majority did not live alone. Sixty-seven percent of single subjects and 52 percent of divorced subjects reported living with a partner. In fact, only 22 percent of the study subjects lived alone at the time of their parasuicide incident. To Hawton and colleagues, these findings suggested that the central risk factor may have to do with interpersonal conflict, especially in relation to a partner. This idea would be consonant with evidence in several previous studies (31,49,51).
Clearly, the relationship between marital status and parasuicide is complex. Future research will be needed to clarify the underlying mechanisms of risk, whether they are the interpersonal friction of divorce, interpersonal problems within a household, loneliness or lack of social support among single persons, interaction between factors, or other factors. It also remains unclear, in the absence of longitudinal data, whether parasuicide is a cause or a consequence of being single or divorced.
Living situation. The WHO study showed that a change in living situation occurred before a parasuicide in 10 percent of male subjects and 6 percent of female subjects. The most frequent pattern was a change from some socially stable situation to living alone, living in an unstable situation, or living in an institution (35). Hjelmeland (20) found that having changed address within the previous 12 months was a risk factor for parasuicide.
The presence of children in the household may serve as a protective factor against parasuicide. In the WHO study, a relatively high proportion of parasuicidal females who normally lived with a partner and children (24 percent, compared with 2.2 percent of males) had changed to living with only a partner (35). Appleby and Turnbull (52) found that parasuicide among postpartum women is much lower than among other women, despite the high rates of postpartum depression. This finding is consistent with other research suggesting that reasons people have for living, such as children, may be predictive of whether or not they will attempt to kill themselves (53).
Unemployment. Unemployment has long been thought to increase the risk of parasuicide and was confirmed by Platt (54), who found in his 1984 review that the overrepresentation of the unemployed across studies was overwhelming. His conclusion is strongly supported in recent studies as well (20,40,72,74). The proportion of unemployed persons is significantly higher among parasuicidal individuals than among the general population, and parasuicide rates among unemployed persons are consistently higher than rates among employed people. Furthermore, the risk of parasuicide is positively correlated with duration of unemployment.
Understanding precisely why unemployment is so important, however, has proved difficult. Even with a longitudinal design spanning 19 years, Platt and Kreitman (55) were unable to find any simple explanation for the relationship of unemployment to parasuicide rates. Several explanations have been proposed, but it remains unclear to what degree other, co-occurring risk factors contribute to the trends. For instance, in a report on a two-year cohort of males in Edinburgh (56), unemployed parasuicidal men also tended to have other risk factors that are linked to both parasuicide and unemployment. Other research has suggested that ethnic or cultural factors (57) or characteristics such as hopelessness (58) may mediate the relationship.
Mental disorders. There is some evidence that having a mental disorder is a risk factor for parasuicide. The most frequent diagnoses are mood disorders, and especially depression (19,39,41,49,5960,61). Panic and anxiety disorders have also been associated with parasuicide (62,74), as have schizophrenia, psychotic disorders, personality disorders, and adjustment disorders (39,41,59). Comorbidity is common (19,59,63).
Alcohol or substance abuse is commonly associated with parasuicide (20,28,40,59,64,65,73,74). Alcohol use immediately before the parasuicide may be even more common. In a Helsinki sample, 81 percent of men and 66 percent of women had consumed alcohol before their parasuicide (11). Other studies report rates of 24 percent (65); 41 percent for males and 31 percent for females (67); and 24.8 percent (38). In one prospective study, alcohol abuse was one of a few significant predictors of a future parasuicide (20).
Socioeconomic status. Low socioeconomic status has been examined as a risk factor for parasuicide. It is sometimes assessed in terms of its correlates—for instance, low educational status or living in a low-income area. Still, researchers almost universally find correlations between these variables and parasuicide (35,36,49,57,61,67).
Previous attempts. Previous parasuicide is highly predictive of future parasuicide (68). Research generally involves either retrospective reports by parasuicidal patients or hospital readmission rates. In the WHO study, 42 percent of males and 45 percent of females had a previous parasuicide (35). Other studies have reported similar findings, with repetition rates ranging from 20 percent to more than 50 percent (27,36,40,67,69). Not much longitudinal research has been done with follow-up of individuals after an incident of parasuicide, which is the next step in accurately assessing parasuicide repetition rates.
Conclusions
Clearly, parasuicide is a complex behavior that is difficult to study effectively. Despite mounting efforts, we are still left with a fairly rough epidemiological picture, largely because of methodological inconsistencies across studies. Nevertheless, rates of parasuicide seem quite high. Findings range from 2.6 to 542 per 100,000 in registration studies, which are mostly based on samples of medically treated individuals. One-year incidence rates from population surveys, which include more than just those who were medically treated, range from 700 to 1,100 per 100,000, and lifetime prevalence rates range from 720 to 5,930 per 100,000. It is unclear whether rates truly vary by location, or whether different methodologies account for the differences.
Despite methodological problems, most studies identify similar risk factors. Women appear to have higher rates of parasuicide than men. Younger age groups of both males and females are at higher risk, with females somewhat younger than males in many studies. Marital status, being unemployed, having a recent change in living situation, having a mental disorder, and having a previous parasuicide incident are risk factors. How these factors interact is unclear, and we have yet to identify precisely the reasons for these risk factors.
Studies are needed that analyze broader samples than just medically treated subjects. Definitions must be tightened and standardized, and more longitudinal studies could provide valuable information. Naturally, such projects would require considerable resources. Studying parasuicide is difficult. It involves tremendous sensitivity and cost, and parasuicidal individuals are difficult to assess, both in the hospital and in the community. However, the potential costs of letting this problem go on without focused attention are surely far greater.
Acknowledgments
The author thanks Marsha Linehan, Ph.D., for her guidance and suggestions and Kate Comtois, Ph.D., Ann VanderStoep, Ph.D., and Shawn Welch for their helpful comments.
Ms. Welch is a doctoral student in the department of psychology, University of Washington, Seattle, Washington 98195 (e-mail, [email protected]). She is also affiliated with the department's behavioral research and therapy clinics.
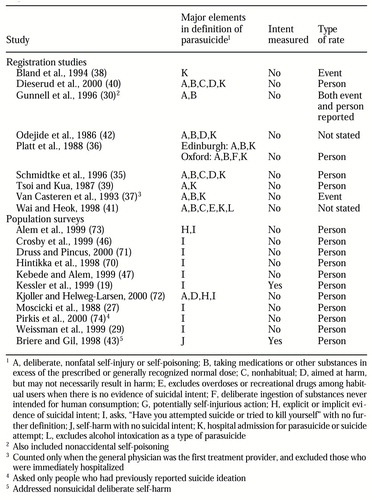 |
Table 1. Definitions and type of rate reported registration studies and population surveys of parasuicide
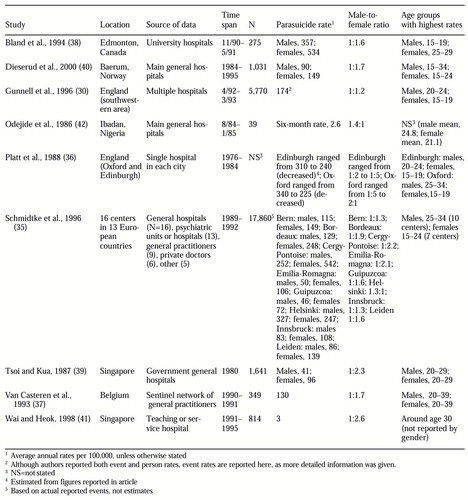 |
Table 2. Studies of parasuicide based on data from medical records (registration studies)
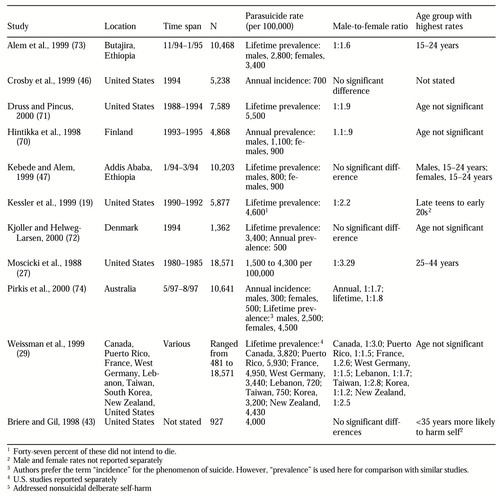 |
Table 3. Studies of parasuicide based on data from population surveys
1. US Public Health Service: The Surgeon General's Call to Action to Prevent Suicide. Washington, DC, 1999Google Scholar
2. Murray CJL, Lopez AD (eds): Summary: The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Global Burden of Disease and Injury Series, vol 1. Harvard School of Public Health, on behalf of World Health Organization and World Bank. Cambridge, Mass, Harvard University Press, 1996Google Scholar
3. Linehan MM: Behavioral treatments of suicidal behaviors: definitional obfuscation and treatment outcomes, in The Neurobiology of Suicide: From the Bench to the Clinic. Edited by Stoff DM, Mann JJ. Annals of the New York Academy of Sciences 836:302-328, 1997Crossref, Medline, Google Scholar
4. Gunnell D, Frankel S: Prevention of suicide: aspirations and evidence. British Medical Journal 308:1227-1233, 1994Crossref, Medline, Google Scholar
5. Ovenstone IM, Kreitman N: Two syndromes of suicide. British Journal of Psychiatry 124:336-345, 1974Crossref, Medline, Google Scholar
6. Foster T, Gillespie K, McClelland R: Mental disorders and suicide in Northern Ireland. British Journal of Psychiatry 170:447-452, 1997Crossref, Medline, Google Scholar
7. Nordentoft M, Breum L, Munck LK, et al: High mortality by natural and unnatural causes: a 10-year follow-up study of patients admitted to a poisoning treatment center after suicide attempts. British Medical Journal 306:1637-1641, 1993Crossref, Medline, Google Scholar
8. Nordstrom P, Samuelsson M, Asberg M: Survival analysis of suicide risk after attempted suicide. Acta Psychiatrica Scandinavica 91:336-340, 1995Crossref, Medline, Google Scholar
9. Hawton K, Fagg J: Suicide and other causes of death following attempted suicide. British Journal of Psychiatry 152:259-266, 1988Google Scholar
10. Schmidtke A: Perspective: suicide in Europe. Suicide and Life-Threatening Behavior 27:127-134, 1997Medline, Google Scholar
11. Ostamo A, Lonnqvist J, Heinonen S, et al: Epidemiology of parasuicides in Finland. Psychiatria Fennica 22:181-189, 1991Google Scholar
12. Hawton K, Arensman E, Wasserman D, et al: Relation between attempted suicide and suicide rates among young people in Europe. Journal of Epidemiology and Community Health 52:191-194, 1998Crossref, Medline, Google Scholar
13. Sapien RE, Fullerton L, Olson LM, et al: Disturbing trends: the epidemiology of pediatric emergency medical services use. Academic Emergency Medicine 6:232-238, 1999Crossref, Medline, Google Scholar
14. D'Mello DA, Finkbeiner DS, Kocher KN: The cost of antidepressant overdose. General Hospital Psychiatry 17:454-455, 1995Crossref, Medline, Google Scholar
15. Rice DP, MacKenzie EJ, Jones AS: Cost of Injury in the United States: A Report to Congress. San Francisco, Institute for Health and Aging, University of California; and Injury Prevention Center, Johns Hopkins University, 1989Google Scholar
16. Velamoor VR, Cernovsky ZZ: Suicide with the motive "to die" or "not to die" and its socioanamnestic correlates. Social Behavior and Personality 20:193-198, 1992Crossref, Google Scholar
17. Brent DA: Correlates of the medical lethality of suicide attempts in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 26:87-91, 1987Crossref, Medline, Google Scholar
18. Lewinsohn PM, Ronde P, Seely JR: Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice 3:25-46, 1996Crossref, Google Scholar
19. Kessler RC, Borges G, Walters EE: Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Study. Archives of General Psychiatry 56:617-626, 1999Crossref, Medline, Google Scholar
20. Hjelmeland H: Repetition of parasuicide: a predictive study. Suicide and Life-Threatening Behavior 26:395-404, 1996Medline, Google Scholar
21. Pierce D: Suicidal intent and repeated self-harm. Psychological Medicine 14:655-659, 1984Crossref, Medline, Google Scholar
22. Platt S, Bille-Brahe U, Kerkhof A, et al: Parasuicide in Europe: the WHO/EURO Multicentre Study on Parasuicide: I. introduction and preliminary analysis for 1989. Acta Psychiatrica Scandinavica 85:97-104, 1992Crossref, Medline, Google Scholar
23. Linehan MM, Heard HL, Wagner AW, et al: Parasuicide history interview: development of validity and reliability. Unpublished manuscript. Department of Psychology, University of Washington, Seattle, 1997Google Scholar
24. Kreitman N (ed): Parasuicide. London, Wiley, 1977Google Scholar
25. Bille-Brahe U, Schmidtke A, Kerkhof AJ, et al: Background and introduction to the WHO/EURO Multicentre Study on Parasuicide. Crisis 16(2):72-76, 1992Google Scholar
26. Bille-Brahe U, Kerkhof A, De Leo D, et al: A repetition-prediction study of European parasuicide populations: a summary of the first report from part II of the WHO/ EURO Multicentre Study on Parasuicide in co-operation with the EC concerted action on attempted suicide. Acta Psychiatrica Scandinavica 95:81-86, 1997Crossref, Medline, Google Scholar
27. Moscicki EK, O'Carroll P, Rae DS, et al: Suicide attempts in the Epidemiologic Catchment Area Study. Yale Journal of Biological Medicine 61:259-268, 1988Medline, Google Scholar
28. Rossow I, Wichstrom L: Parasuicide and use of intoxicants among Norwegian adolescents. Suicide and Life-Threatening Behavior 24:174-183, 1994Medline, Google Scholar
29. Weissman MM, Bland RC, Canino GJ, et al: Prevalence of suicide ideation and suicide attempts in nine countries. Psychological Medicine 29:9-17, 1999Crossref, Medline, Google Scholar
30. Gunnell DJ, Brooks J, Peters TJ: Epidemiology and patterns of hospital use after parasuicide in the southwest of England. Journal of Epidemiology and Community Health 50:24-29, 1996Crossref, Medline, Google Scholar
31. Van Egmund M, Diekstra RFW: The predictability of suicidal behavior: the results of a meta-analysis of published studies, in Suicide Prevention: The Role of Attitude and Imitation. Edited by Diekstra RFW, Maris RA, Platt S, et al: Leiden, the Netherlands, Brill, 1989Google Scholar
32. Simon GE, VonKorff M: Suicide mortality among patients treated for depression in an insured population. American Journal of Epidemiology 147:155-160, 1988Crossref, Google Scholar
33. Meehan PJ, Lamb JA, Saltzman LE, et al: Attempted suicide among young adults: progress toward a meaningful estimate of prevalence. American Journal of Psychiatry 149:41-44, 1992Link, Google Scholar
34. Larsson B, Ivarsson T: Clinical characteristics of adolescent psychiatric inpatients who have attempted suicide. European Child Adolescent Psychiatry 7:201-208, 1998Crossref, Medline, Google Scholar
35. Schmidtke A, Bille-Brahe U, De Leo D, et al: Attempted suicide in Europe: rates, trends, and sociodemographic characteristics of suicide attempters during the period 1989-1992: results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatrica Scandinavica 93:327-338, 1996Crossref, Medline, Google Scholar
36. Platt S, Hawton K, Kreitman N, et al: Recent clinical and epidemiological trends in parasuicide in Edinburgh and Oxford: a tale of two cities. Psychological Medicine 18:405-418, 1988Crossref, Medline, Google Scholar
37. Van Casteren V, Van der Veken J, Tafforeau J, et al: Suicide and attempted suicide reported by general practitioners in Belgium. Acta Psychiatrica Scandinavica 87:451-455, 1993Crossref, Medline, Google Scholar
38. Bland RC, Newman SC, Dyck RJ: The epidemiology of parasuicide in Edmonton. Canadian Journal of Psychiatry 39:391-396, 1994Medline, Google Scholar
39. Tsoi WF, Kua EH: Suicide following parasuicide in Singapore. British Journal of Psychiatry 151:543-545, 1987Crossref, Medline, Google Scholar
40. Dieserud G, Loeb M, Ekeberg O: Suicidal behavior in the municipality of Baerum, Norway: a 12-year prospective study of parasuicide and suicide. Suicide and Life-Threatening Behavior 30:61-73, 2000Medline, Google Scholar
41. Wai BHK, Heok KE: Parasuicide: a Singapore perspective. Ethnicity and Health 3:255-263, 1998Crossref, Medline, Google Scholar
42. Odejide AO, Williams AO, Ohaeri JU, et al: The epidemiology of deliberate self-harm: the Ibadan experience. British Journal of Psychiatry 149:734-737, 1986Crossref, Medline, Google Scholar
43. Briere J, Gil E: Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. American Journal of Orthopsychiatry 68:609-620, 1998Crossref, Medline, Google Scholar
44. Walsh BW, Rosen PM: Self-Mutilation: Theory, Research, and Treatment. New York, Guilford, 1988Google Scholar
45. Favazza AR, Conterio K: The plight of chronic self-mutilators. Community Mental Health Journal 24(1):22-30, 1988Google Scholar
46. Crosby AE, Cheltenham MP, Sacks JJ: Incidence of suicidal ideation and behavior in the United States, 1994. Suicide and Life-Threatening Behavior 29:131-140, 1999Medline, Google Scholar
47. Kebede D, Alem A: Suicide attempts and ideation among adults in Addis Ababa, Ethiopia. Acta Psychiatrica Scandinavica 100:35-39, 1999Crossref, Google Scholar
48. Van Herringen K: Epidemiological aspects of attempted suicide: a case control study in Gent, Belgium. Crisis 15(3):116-121, 1994Google Scholar
49. Petronis KR, Samuels JF, Moscicki EK, et al: An epidemiologic investigation of potential risk factors for suicide attempts. Social Psychiatry and Psychiatric Epidemiology 25:193-199, 1990Medline, Google Scholar
50. Hawton K, Fagg J, Simkin S, et al: The epidemiology of attempted suicide in the Oxford area, England (1989-1992). Crisis 15(3):123-135, 1994Google Scholar
51. Bancroft J, Skrimshire A, Casson J, et al: People who deliberately poison or injure themselves: their problems and their contacts with helping agencies. Psychological Medicine 7:289-303, 1977Crossref, Medline, Google Scholar
52. Appleby L, Turnbull G: Parasuicide in the first postnatal year. Psychological Medicine 25:1087-1090, 1995Crossref, Medline, Google Scholar
53. Linehan MM, Goodstein JL, Neilsen SL, et al: Reasons for staying alive when you are thinking of killing yourself: the Reasons for Living Inventory. Journal of Consulting and Clinical Psychology 51:276-286, 1983Crossref, Medline, Google Scholar
54. Platt S: Unemployment and suicidal behavior: a review of the literature. Social Science Medicine 19:93-115, 1984Crossref, Medline, Google Scholar
55. Platt S, Kreitman N: Long-term trends in parasuicide and unemployment in Edinburgh, 1968-87. Social Psychiatry and Psychiatric Epidemiology 25:56-61, 1990Medline, Google Scholar
56. Platt S, Kreitman N: Trends in parasuicide and unemployment among men in Edinburgh, 1968-82. British Medical Journal (Clinical Research Edition) 289:1029-1032, 1984Crossref, Medline, Google Scholar
57. Neeleman J, Jones P, Van Os J, et al: Parasuicide in Camberwell: ethic differences. Social Psychiatry and Psychiatric Epidemiology 31:284-287, 1996Crossref, Medline, Google Scholar
58. Platt S, Dyer JAT: Psychological correlates of unemployment among male parasuicides in Edinburgh. British Journal of Psychiatry 151:27-32, 1987Crossref, Medline, Google Scholar
59. Suominen K, Henriksson M, Suokas J, et al: Mental disorders and comorbidity in attempted suicide. Acta Psychiatrica Scandinavica 94:234-240, 1996Crossref, Medline, Google Scholar
60. Pfeffer CR, Klerman GL, Hurt SW, et al: Suicidal children grow up: rates and psychosocial risk factors for suicide attempts during follow-up. Journal of the American Academy of Child and Adolescent Psychiatry 32:106-113, 1993Crossref, Medline, Google Scholar
61. Neeleman J, Power MJ: Social support and depression in three groups of psychiatric patients and a group of medical controls. Social Psychiatry and Psychiatric Epidemiology 29:46-51, 1994Medline, Google Scholar
62. Weissman MM, Gerald LK, Markowitz JS, et al: Suicidal ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine 321:1209-1214, 1989Crossref, Medline, Google Scholar
63. Rudd M, Joiner T, Rajab M: Relationships among suicide ideators, attempters, and multiple attempters in a young-adult sample. Journal of Abnormal Psychology 105:541-550, 1996Crossref, Medline, Google Scholar
64. Garrison CZ, McKeown RE, Valois RF, et al: Aggression, substance use, and suicidal behaviors in high school students. American Journal of Public Health 83:179-184, 1993Crossref, Medline, Google Scholar
65. Hawton K, Fagg J, Simkin S, et al: Attempted suicide in Oxford. Cited in Williams M: Cry of Pain: Understanding Suicide and Self-Harm. London, Penguin, 1997Google Scholar
66. Ndosi NK, Waziri MC: The nature of parasuicide in Dar es Salaam, Tanzania. Social Science Medicine 44:55-61, 1997Crossref, Google Scholar
67. Hjelmeland H, Bjerke T: Parasuicide in the county of Sor-Trondelag, Norway: general epidemiology and psychological factors. Social Psychiatry and Psychiatric Epidemiology 31:272-283, 1996Medline, Google Scholar
68. Diekstra RF: The epidemiology of suicide and parasuicide. Acta Psychiatrica Scandinavica 87:9-20, 1993Crossref, Google Scholar
69. Kreitman N: Suicide, age, and marital status. Psychological Medicine 18:175-190, 1988Crossref, Google Scholar
70. Hintikka J, Viinamaki H, Tanskanen A, et al: Suicidal ideation and parasuicide in the Finnish general population. Acta Psychiatrica Scandinavica 98:23-27, 1998Crossref, Medline, Google Scholar
71. Druss B, Pincus H: Suicidal ideation and suicide attempts in general medical illnesses. Archives of Internal Medicine 160:1522-1526, 2000Crossref, Medline, Google Scholar
72. Kjoller M, Helweg-Larsen M: Suicidal ideation and suicide attempts among adult Danes. Scandinavian Journal of Public Health 28:54-61, 2000Crossref, Medline, Google Scholar
73. Alem A, Kebede D, Jacogsson L, et al: Suicide attempts among adults in Butajira, Ethopia. Acta Psychiatrica Scandinavica 100:70-76, 1999Crossref, Google Scholar
74. Pirkis J, Burgess P, Dunt D: Suicidal ideation and suicide attempts among Australian adults. Crisis 21(1):16-25, 2000Google Scholar



